General information
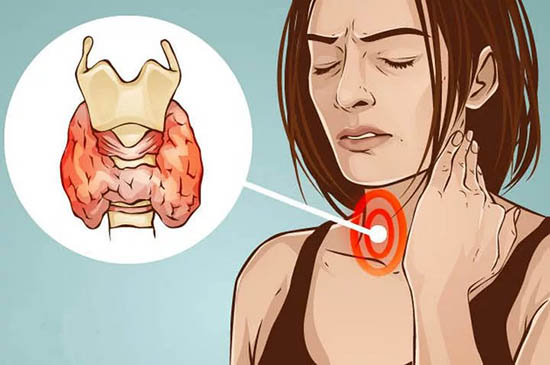
Thyroglobulin (TG) is a prohormone - a precursor of hormones, a large glycoprotein, which is the starting “material” in the process of formation of the thyroid hormones thyroxine (T4) and triiodothyronine (T3). The thyroid gland is the only organ in the body that produces TG. It is produced by cells of a healthy thyroid gland, as well as cells of highly differentiated malignant tumors localized in its tissues (adenocarcinoma, papillary and follicular).
In the presence of endocrine pathologies or other autoimmune abnormalities in the body, intensive production of antibodies (AB) to this hormone begins, which leads to disruption of the planned production of T3 and T4.
AT-TG can reduce the synthesis of thyroid hormones and cause hypothyroidism or, conversely, overstimulate the gland, causing its hyperfunction.
The test for antibodies to thyroglobulin (AT-TG) allows you to identify autoimmune thyroid diseases in a patient and promptly begin hormone replacement therapy, which is also aimed at suppressing the activity of antibodies.
Rules for donating blood and interpretation of test results for thyroglobulin levels
After removal of the thyroid gland, an analysis of the concentration of thyroglobulin in the blood is recommended only after 3 months after surgery or 6 months if a course of treatment with radioactive iodine was carried out.
Taking the test before these dates will not give a real picture and may show a false increase in thyroglobulin levels, which in turn makes one think about a recurrence of cancer.
In a situation where antibodies to thyroglobulin are highly elevated in the body, an analysis for thyroglobulin itself will not be of any value, since the antibodies will kill protein molecules and its concentration will not be significant.
An analysis of venous blood for TG, done against the background of a 3-week withdrawal from taking a thyroxine-based drug, is the most accurate marker of the reappearance of malignant neoplasms (carried out only in the absence of elevated antibodies to the glycoprotein).
In most cases, it is more important to see the dynamics of changes in thyroglobulin concentration than its value itself. This means that even with its increased level, treatment can be considered successful if there is a positive dynamics of its decline
This means that even with its elevated level, treatment can be considered successful if there is a positive trend in its decline.
Indications
The AT-TG marker allows you to identify autoimmune lesions of the thyroid gland (Hashimoto's disease, diffuse toxic goiter, atrophic autoimmune thyroiditis, etc.). The analysis is also used for the differential diagnosis of endocrine pathologies in iodine-deficient areas and the treatment of children born to mothers with an increased concentration of antibodies to TG. In addition, testing for AT-TG is necessary to monitor the rehabilitation of patients with thyroid cancer. In this case, the purpose of testing is to prevent disease relapse and metastasis.
According to the statistics of AT to TG, the following are determined:
- 40-70% of cases in patients with chronic thyroiditis (inflammation of the thyroid gland);
- 70% - with hypothyroidism (lack of function);
- 35-40% for toxic goiter (increase in size and change in the functional state of the gland);
- less often in other cases (including with pernicious anemia).
According to a 2012 study by the British Association of Dermatologists, patients with vitiligo have a higher risk of autoimmune thyroid disease. 9.7% of the examined people with vitiligo had antibodies to TG.
Antibody levels can also be elevated in healthy people (for example, in 10% of cases in menopausal women).
