Among the most complex biochemical tests, through which the condition of children is diagnosed and the need for treatment is determined, is stool examination. Leukocytes in a child's stool are allowed only up to 3 months, when the intestines are formed. For each age category there is a certain leukocyte count:
- From 6*109/l to 7.5*109/l, if the child’s age is 13 - 16 years.
- 8*109/l for children 7 - 12 years old.
- 8*109/l – 10*109/l for children from 2 to 6 years old.
- 10*109/l is the norm for a one-year-old baby.
- 11*109/l, if the baby is six months old.
- 12*109/l in a one-month-old baby.
- 15*109/l, if the baby is a newborn.
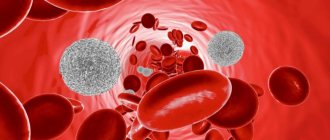
However, the number of leukocytes in the analysis does not always correspond to the norm. Sometimes the level rises and neutrophils penetrate into the baby's stool.
Advice! Even with an elevated white blood cell count, some children feel normal. But parents should pay attention to the excess of neutrophils, because this is an indicator of the body’s fight against infection or a signal of an inflammatory process.
Why do children's stool contain leukocytes?
To protect against infections, the body produces white blood cells. Moreover, with increasing age, the norm of indicators decreases. So, in a child aged 14 - 16 years, the normal level of neutrophils is 7.5 * 109 / l, and in an infant - 15 * 109 / l. The newborn’s body more actively fights infectious diseases.
The leukocyte level does not increase without a reason. A newborn's stool is sterile and olive-colored. Then parents notice a change in the color of the stool. There is no cause for concern as the bowel movements will continue to be greenish-brown until the baby is 2 weeks old. During this period, the baby's stool is formed. For children aged 1 year and older, it is formalized.
But if there is a serious excess of leukocytes in the stool, or the appearance of an uncharacteristic smell or color of the stool, you should contact your pediatrician. Perhaps this condition was caused by infectious diseases. To identify and eliminate the causes that provoked this condition, a high-quality diagnosis is required, on the basis of which the doctor will refer you to the right specialist. Most often, a consultation with a pediatric gastroenterologist is needed, who will then determine the appropriate treatment.
Diagnosis and signs of elevated white blood cell levels
Correct treatment is carried out only after performing a detailed qualitative analysis. Using this diagnostic method, the enzyme state, the number of leukocytes, and the presence of a pathological process in the body are determined. Such research in the laboratory is called scatology, and the feces themselves are called coprograms.
Based on scatological data, a doctor can diagnose a child with:
- diseases of the digestive system;
- ailments of the small and large intestines;
- giardiasis;
- presence of helminths.
Often, a pronounced increase in white blood cell counts is accompanied by diarrhea and other symptoms. During this period, children lose a lot of fluid. For some, mucus and even pinkish discharge are visualized in the coprogram. This condition requires urgent treatment, because mucus in the stool can signal a dangerous disease.
Do you know whether your baby needs an analysis of the number of lymphocytes in the blood? We advise you to familiarize yourself with the material.
Diagnosis of leukocytes and mucus in infant stool
If mucus is detected in the stool in children, they are diagnosed with:
- Dysentery. An increased number of neutrophils is often a symptom.
- Spastic colitis. Pronounced symptoms of the disease are poorly digested fiber and an increased number of white blood cells.
- Ulcerative colitis. With it, inflammation spreads only to the large intestine. The newborn develops diarrhea, and in an advanced state, ulcerative colitis leads to intestinal perforation, acute toxic dilatation, sphincter weakness, accompanied by fecal and gas incontinence, and even colon cancer.
- Follicular enteritis. The coprogram contains mucus in the form of lumps.
- Dysbacteriosis. Often accompanied by E. coli or parasites in the newborn’s intestines.
Normal coprogram indicators
Sometimes white blood cells in the stool in children occur after long-term treatment with antibiotics or other medications. In this case, the problem is eliminated after eliminating or replacing the drug. The norm is also exceeded in case of prolonged diarrhea. Moreover, this factor is observed not only in infants, but also in children over 8 years of age. Parents may not worry too much about their children's health if they:
- are not capricious;
- active and cheerful;
- do not experience abdominal cramps or allergic reactions;
- feel good;
- eat with gusto.
