Starch in a child’s stool is a sign of a disease developing in the digestive system. The phenomenon is designated by the term “amilorrhea”. But a symptom does not always indicate a pathology. In some cases, this is a natural phenomenon that does not require therapeutic measures. When to sound the alarm, and in what cases there is no need to worry - more about this in the article.
Kinds
There are two types of starch in a child’s stool:
- Intracellular starch in a child’s feces is formed as a result of accelerated processes occurring in the small intestine. Products rich in fiber simply do not have time to break down completely and are excreted from the body in an undigested form, which provokes the appearance of intracellular starch.
- Extracellular starch in the feces of a child - appears in cases of improper functioning of the pancreas or stomach. It does not produce the proper amount of amylase contained in saliva. The disease is accompanied by a lack of gastric juice to completely break down complex carbohydrates, which leads to the appearance of extracellular starch.
Causes
Depending on the age of the child, the appearance of starch in feces can be both a pathological and physiological indicator.
Non-pathological causes
Normally, it is possible to detect starch in the stool of:
- Child up to one year old. Extracellular and intracellular starch may be detected, since the digestive system is not yet mature, many foods are introduced for the first time. Enzymatic pancreatic insufficiency is a variant of the norm, in the absence of other clinical signs of pathology: fever, diarrhea, vomiting, and so on.
- Child under 2 years old. Intracellular starch may be detected in the presence of frequent bowel movements. At this age, the child switches from breastfeeding to general feeding and the motility of the gastrointestinal tube adapts to the changes. If milk or an adapted formula is digested quickly, then regular products should linger longer in the cavity of the gastrointestinal tube. This can lead to the fact that even the cell wall does not have time to dissolve.
If, along with the detection of starch in the stool, the mother notices other pathological signs (see below “Concomitant symptoms”), then a more in-depth examination should be carried out.
Pathological causes
- intestinal infections;
- pancreatitis of various etiologies;
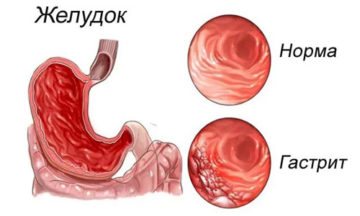
- gastritis or gastropathy;
- helminthiases;
- inflammatory bowel diseases: enteritis, ulcerative colitis;
- fermentative dyspepsia and imbalance of intestinal microflora;
- irritable bowel syndrome.
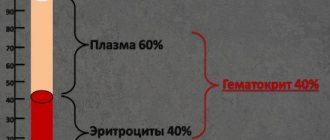
Diagnosis of amilorrhea
Diagnosis of starch digestion disorders is carried out through a laboratory general stool analysis, called a coprogram. The analysis is a comprehensive study of the physical and chemical properties of feces, identifying various inclusions.
The decoding of the coprogram may indicate two types of starch.
- Intracellular - found inside the membranes of plant cells. Normally, it should be completely digested and absent from waste products. The reason for the appearance of intracellular starch is the too rapid evacuation of intestinal contents, as a result of which enzymes do not have time to break down complex carbohydrates.
- Extracellular - starch grains, which must also be completely digested. It is detected when there is a lack of amylase in saliva, with reduced activity of amylase produced by the pancreas, and with reduced secretion of gastric juice.
Decoding the result of fecal starch analysis
In young children who receive a lot of carbohydrate foods, a small content of starch in the stool is acceptable. In adults it should normally be absent. If starchy grains are found in the stool, this indicates a digestive disorder in the small intestine.
There are two types of starch grains in feces.
- Intracellular - found inside cells of plant origin that are not destroyed by gastric juice. The detection of such grains indicates a disruption in the functioning of the stomach, changes in the intestinal microflora and putrefactive processes in the gastrointestinal tract.
- Extracellular grains are lumps of starch that have not been treated with amylase. This is observed in pancreatitis, exocrine pancreatic insufficiency, as well as intestinal diseases with increased peristalsis.
Treatment for these pathologies of the digestive organs is different, so the analysis should only be carried out by an experienced specialist who knows the differences between extracellular and intracellular starch grains.
Reasons for the appearance of extracellular starch in feces
This substance is undigested starch grains from cells that have collapsed.