Indications for the purpose of analysis are as follows:
- changes in the size, shape, structure of the thyroid gland;
- blurred vision, ophthalmopathy;
- sudden weight loss or gain without objective reasons;
- rapid heartbeat (tachycardia) or arrhythmia;
- increased weakness and fatigue, decreased performance;
- monitoring the effectiveness of treatment with thyroglobulin after removal of a tumor on the gland;
- systemic autoimmune processes (to determine the risk of thyroid damage);
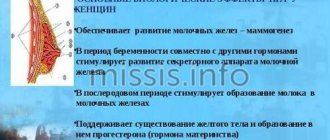
- problems in the reproductive sphere in women;
- dense swelling of the lower extremities, which may indicate pretibial myxedema;
- for differential diagnosis of toxic and non-toxic (for example, iodine deficiency) nodular goiter;
- monitoring the condition of pregnant patients if they have a history of autoimmune diseases (analysis is carried out upon registration and in the 3rd trimester of pregnancy);
- to determine risk groups for the development of thyroid diseases among children born to mothers with pathology of the endocrine organs.
Diagnostics and tests
It should be noted that many patients are wary of antibody tests. But do not be afraid of the purpose of this analysis. It can be prescribed not only for suspected cancer. Thyroid dysfunction can also occur for other reasons.
Testing for antibodies to TG is often prescribed for diseases of an autoimmune nature, i.e. for disorders of the human immune system. In such diseases, the body perceives its own tissues as foreign, resulting in their damage. An antibody test allows you to identify serious pathologies at the initial stage of their development.
Similar situations arise in the following violations:
- When controlling the processes occurring in the thyroid gland.
- For systematic pathologies of an autoimmune nature.
- If any violations are detected after injuries.
- In case of disruption of the reproductive system in women.
- To monitor the behavior of the body after surgical interventions.
Often, a test for antibodies to thyroglobulin is prescribed based on the patient’s verbal complaints.
Such complaints may include:
- Apathetic mood.
- Fatigue and weakness.
- Increase in neck volume.
- The appearance of rashes on the skin, its dryness.
- Noticeable bulging of the eyes.
- Insomnia.
- Increased irritability and anxiety.
- Memory problems.
- Cycle disturbances, miscarriages, infertility in women.
- Decrease/increase in body weight from normal.
Frequently, antibodies to thyroglobulin should be tested for the following diseases or suspicion of them:
- Tumor diseases or diseases of an oncological nature,
- Down syndrome disease,
- Thyroid diseases
- Hemolytic anemia,
- Hashimoto's thyroiditis,
- Diffuse or toxic goiter.
What are the rules for donating blood for analysis to detect antibodies to thyroglobulin?

To obtain a more accurate and reliable analysis result, a number of conditions must be met.
- Blood for analysis must be taken from the ulnar vein.
- Blood sampling must be done before 11 o'clock in the afternoon, i.e. in the first half of the day, since it is at this time that hormone levels peak.
- Blood must be donated on an empty stomach; only clean drinking water can be consumed.
- Smoking is strictly prohibited several hours before the test (including the use of nicotine substitutes).
- About a day before the analysis, physical activity and psychological stress should be excluded, i.e. it is necessary to ensure the patient's rest. Half an hour before the analysis should be spent in absolute peace.
- It is necessary to interrupt treatment if it is in progress. You should also temporarily stop taking certain medications that may distort the test result.
- The analysis should be carried out separately from other studies. It is not advisable to undergo ultrasound, MRI and other examinations on this day.
The test should be postponed for some time if the patient has recently suffered from an infectious disease with an increase in body temperature.
Also, if minor deviations from the norm are detected, the analysis should be repeated after 7-10 days in order to compile a complete and correct picture of the pathology and its origin.
Factors influencing the result
The patient should be careful when preparing for the test and be completely honest with their doctor. For example, if a woman hides the fact of taking oral contraceptives (birth control) from a specialist and does not cancel them, then the AT-TG result may be false-positive (unreliable).
Changes in the structure of thyroid tissue can also distort the result.
The absence of antibodies in the biomaterial may also be due to other pathological processes:
- the body produces antibodies to other antigens;
- Specific thyroglobulin-antibody immune complexes appeared.
Antibody synthesis can be limited by lymphocytes, which will also give negative test results.
Important! The interpretation of the results is always carried out comprehensively. It is impossible to make an accurate diagnosis based on only one analysis.
For what reasons may indicators be increased?
In some cases, an increase in antibodies to thyroglobulin may be due to the influence of external factors that affect hormonal levels.
The main factors that provoke intense protein release include the following:
- active production of hormones;
- the presence of inflammatory processes, mainly in the thyroid gland;
- long-term use of oral or combined contraceptives;
- an increase in the size of the thyroid gland.