But the occurrence of opposite signs is a cause for serious concern.
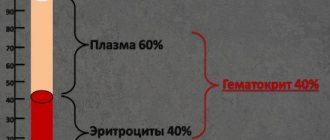
With constipation in children, there is also an increased content of leukocytes in the coprogram. The same state of the internal nodes of the intestinal veins is signaled by red blood cells in the feces. These blood cells, whose main function is to transport oxygen throughout the body, should not be present in large quantities in the stool. Their abundance in the coprogram indicates bleeding in the intestines or anal fissure. Also, these bodies appear in the coprogram due to improper sampling or placement of the material in a non-sterile container.
The permissible norm for children from 2 to 12 years is from 8 to 109/l; a newborn has more of these bodies in the feces (as well as red blood cells and hemoglobin in the blood) than older children. Of course, the norm may be slightly exceeded if the baby has recently been ill, is not eating properly or is nervous. Stress in a child occurs due to teething, fear, tense family situations, difficulties at school, etc. When teething, parents often notice changes in stool, increased irritability of the baby and drooling. But most often, a lot of leukocytes in feces is a signal of disease.
Reasons for development
Each child has individual characteristics of the body. With age, not only the nature, but also the frequency of bowel movements changes. A baby's stool may contain leukocytes if it has an unpleasant odor. Parents should also analyze consistency. If there are negative manifestations, the presence of an inflammatory process or infection can be suspected.
Leukocytes can be detected in the stool of children in the presence of the following diseases:
We recommend reading: Green stool in a baby
- Large lumps of mucus are fixed in the case of follicular enteritis.
- Additionally, rods and cocci are present in the feces in acute colitis.
- Thanks to this analysis, it is possible to diagnose allergic and ulcerative colitis, constipation, and dysentery.
If there are a lot of leukocytes in the stool, then parents should not panic. This indicator does not yet indicate the presence of serious diseases. If the manifestation of other symptoms is not recorded, then the presence of a serious illness should not be suspected.
The conclusion about the patient’s condition and the need for treatment is determined only by the doctor.
White blood cells are present in stool in the following cases:
- The presence of infections in the stomach and intestines.
- An active inflammatory process in the small intestine.
- A young patient regularly experiences constipation or dysbacteriosis.
- Severe intoxication of the body.
- One of the types of colitis was previously diagnosed.
- Inflammatory process in the rectum.
- The analysis was carried out incorrectly due to improper collection of materials.
- The baby is not eating well or is constantly under extreme stress.
Treatment for infants is prescribed in the case of an inflammatory process in the small or large intestine. However, the situation with an increase in the level of leukocytes is observed against the background of the influence of the following factors:
- Immediately after birth, the baby’s digestive system is still at the stage of formation. It does not contain enough enzymes. Taking medications can have a negative impact on the situation.
- Mommy does not adhere to the diet prescribed during lactation. It is recommended to refrain from prohibited foods immediately before taking tests. Otherwise, the result may be greatly distorted.
- For a child under one year old, weight gain is an important indicator. In case of deviation from the norm, it is imperative to check the number of leukocytes in the stool. You should be concerned if the baby also experiences colic, tearfulness, and irritation. The situation can become very aggravated during defecation. In this case, leukocytes in the stool indicate the presence of an inflammatory process in the gastrointestinal tract.
- Additionally, it should be noted that the number of leukocytes in the stool of children on artificial and natural feeding options is very different. The situation changes if complementary foods are introduced into the diet. As a rule, the number of white blood cells in the stool decreases.
It is easy to make the correct diagnosis based on the number of leukocytes in the stool. Cells are observed in increased numbers in the presence of inflammation. If the indicator was recorded in this form, then a number of additional tests will be required. Based on their results, a diagnosis will be made. The child’s behavior and complaints are taken into account. Additionally, stool disturbances, loss of appetite and general weakness can be recorded.
Why does the number of leukocytes increase in a baby?