A normal indicator is considered if there is no extracellular starch in the biomaterial. This is explained by the fact that the substance is properly broken down by enzymes of the gastrointestinal tract.
Stool analysis reveals pathologies of the digestive system
In medical terminology, an increase in starch in feces is called amilorrhea. It occurs due to dysfunction of the gastrointestinal tract.
The main reasons for the development of this condition are:
- Deficiency of amylase, a digestive enzyme, in saliva
- Decreased secretion of gastric juice
- Decreased activity of amylase, which is produced by the pancreas
Possible reasons for the appearance of starch in feces include the following pathologies:
- Enteritis is an inflammatory process in the intestinal walls, as a result of which food masses move faster through the digestive tract
- Gastritis and other diseases associated with dysfunction of the stomach
- Fermentative dyspepsia
- Intestinal dysbiosis affecting the absorption of starch
- Inflammation or atrophy of the pancreas, such as pancreatitis
Among the common causes of amilorrhea are increased motility of the small intestine, as well as its diseases.
In infants, starch is usually also found in the feces, but this phenomenon is not considered a pathological condition and is associated with the immature functioning of the secretory glands.
Factors that influence this condition are:
- Excessive consumption of foods that contain starch (potatoes, bananas, pears)
- Use of medicinal products containing this component before testing
- Poor nutrition
- Excessive drinking and smoking
- Living in an area of unfavorable environmental situation
Only an experienced specialist can detect the main reason for the appearance of extracellular starch in stool. Depending on it, he will establish the correct treatment tactics.
Starch in a child's stool
Starch is a complex chemical compound that enters the body mainly from plant foods. Starch in a child’s feces is observed when the gastrointestinal tract organs malfunction, due to which the breakdown processes worsen. A large number of grains of this substance in human waste products is called amilorrhea.
Starch in feces
The first stage of starch breakdown occurs in the human mouth. Our saliva contains the enzyme amylase, which begins the digestion process. The breakdown process then continues in the intestines. This complex carbohydrate breaks down into glucose upon contact with a pancreatic enzyme. Starch is completely absorbed by the body in the presence of a sufficient amount of amylase and pancreatic secretions. In a child under 1 year of age, the detection of starch grains is not always associated with the disease. In infants, this may occur due to incomplete functional maturation of the internal glands that produce enzymes. In infants, amilorrhea is considered normal. Most often, the pathology does not require therapy, since it disappears on its own after some time. Amilorrhea is diagnosed by conducting a special laboratory test called a coprogram. As a result of the study, the physical and chemical properties of the biomaterial are analyzed. Various impurities are being identified. When deciphering the analyses, two types of starch are indicated:
- Intracellular starch. It is contained in the inner membranes of plant cells. With the normal functioning of the gastrointestinal tract, this type of carbohydrate is completely digested. Due to the accelerated passage of undigested food through the intestines, enzymes may not have time to decompose the complex substance, which leads to the detection of traces of it in the child’s biomaterial.
- Extracellular starch. These are undigested grains from destroyed plant cells. The coprogram of a healthy person will not detect this substance in the biomaterial.
Causes of increased starch
After additional tests, the main causes of amilorrhea are discovered. This pathology can be caused by:
- deficiency of amylase in saliva,
- a small amount of gastric juice secreted,
- insufficiency of enzymatic activity of the pancreas.
A lot of starch in a child’s stool may indicate the development of pathologies. Such diseases include:
- Enteritis is a disease of the small intestine and its peristalsis. Due to the development of pathology, digested food begins to move extremely quickly through the digestive tract.
- Gastritis and other diseases that lead to disruption of the functioning of the stomach.
- Fermentative dyspepsia.
- Atrophy or inflammation of the pancreas.
- Impaired absorption of starch caused by intestinal dysbiosis.
The following factors may affect the results of the coprogram:
- Excessive consumption of potatoes, pears, bananas and other foods that contain starch.
- Poor nutrition.
- Living in an area with an unfavorable ecological environment.
Medicines containing starch carbohydrates are not recommended for children, which is why the reasons for poor coprogram results often lie in their use.
What to do
You should not try to treat the pathology yourself. You should immediately contact a gastroenterologist. The doctor will prescribe special tests.