These factors can lead to an intense increase in thyroglobulin protein, and this will lead to unpleasant consequences for the body.
Important! There are a number of diseases for which antibody analysis for thyroglobulin concentration is simply necessary. These include diabetes, diffuse toxic goiter, rheumatoid arthritis, hypothyroidism, nodular goiter, lupus erythematosus and others.
In all of these diseases, thyroglobulin is produced in increased quantities and is greatly elevated.
Hyperthyroidism, that is, increased functions of the thyroid gland, is described in the video:
AT-TG is higher than normal
Important! the presence of antibodies to thyroglobulin in the body of a pregnant woman increases the risk of thyroid dysfunction in the embryo and newborn.
When diagnosing pathologies, the number of antibodies does not provide complete information about the stage and severity of the disease.
Exceeding the antibody norm indicates the following pathologies:
- diffuse toxic goiter (Graves' disease, Graves' disease),
- granulomatous thyroiditis (non-purulent inflammation of the thyroid gland);
- Hashimoto's disease (chronic thyroiditis), especially in combination with elevated levels of AT-TPO;
- genetic pathologies that are accompanied by autoimmune thyroiditis (Klinefelter, Down, Shereshevsky-Turner syndrome);
- idiopathic myxedema (lack of thyroid hormones, which is manifested by changes in the structure of facial tissues and swelling);
- subacute and acute thyroiditis (inflammation of the thyroid gland);
- diabetes mellitus type 1 (insulin dependent);
- goiter (enlargement of the gland);
- primary hypothyroidism (reduction in the synthesis of endocrine hormones);
- malignant neoplasms in the tissues of the thyroid gland;
- other autoimmune pathologies: systemic lupus erythematosus (connective tissue damage);
- pernicious (B-12 deficient) or hemolytic anemia;
- Sjögren's disease (systemic connective tissue damage);
- myasthenia gravis (a disease of the neuromuscular system characterized by weakness and increased fatigue of striated muscles);
- rheumatoid arthritis, etc.
The interpretation of the results can be carried out by a qualified specialist - an endocrinologist, obstetrician-gynecologist, oncologist, pediatrician, etc.
What is thyroglobulin?
What is thyroglobulin? This is one of the variants of globulins that are present in the body.
Thyroglobulin is a protein iodine-containing biologically active compound that reflects the presence of thyroid cells in the human body.
It is produced and accumulates exclusively in the follicular cells of the thyroid gland. The main thyroid hormones, T4 (thyroxine) and T3 (triiodothyronine), are formed from thyroglobulin.
The TG concentration in the blood is directly dependent on the mass of the gland and therefore can be considered a reliable indicator of its condition.
When the blood test for TSH is higher than normal, then with a high degree of probability it is possible to suspect the occurrence of tumor processes in the thyroid gland or its inflammation.
Important! The iodine-containing protein thyroglobulin is not a tumor marker for the unremoved thyroid gland. However, its inflated indicators may indicate an increased risk of oncological processes in the organ.

Thyroglobulin can be considered a tumor marker only if its concentrations are studied after removal of the thyroid gland.
If the thyroid gland is removed, such a blood test is required approximately once every 4 months. This allows you to diagnose a possible relapse at an early stage.
And in the presence of thyroid gland, a blood TG test to determine the primary tumor is meaningless.
AT standards for rTSH in various laboratories
*It should be immediately noted that the difference in reference values is due to insufficient standardization and the use of different methods in laboratories.
The following reference values have been established for both women and men:
- Negative: 1.0 U/l
- Doubtful: 1.1-1.5 U/l
- Positive: 1.5 U/l
Reference values in the Invitro laboratory:
- less than 1.0 – negative;
- greater than or equal to 1.0 – positive
Standards in the Helix laboratory
- less than 1.75 IU/l - negative
- more than 1.75 IU/l - positive
Note:
the result of the study is assessed in conjunction with additional clinical, laboratory and instrumental tests. If a negative answer is received, the presence of the disease cannot be completely ruled out.
How can elevated levels be dangerous?
An analysis for an increased amount of antibodies to thyroglobulin is used in the early stages of any disease, when other methods are powerless. If antibodies to thyroglobulin exceed the norm, this may mean the presence of certain pathological diseases occurring in the body.