A child’s white blood cell count does not always increase due to infection. Sometimes this happens when:
- Poor weight gain. Leukocytes in the stool of an infant can be observed even with a healthy set, but this does not indicate the presence of pathologies. But when a baby does not gain weight well, experiences colic and often cries during bowel movements, most likely he has problems with the gastrointestinal tract.
- Impaired digestion. An immature gastrointestinal tract does not produce enough enzymes. Or it functions poorly due to long-term antibiotic therapy. Then mucus may appear in the stool.
- A certain type of nutrition. Pediatricians have noticed that in infants fed artificial formula, immune cells are less often detected than in children fed breast milk.
- The mother's consumption of allergenic foods. This could be chocolate, strawberries, eggs, fried, fatty or smoked foods. These products can cause changes in the baby's stool.
Treatment
There is no need to use drug treatment if the baby does not have additional symptoms or complaints from the parents. If there are a lot of leukocytes in the stool, then it is necessary to carefully monitor changes in the condition. Depending on the test results, the doctor will prescribe the necessary therapy:
- To normalize and restore intestinal microflora, it is advisable to use probiotics. The pharmacy offers a wide range of drugs in this group. The choice of one of them directly depends on the individual characteristics of the baby’s body.
- It is necessary to carefully analyze the diet. It should have the perfect balance of vitamins and minerals. Otherwise, the risk of microflora disruption increases. The child must receive sufficient amounts of fluid. Thanks to it, vitamins, minerals and trace elements are absorbed. To obtain correct test results, you should adhere to a special diet before taking the test. Otherwise, stool collection is considered inappropriate.
- The number of leukocytes is not a constant value. It can change during the day and depending on food. The emotional state of the baby and regular physical activity are of no small importance. If a large number of white blood cells were detected in the stool, the test will need to be repeated. Thanks to this, it will be possible to make the correct diagnosis.
Examinations must be completed if the baby feels unwell. Tests will help determine the presence of gastrointestinal diseases. In the future, their treatment will be carried out by a gastroenterologist. A large number of leukocytes in the stool is also observed in case of infection. In this case, it is advisable to use drugs against broad-spectrum microbes.
If the baby does not have other symptoms, then treatment may not be required. It is necessary to pay close attention to his well-being and monitor changes in him. Drug treatment is required in case of intestinal microflora disturbance.
Studying coprogram with test strips
If a mother has doubts about the condition of her child’s intestines, she can purchase special tests to study the coprogram. A coprogram is done at any time of the day, and then, using such rapid tests, the presence or absence of leukocytes, the level of bilirubin, protein, the presence of blood and the pH reaction are determined.
Some test strips do not detect the presence of leukocytes in stool, so it is better to purchase multifunctional ones of the OctaFan type. Before analysis, prepare a fecal emulsion by diluting the feces with saline or distilled water to a slightly runny consistency. After thorough mixing, feces is applied to a corner of the reagent field and the reaction of the test is monitored. The final color of the reagent zone is compared with the color indicated on the container scale.
Test strips are used to analyze the child’s coprogram for:
- Alkali. The reaction of the coprogram should be slightly alkaline or neutral. An acidic reaction signals digestive disorders, including colitis or dysbacteriosis. With these ailments, leukocytes are often detected in the stool.
- Protein. Its presence in stool indicates damage to the stomach, duodenum, rectum or colon.
- Hemoglobin. Sometimes these tests visualize “occult blood” that was not recognized by macroscopic analysis.
- Urobilinogen and stercobilin. Often observed with dysbacteriosis and pancreatitis.
- Bilirubin. For children under 3 months of age, its presence is considered normal, since during this period a healthy bacterial flora of the gastrointestinal tract is formed. In older children, its presence signals a severe gastrointestinal pathology: severe dysbiosis or rapid food evacuation through the intestines.
- Leukocytes. Their presence indicates inflammatory processes in the large, small or duodenal intestine. The test can easily determine the intensity of the reaction. If the diagnostic zone has not changed color, the reaction to leukocytes is negative. A low neutrophil count is expressed in a lilac color. But the rich lilac color shows a pronounced reaction to neutrophils. If too many leukocytes are found in the coprogram, a re-examination is required. This is due to a possible psychological disorder of the baby or high physical activity, due to which the test determined the presence of leukocytes in the stool.