The coprogram will help you understand in detail the root causes of malfunctions in the functioning of the child’s gastrointestinal tract.
To treat amilorrhea, you need to change your diet; first, it is recommended to limit the consumption of fruits and vegetables that contain the substance. In most cases, drug treatment with drugs that restore intestinal microflora cannot be avoided. These include probiotics and mild laxatives, which help normalize the functioning of the digestive system. If the functioning of the pancreas fails, the child is prescribed enzyme complexes: Pancreatin, Festal, Mezim. Medications may be prescribed to treat various pathologies of the intestines and stomach. The course of treatment and the drugs used are determined by the attending physician depending on the cause of amilorrhea.
Possible complications and prognosis
The prognosis is favorable, the indicators completely disappear with proper treatment.
If amilorrhea is not treated, a young child may experience the following conditions:
- stunting, underweight;
- developmental delay: difficulties with analysis and perception of new information;
- vitamin deficiency and all complications associated with it.
In continuation of the topic, be sure to read:
- Details about the coprogram: preparation, conduct and interpretation of the analysis
- What to do if your child is constipated?
- Worms in children: how do they manifest themselves and what drugs to treat them with?
- Irritable bowel syndrome: symptoms and treatments
- Causes of bloating and increased gas formation, treatment methods
- Why is there mucus in the stool and how to diagnose the cause?
- Undigested starch in the stool of an adult: causes and principles of treatment
- Mucus in a child’s stool: causes and what to do?
- Yeast fungi were found in a child’s stool: is it dangerous and is treatment necessary?
- Undigested food in a child’s stool: why does it appear and what does it mean?
Be sure to read:
How is rotavirus intestinal infection manifested and treated?
If the disease appears in a child under one year of age
In infants (up to one year), amilorrhea is not necessarily associated with the presence of any disease.
If the child is breastfed, then there should be no starch in principle. The presence of starch in the feces of babies is considered normal, since the secretory glands at this age are not yet sufficiently developed.
Amilorrhea goes away on its own as you get older. The only thing you can do is adjust your diet.
It is recommended to reduce the consumption of potatoes, pears, bananas and other starchy foods. If the problem cannot be solved in this way, then the child must be shown to a gastroenterologist, remember this for the future.
Treatment
The attending physician draws up a course of treatment, depending on the age of the child and the causes of the disease.
First of all, the baby’s diet is restructured. Representatives of legumes, various cereals, flour products, pasta, potatoes, cauliflower, sweet potatoes, nuts (peanuts, cashews, almonds, pistachios), carrots, melon, eggplant, beets, apples, zucchini are excluded from it. You don't have to eliminate these foods from your diet completely. It is enough to reduce their consumption by half.
Doctors advise increasing the consumption of dairy products, eggs, tomatoes, cucumbers, lean meats and white cabbage. If you see starch as a thickener in milk or sour cream, discard this product.
If such a diet does not provide the desired result, you must again contact your doctor so that he can prescribe an additional examination. After this, he may prescribe medication. In the case of Ameloria, it may consist of:
- Probiotics. Used to restore intestinal microflora. These drugs improve the functioning of the gastrointestinal tract and prevent stool disorders. These include: Florin Forte, Linex, Bifikol, Bifiform, Lactobacterin, Bifidumbacterin.
- Bacteriophages - these drugs have a “selective property”. They keep the microflora intact and kill only pathogenic bacteria. Representatives: Intesti bacteriophage, Staphylococcal bacteriophage.
- Enzymes - if their production is insufficient, special preparations will be needed to activate these processes. Main representatives: Pancreatin, Festal, Panzinorm, Mezim.
- Anthelmintics - Albendazole, Pyrantel, Levamisole, Mebendazole.
- Antidiarrheals - aimed only at correcting problematic stools. The most popular drugs: Hilak Forte, Normobakt, Lactobacterin, Enterol.
If drug treatment does not work and starch grains remain in the stool, the gastroenterologist will prescribe a more in-depth study. For this, the child undergoes an ultrasound of the abdominal cavity, as well as gastroscopy. The second, very unpleasant and at the same time the most accurate part of the examination.