These include:
- inflammation of the thyroid gland;
- malignant thyroid tumors;
- benign adenomas;
- the body's reaction to damage to the thyroid gland;
- decreased production of thyroid hormones;
- chronic thyroiditis.
Quite often, pernicious anemia, thyroid surgery, or some genetic disease contributes to an increase in antibodies.
In addition, a woman's age may be a potential reason for the increase in the rate. Men suffer from this pathology much less frequently than women. You should also take into account recent illnesses or treatment of a disease that has not been completed.
Indications for the study
An endocrinologist deals with the diagnosis and treatment of disorders in the functioning of the thyroid gland. The specialist, taking into account the patient’s complaints, prescribes a medical examination and, based on the results obtained, selects the most effective treatment.
Complex diagnostics is indicated for patients in the following situations:
- a person is worried about weakness and increased fatigue, performance decreases;
- there is apathy towards the surrounding world;
- there is irritability, anxiety, tearfulness;
- disturbed sleep and insomnia;
- lower limbs swell;
- the neck is increased in volume;
- rashes appear on the skin, it becomes dry;
- memory and visual functions are impaired;
- there are problems with reproductive function;
- body weight is noticeably reduced.
An examination is necessary if there is a rapid heartbeat or the presence of arrhythmia. All these clinical signs should alert a person and force them to go to the hospital for diagnosis. Assessing the functioning of the thyroid gland is also necessary to monitor how to proceed with therapy after removal of a tumor on the organ.
Thyroid diseases: 5 tips
Since we're talking about the thyroid gland, I'll take this opportunity to give a few more important recommendations.
Ultrasound does not provide insight into how the thyroid gland works
- Most regions of Russia are in the zone of iodine deficiency. Buy only iodized salt and use it instead of regular salt.
- Sea kale does not contain as much iodine as is commonly believed. You can use seaweed to make salads if you like, but this does not mean at all that you can abandon traditional methods of iodine prophylaxis (iodized salt or pharmacological doses of iodine for pregnant women).
- You cannot use an alcohol solution of iodine for “prevention and treatment of the thyroid gland,” as is sometimes recommended in TV shows and pseudoscientific books about health. “Iodine nets,” a solution of iodine in sugar or milk, can quickly lead to the accumulation of toxic doses of iodine in the thyroid gland and the development of thyrotoxicosis.
- There is no need to do an ultrasound of the thyroid gland just in case. If the function of the thyroid gland is not impaired, and the gland itself is not enlarged and no formations are palpable in it, then an ultrasound “just in case” will do more harm than good. Detection of small nodular formations, fear of detecting cancer, unjustified repeated punctures, repeated ultrasounds - this is what awaits a person who has set foot on this slippery path of multiple unnecessary examinations.
- A healthy adult needs to have their TSH level determined once every 5 years. If you have previously been diagnosed with subclinical hypothyroidism, subclinical thyrotoxicosis, or if you are taking the antiarrhythmic drug amiodarone, then take a TSH blood test once every 6 months.
When to see a doctor
Progressive pathological processes provoke degeneration of thyroid tissue. A timely visit to a specialist will prevent complications, reduce the risk of relapse if it is cancer, and reduce the amount of surgical intervention.
An endocrinologist should be visited when the first disturbances and signs of a pathological condition appear. Taking into account the results of the examination and the cause of the problems, you may additionally need to consult other specialized specialists (oncologist, obstetrician-gynecologist, surgeon, therapist).
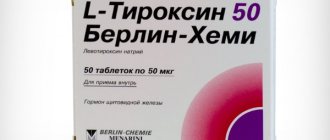
Treatment of hypothyroidism and thyrotoxicosis
Overt hypothyroidism should always be treated. You will be prescribed thyroid hormone replacement therapy, levothyroxine, which you will need to take for life.
Subclinical hypothyroidism in most cases does not require treatment; tests must be repeated after 3–6 months. The exception is pregnancy, as well as a pronounced increase in cholesterol (> 7 mmol/l). In these cases, even with subclinical hypothyroidism, thyroxine replacement therapy is prescribed.
Manifest (overt) thyrotoxicosis almost always requires treatment. At first I wrote “always,” then, to be fair, I decided to add that there are rare forms that go away on their own. However, thyrotoxicosis always requires consultation with a doctor and observation.
Subclinical thyrotoxicosis does not require treatment, but tests must be repeated after 6 months, there is a possibility of transition to an expanded form.