Diagnostic test strips for stool examination
Test strips are used at home. To do this, according to the instructions, you must first prepare the required consistency of stool. Express tests allow you to track the dynamics of the inflammatory process or, conversely, remove suspicion of any diagnosis in your baby. You can also do a stool test at different times of the day, which will allow you to see when there are more leukocytes and when there are fewer. Using a chemical test of stool at home, you can determine not only the level of immune cells, but also bilirubin, urobilinogen, blood, protein, and pH reaction.
Diet before taking the test
Regardless of which method the study will be carried out, you should prepare for it by following a diet. Doctors recommend 2 types of diets:
- According to Pevzner. This Soviet doctor developed a number of diets for the treatment of gastrointestinal diseases and the rehabilitation of those who had cholecystitis and hepatitis. During the diet, the child is fed potatoes, butter, vegetables, vegetable soups, buckwheat and rice porridge, sauerkraut and apples. To improve intestinal motility, crumbs exclude meat, fish and confectionery products from the menu.
- According to Schmidt. The menu includes milk oatmeal, potatoes, eggs, milk and butter. This diet is also prescribed before coprology to check for bleeding. Then the child’s menu should not contain green vegetables, tomatoes, fish and meat.
Parents should also take into account that some medications can distort the results of coprograms. This issue should be discussed with the treating pediatrician or pediatric gastroenterologist before the analysis.
How to lower the level of leukocytes in a coprogram
Treatment for excess white blood cells involves eliminating the cause and lowering the white blood cell level. The child must be shown to a doctor if the following symptoms occur:
- frequent fatigue and drowsiness;
- general malaise;
- increased body temperature;
- urination less often than usual with an uncharacteristic odor and color;
- quiet crying, with almost no visible tears;
- dry mouth;
- frequent diarrhea with a strong odor;
- vomit.
If a child experiences such signs, immediate consultation with a doctor is required. This is associated with an increased risk of dehydration and even death!
By contacting a doctor in a timely manner, taking tests and immediately starting to treat the child, parents increase the chances of a good prognosis for the disease and rapid recovery of the baby’s body. The doctor prescribes treatment with Lactazar, Acipol, Bifidumbacterin, Linex or other drugs. It is only allowed for children over 3 years of age and adults - infants have hearing problems.
It is also impossible to treat with prescribed medications for too long - dysbacteriosis may occur. But you cannot prescribe or cancel medications on your own - such actions are performed only under the close supervision of a doctor. Incorrect treatment can only make the situation worse.
0 0 votes
Article rating
Causes of diarrhea in a child
The acute process is often infectious in nature, especially if it occurs suddenly or is combined with vomiting, blood, fever and anorexia. Maintenance treatment is prescribed based on clinical diagnosis and continues until improvement occurs.
Chronic diarrhea in a child without fever can develop due to the following reasons:
- Allergic gastroenteropathy. Cow's milk protein causes bloody diarrhea and vomiting. The condition is normalized when hydrolyzed protein is included in the diet instead of cow's milk. Most children improve spontaneously.
- Disaccharidase deficiency. It is characterized by the absence of lactase, which breaks down lactose into galactose and glucose. The disorder may be congenital or develop after a gastrointestinal infection, acting as a temporary disorder. An improvement in the condition after eliminating lactose or other carbohydrates from the diet confirms the diagnosis. In this case, the child has light diarrhea and there is severe irritation in the perineal area caused by liquid feces.
- Gluten enteropathy (celiac disease). In celiac disease, the wheat protein fraction damages the intestinal mucosa, which can impair fat absorption. This leads to malabsorption and anorexia, which is accompanied by the passage of copious amounts of stool. Changes in the body occur when consuming products made from wheat flour and dishes containing gluten.
- Cystic fibrosis. Cystic fibrosis is characterized by the development of pancreatic insufficiency, which is accompanied by a deficiency of trypsin and lipase. In this case, there is a large loss of fat and protein in the stool, which means that physical development is delayed. The stool is usually smelly. Children with cystic fibrosis often develop respiratory problems.