Do not self-medicate. You can not only leave the baby’s situation in the same condition, but also aggravate it. Coordinate any actions with your doctor.
If, with amilorrhea, a child has stool disorders, gastritis, pancreatitis, enteritis or dysbacteriosis, it must be treated comprehensively. Otherwise, the effect will be insignificant. If pain appears in the intestines or stomach, the baby should be given painkillers: Nemisulide, Paracetamol, Ibuprofen.
Stool analysis for a newborn baby is best done twice a year. If the child is over 3 years old, you can limit yourself to one examination during the year. If starch grains appear in your child's stool, contact your doctor immediately.
Treatment of amilorrhea
If a small amount of starch grains is detected in the baby's stool, his nutrition is corrected. If the baby is breastfed, the mother's diet is changed; the quality composition of the mother's milk depends on her nutrition during breastfeeding.
Treatment of amilorrhea in children with polysaccharides in the stool and concomitant nutritional disorders is carried out by a gastroenterologist. Treatment depends on the etiological indicators.
- In case of malnutrition, a diet containing foods without the presence of starch is prescribed.
- In case of disruption of the child's pancreas, enzymes are prescribed.
- Dysbacteriosis is treated with drugs that improve the condition of the intestinal microflora.
- In case of inflammation of the gastrointestinal tract, a complete screening is carried out.
Proper nutrition after detecting starch in a child’s stool
Foods rich in starch are excluded from the diet.
To reduce the amount of starch in a child’s stool, exclude grains, cauliflower, legumes, baked goods, nuts, potatoes, pasta, and other foods rich in starch from the diet. Additionally, carrots, pumpkin, beets, zucchini, eggplants, strawberries, melon, and apples are excluded. There the amount of polysaccharides is smaller, but in case of serious pathology they should be abandoned.
Products containing protein are allowed for consumption: meat, dairy products, eggs. Vegetables eaten include tomatoes and cucumbers.
Drug therapy for amilorrhea in children
When selecting medications, take into account the child’s age, weight and identified pathology of digestive function. Pediatricians and gastroenterologists recommend the following drug groups for the treatment of amilorrhea in children:
- preparations containing gastrointestinal enzymes (Pancreatin, Creon, Mezim);
- non-addictive laxatives (Duphalac);
- probiotics (Linex, Normobact-L);
- anti-diarrhea medications (Smecta).
The doctor can prescribe the drug, determining the duration of its course individually, depending on the test results. When using medications, you cannot independently adjust the dosage of the drug.
If amilorrhea is detected in children, self-medication is excluded. Mom can seriously harm the digestive tract by choosing the wrong drug or its dosage. After therapy with a gastroenterologist and following a diet, the prognosis for the disease is favorable.
Do not self-medicate, consult a doctor! Be healthy.
Extracellular
Go to Medicines Catalog
Return to Catalog of medical terms
A B C
G D E F G H I K L M N O P R S T U V H C CH W SCH E Y
Extracellular - (extracellular) - located or originating outside the cell; for example, extracellular fluid is the fluid surrounding cells;
Found in 158 questions:
gastroenterologist April 15, 2021 / Nadezhda / Ryazan region
… . - in large quantities Rast. fiber digest. — single in the field of view Intracellular starch — not detected. Extracellular starch
- not found.
Iodophilic flora is normal. — single in the field of view Iodophilic flora patol. - only a few in sight... open
gastroenterologist May 18, 2021 / Sergey
... digest. IN SMALL QUANTITIES Intracellular starch not detected Extracellular
in moderation
Iodophilic flora is normal. IN MODERATE QUANTITIES Iodophilic flora ... open
gastroenterologist February 24, 2021 / Vera / Belgorod
... untranslated grows in small quantities. fiber digest. single in the field of view Intracellular starch not detected. Extracellular starch
not detected Iodophilic flora is normal. single in the field of view Iodophilic flora patol. only a few in sight... open
gastroenterologist February 18, 2021 / Irina / Moscow
... QUANTITY Rast. fiber digest. SINGLES IN VIEW Intracellular starch IN SMALL QUANTITIES Extracellular
IN A SMALL QUANTITY Iodophilic flora is normal. IN A SMALL QUANTITY Iodophilic flora is pathological. IN A SMALL QUANTITY ... open
gastroenterologist January 23, 2021 / Svetlana... / Omsk
… . light brown strong fecal odor of muscles. fibers without striations + indigestible. fiber +++ extracellular
+++ pathological iodophilic flora (cocci and rods) +++ mucus ... open
gastroenterologist December 25, 2015 / Irina / St. Petersburg
...at zero. I don’t particularly complain about my intestines. Tests taken in December: urine is normal. Coprogram - extracellular
2, digestible plant fiber - 3. Blood: cholesterol - 5.8, other biochemistry is normal. Clinical blood test: hemoglobin - ... open
urologist December 20, 2015 / alim / infection
Hello doctor, please tell me. I picked up the infection through sexual contact, I was told to take Tavanic 500 mil, I took it for 10 days, tell me what should I do next? open
December 20, 2015 / alim
1Mycoplasma genitalium Ureaplasma spp.(Ur.parvum+ Ur.urealyticum/T-960 Staphylococcus epidermidis 10″6 Acinetobacter species 10″6 Leukocytes 20-50 Extracellular
(Gram smear recommended) this is what was found for me
urologist December 4, 2015 / alim / help me how to recover
1Mycoplasma genitalium Ureaplasma spp.(Ur.parvum+ Ur.urealyticum/T-960 Staphylococcus epidermidis 10″6 Acinetobacter species 10″6 Leukocytes 20-50 Extracellular
(Gram smear recommended) open
gastroenterologist October 8, 2015 / A / Moscow
... stool analysis - coprogram
Consistency - mushy Form - unformed
Microscopic examination
Extracellular starch
— insignificant Intracellular starch — insignificant Oxalates — single Iodophilic flora normal — … open
gastroenterologist July 14, 2015 / Olga / Moscow
... fatty acids (soap) - no Undigested plant fiber - moderately Digested plant fiber - moderately Extracellular
-moderate Intracellular starch - single Crystals - none Activated carbon crystals - none Charcot-Leyden crystals ... open
gastroenterologist June 24, 2015 / Ekaterina... / Cool
... day. My name is Ekaterina, I’m 35 years old. Help me understand the results of the caprogram, the analysis revealed blastospores 3+, extracellular
- small amount, digestible fiber - small amount, muscle fibers without striations - moderate amount - ... open
gastroenterologist March 14, 2015 / Tatyana / St. Petersburg
... exhaustion 2 neutral fat 1 fatty acids 2 soaps 1 digestible plant fiber - 1 indigestible plant fiber 2 extracellular
1 iodophilic flora 1 BLOOD everything is normal except alpha-amylase-113 and immature granulocytes 0.1 after that the therapist ... open
gastroenterologist February 24, 2015 / Yana / Moscow
… . IN LARGE QUANTITIES Plant. fiber digest. IN LARGE QUANTITIES Intracellular starch SINGLES IN THE FIELD OF VIEW Extracellular
IN A SMALL QUANTITY Iodophilic flora is normal. SINGLE IN FIELD OF VIEW Iodophilic flora patol. SINGLES IN THE FIELD … open
Possible consequences and prognosis for life
The appearance of starch in stool is not a disease, but only a symptom of it.
It is important not only to remove negative phenomena, but also to eliminate their cause. Without treatment, disturbances in the functioning of the stomach, intestines and pancreas can lead to the following conditions:
- progressive weight loss;
- Iron-deficiency anemia;
- avitaminosis.
All these conditions are associated with insufficient digestion of food and lead to disruption of the functioning of internal organs.
Amilorrhea caused by pathology of the pancreas requires special attention. This organ is very sensitive to negative influences and easily fails. The most dangerous complication is pancreatic necrosis. Complete cessation of pancreatic function can be fatal.
The prognosis for amilorrhea depends on its cause and the severity of the pathology. The sooner the source of the problem is found and treatment is carried out, the higher the chances of a favorable outcome.
Associated symptoms
If the cause of the appearance of starch in the feces is pathological changes in the digestive system, then the mother should pay attention to the accompanying symptoms:
- abdominal pain;
- rumbling along the intestines;
- stool disorders in the form of diarrhea, increased stool volume;
- nausea;
- vomit;
- flatulence;
- intestinal colic;
- the presence of other pathological impurities in the stool: blood, mucus, undigested muscle fibers;
- temperature increase.