Inflammatory processes in the intestines and some infections can also cause diarrhea. The most common is gastroenteritis, an infection of the small intestine that is accompanied by vomiting. The main danger of this disease is dehydration and water-electrolyte imbalance. Dehydration develops especially often and quickly against the background of rotavirus infection.
The causes of secretory diarrhea in a child are usually due to infection:
- bacterial (staphylococcus, salmonella, E. coli, shigella);
- parasitic (giardiasis, amoebic dysentery).

Secretory diarrhea can also be caused by inflammatory bowel disease. In children it can occur with excessive consumption of carrots and peas. The reason is increased intestinal motility. This type of diarrhea goes away on its own over time. Diarrhea with blood in a child develops against the background of an acute intestinal infection - campylobacteriosis, necrotizing enterocolitis, intussusception (intestinal obstruction).
Black diarrhea
After taking activated carbon and some vitamin and mineral preparations, stool may turn black. This may also be due to internal bleeding - from the stomach, esophagus or intestines, which occurs against the background of serious pathologies (ulcers, cancer, polyps, etc.). Associated symptoms of internal bleeding may include pale complexion, dizziness and anemia.
If you have black diarrhea, you should consult a doctor immediately. For diagnosis, a specialist will prescribe fibroesophagogastroduodenoscopy (examination of the esophagus, stomach cavity and duodenum using a gastroscope, which is inserted into the stomach through the mouth and esophagus) or colonoscopy (probing of the colon).
Chronic diarrhea
Frequent diarrhea in a child can manifest itself as a mild illness or more serious disorders. At the same time, the intestinal walls become susceptible to various allergens and toxins, and the protective functions of the liver are reduced. The body absorbs vitamins and minerals worse, metabolic processes worsen, and liver and pancreas diseases occur.
The following factors can trigger the development of chronic diarrhea:
- long-term use of medications, especially antibacterial ones;
- long-term treatment with hormonal drugs and NSAIDs;
- unbalanced diet;
- immunodeficiency states;
- stress, emotional overstrain.
Chronic diarrhea causes nausea, loss of appetite, bad taste in the mouth, belching, pain and bloating, weakness and trouble sleeping. To make a diagnosis, a microbiological examination of the stool is performed, as well as an assessment of the digestive system. Therapy is aimed at eliminating the causes and restoring the general condition.
Diarrhea with mucus
Mucous diarrhea in a child develops against the background of a violation of the intestinal microflora, polyps and hemorrhoids. Mucus binds and removes pathogenic microorganisms. Clinical signs of hemorrhoids include itching and bleeding from the anus. Intestinal diverticulitis also causes mucus to be secreted in the feces. Associated symptoms are abdominal pain arising on the left side and flatulence.
Diarrhea with mucus in children occurs as a result of insufficient bowel function. As a rule, this is associated with poor nutrition. This condition is accompanied by malaise, nausea and rumbling in the stomach. Liquid feces with mucus also occur with IBS (irritable bowel syndrome). To identify the disease and the purpose of therapy, you need to contact a specialist and conduct a diagnosis.
Diarrhea and fever
Diarrhea, vomiting and fever are the main signs of an intestinal infection, which can be caused by bacteria or viruses. An accurate diagnosis can only be made by a doctor after examination.
In the first hours after the onset of alarming symptoms, frequent small drinks are necessary. Dark colored urine may indicate a lack of fluid in the body. Normalizing the water-salt balance during intestinal infections is extremely important. Refusal of food and heavy drinks in case of diarrhea, vomiting and fever is a necessary condition. Drug treatment of intestinal infections is carried out under the strict supervision of a doctor.
Severe diarrhea
If the small intestine is affected, severe diarrhea may occur. This can happen during food poisoning and intestinal infections. Often such stools are watery, may contain food debris and do not cause abdominal pain. Bile acids and peptide molecules can promote the release of water and ions. The severe condition can occur when the absorption of bile and fatty acids is impaired, such as in Crohn's disease.