What is coprogram and why is it carried out?

It is almost impossible to make a correct diagnosis and notice the presence of a particular disease without certain tests. Stool scatology is one of the most popular, fastest and most accessible research methods. This laboratory test is performed in almost every hospital.
Feces, their physical characteristics and chemical composition can tell a lot about how the body works. In particular, by studying the results, the doctor can identify the peculiarities of the human digestive tract. In addition, testing is used in the diagnosis of diseases of the liver and gallbladder, pancreas, and stomach. Fecal analysis in children helps the pediatrician get an overall picture of the development of the digestive tract and the presence of metabolic failures. The study is indispensable in diagnosing helminthiasis, as well as detecting hidden gastrointestinal bleeding.
There are not many diseases of internal organs for which differential diagnosis does not require obtaining a coprogram. The doctor may order an examination to check whether starch is present in the stool, whether there are traces of helminthic infestations, proteins or occult blood, etc. A natural question is whether the examination requires any specific preparation. Some rules will help you get accurate information:
- It is recommended that you eat a basic, healthy diet for a few days before collecting samples. You should exclude colored vegetables, fish, fatty meats and, of course, foods with food dyes from your diet.
- If you are taking any medications without the ability to stop therapy for a few days, be sure to tell your doctor.
- The collection should not be carried out on women during menstruation - it is better to wait until it ends.
- If bowel movements are a problem (for example, constipation), you should not use laxatives or enemas, as this may distort test results. It is better to wait for natural bowel movements.

Test results largely depend on proper sample preparation and collection. So how to donate feces? There is nothing complicated in the procedure. To collect samples, it is recommended to purchase a special plastic container with a lid. Such containers are sold in almost any pharmacy. They are equipped with a convenient spatula for collecting feces.
Before the procedure, you should wash, otherwise during the study, uncharacteristic bacterial organisms, epithelial cells, and chemical compounds may be detected, which, naturally, will affect the further diagnostic process. The collection is carried out immediately after defecation.
According to laboratory technicians, a complete analysis requires one teaspoon of material. Smaller samples may not be sufficient to perform all tests. Feces should be sent to the laboratory as quickly as possible - no later than 5-7 hours after collection. The longer the biomaterial is stored, the less likely it is to obtain accurate results, because under the influence of environmental factors (light, temperature, air) some chemical components of feces are destroyed, which leads to distortion of information. It is best to store the sample container in the refrigerator.
If a coprogram is carried out on a baby, then parents are not recommended to collect feces from the diaper - it is better to first place a clean diaper under the baby. If a special plastic container is not available, samples can be placed in a glass jar, but it must first be sterilized.
basic information
Starch is a substance that is often found in food (plant foods). This is a complex carbohydrate, which, when present in a growing plant, protects it from low temperatures and activates the development of plant fibers in the spring.
The following products contain starch:
- rice porrige,
- oatmeal,
- corn,
- wheat,
- potato,
- peas,
- beans,
- kvass,
- Rye bread.
When eating food, this polysaccharide begins to break down in the oral cavity, with the help of enzymes contained in saliva. In the stomach it is broken down by gastric juice. After these processes, starch is converted into glucose and is completely absorbed by the body. This applies to both adults and children.
If starch was found in large quantities in the child’s coprogram, then you are dealing with the disease Amilorrhea. Sometimes, the appearance of such a problem is caused by heavy complementary foods that were introduced into the baby’s diet too early, with diseases of the gastrointestinal tract.
Causes of starch in a child’s stool
The causes of amilorrhea can be divided into two groups: general and age-related.
Common reasons:
- stool disorders (diarrhea),
- stomach diseases (in most cases gastritis),
- improper functioning of the pancreas,
- dysbacteriosis,
- eating large amounts of food rich in starch,
- pancreatitis (acute and chronic),
- enteritis.
Up to a year
Amilorrhea in infants does not mean that the child is sick. When a child is breastfed, starch cannot be supplied with food. Its appearance in feces is due to the immaturity of the secret glands. With the process of growing up, Amilorrhea goes away on its own. To get rid of this problem as quickly as possible, you can rearrange your child’s diet. Reduce the amount of starchy vegetables and fruits you eat.
After a year
At one year of age, the child’s diet begins to be replenished with various products. This is the main reason for the appearance of Amilorrhea. Introduce new foods into your baby's diet very carefully. If the problem persists, reduce your intake of certain vegetables and fruits.
After 2 years
At 2 years of age, the occurrence of Amilorrhea is associated with disturbances in the functioning of the small intestine. In order to verify this, you need to undergo an examination.
If the equipment does not display problems and disorders associated with the functioning of the gastrointestinal tract, then medications will not be needed. It is enough to visit a gastroenterologist and with his help create a detailed diet for the child. He will select an individual diet. After some time, the child will again need to take a stool test. If starch grains remain, then the pediatrician should prescribe an additional examination.
After 3 years
The older you are, the more reasons there are. After three years, amilorrhea may indicate not only disturbances in the gastrointestinal tract or poor nutrition. This disease may indicate the presence of gastritis or pancreatitis. To determine the exact cause, the child must undergo a thorough examination of the entire digestive system.
Main causes of pathology
The reasons for the presence of starch in the stool of infants and children under one year of age do not always indicate a disease.
Often this symptom is associated with incompletely formed secretory glands. As you grow older, this phenomenon goes away without requiring specific therapy.

In a one-year-old child, when new foods begin to appear in his diet, amilorrhea is a normal phenomenon that is associated with the consumption of foods containing carbohydrates.
If the problem does not go away on its own, it is recommended to limit the child’s consumption of products with these components..
If a stool examination shows the presence of starch in the stool of a 2-year-old child, this indicates a malfunction of the small intestine. In this case, you should not self-medicate, but rather consult a doctor to confirm the diagnosis.
A large amount of starch in a stool test in children after 3 years of age signals not only problems with the gastrointestinal tract, but also errors in nutrition.
In addition, the symptom occurs with the following pathologies:
- gastritis;
- pancreatitis;
- enteritis;
- fermentative dyspepsia.
If starch (specific grains) is detected in the child’s stool, it is recommended to consult a doctor, who, based on the results of the studies, will make the correct diagnosis.
Physical characteristics of feces as evidenced by deviations

Before starting to study the chemical composition of feces, the laboratory assistant must study and enter physical characteristics into the questionnaire. They are no less important for creating a high-quality coprogram.
By the way, the patient can only note some disorders independently. For example, there are average statistical norms for the daily amount of feces. For an adult, this is 100-200 g. Naturally, we are talking about those cases when the patient follows the correct diet:
- the release of less than 100 g of excrement per day is observed with constipation of various origins;
- more than 200 g often indicates inflammation of the intestinal mucosa, accelerated evacuation of food masses, and insufficient supply of bile;
- If a person excretes more than 1 kg of excrement per day, this indicates serious pancreatic insufficiency.
Another important factor is consistency. Feces are 80% water. With diarrhea, this figure increases to 95%, but constipation is accompanied by a decrease in the amount of fluid to 70-65%. Normally, the stool of an adult is formed and has a dense consistency. What the analysis can tell you:
- abundant semi-liquid feces with oily impurities may indicate impaired absorption of fat in the intestines;
- pasty stool appears when there is insufficient amount of bile and secretion disorders in the pancreas;
- loose, mushy excrement indicates increased fermentation processes, colitis, enteritis;
- liquid feces appear when digestive processes in the small intestine are disrupted;
- solid feces of a ribbon or spiral shape are observed with constipation, hemorrhoids, as well as with the formation of tumors in the colon;
- semi-liquid, foamy feces are characteristic of fermentative colitis and irritable bowel syndrome.
An important factor for diagnosis is the color of the stool:
- light brown stool indicates accelerated evacuation of intestinal contents;
- reddish feces are observed with inflammation and ulceration of the mucous membrane of the colon;
- with disorders of motility and digestion in the small intestine, patients often note that the stool becomes yellow;
- white stool may indicate blockage of the bile ducts;
- With diseases of the pancreas, stool may acquire a gray or yellow-gray tint.
As for other signs, they also pay attention to the smell. Naturally, it depends primarily on food and the amount of protein foods consumed.
This is a subjective factor, although it should not be ignored. For example, the presence of a sour odor may indicate fermentative dyspepsia. A strong stench is characteristic of diseases of the pancreas and a violation of the outflow of bile. And with the accelerated movement of food masses, the stool has a characteristic odor of butyric acid.
It is worth understanding that physical characteristics directly depend on nutrition. That is why, a few days before the test, it is recommended to switch to simple, healthy foods. Overeating, a strict diet, the use of dyes and preservatives - all this can distort the results.
Separately, it is worth highlighting such a parameter as pH. The reaction of feces should be neutral - its values range from 6.8-7.6. If the test data does not correspond to the norm, then the following violations are possible:
- a slightly alkaline reaction occurs against the background of disturbances in the digestive processes in the small intestine;
- an alkaline reaction may indicate diseases of the pancreas, digestive disorders in the stomach, increased secretory activity in the large intestine, ulcerative colitis;
- a sharply alkaline reaction, as a rule, is observed with putrefactive dyspeptic symptoms;
- a pronounced acidic environment, on the contrary, indicates dyspepsia associated with intense fermentation processes in the intestines;
- a moderately acidic environment is associated with impaired absorption of fatty acids.
By the way, a child’s feces can give an acidic reaction, especially if the newborn is bottle-fed - this is due to the composition of the milk formula, so there is no need to worry in advance. Additional information is needed to make an accurate diagnosis.
Diagnostics
Extracellular starch in a child’s feces can be detected both by visual examination and with the help of special medical equipment.
To determine the presence of the disease, it is necessary to conduct a stool examination - a caprogram. If necessary, other additional studies may be prescribed.
Diagnostics:
- stool culture (bacteriological examination) is a procedure aimed at studying and determining the intestinal microflora;
- stool examination for dysbacteriosis is the study of stool in order to determine bacterial damage and disturbances of the intestinal microflora;
- Ultrasound of the abdominal organs;
- fibrogastroduodenoscopy (performed in older children) is an endoscopic examination that allows you to examine the esophagus, stomach and duodenum.

Infants in most cases are prescribed only caprogram.
Preparing for the capprogram
Preparation for the study includes several basic rules that will allow you to correctly collect material and establish an accurate (correct) diagnosis.
Preparation:
- a few days before the analysis, exotic and varied foods should be excluded from the diet;
- 2 days in advance you must completely give up fruits and vegetables that contain dyes;
- 3 days in advance, you should stop taking various medications - antibiotics, drugs that affect intestinal motor function, enzyme-containing drugs;
- adherence to dietary nutrition - refusal of meat products, potatoes, dairy products.

Parents should also purchase a special container for collecting biological material in advance.
Material collection
Extracellular starch (small inclusions can be found in a child’s stool during collection) is not a severe pathological disorder. However, it is necessary to take the test. At the same time, feces must be collected correctly for the research results to be correct.
Collection of material should be carried out only after emptying the bladder and hygiene procedures.
It is prohibited to collect feces from the toilet. In infants, it is recommended to collect material from diapers or oilcloth. However, you should not collect feces from diapers, since they may contain various impurities (urine), which can affect the results of the analysis.
It is recommended to use a special spatula or spatula to collect feces. It is not allowed to use wooden or glass containers as containers. After collecting the material, the container must be tightly closed with a lid and the child’s personal information must be indicated on it. The total volume of collected material should be at least 15-20 g.
All material should be collected only in the morning 2-3 hours before visiting the clinic. The maximum shelf life of the material in the container is no more than 8 hours. It is recommended to store it at a temperature of 3-5 0C.
Timeframe for analysis
The duration of the study depends on the clinic and the workload of the laboratory. You can get acquainted with the results of laboratory tests within 1-2 days after donating stool. In some cases, the process may take up to 3-5 days.
Decoding
Extracellular starch in a child’s feces can indicate various pathologies. The specific cause of the disease must be determined by a specialist after conducting and deciphering the caprogram.
Based on the data obtained, a diagnosis is made:
| Indicators | Norm | General information |
| Consistency | Dense, soft (shaped) | The amount of fluid above 85% indicates the presence of diarrhea; if the water level is less than 50%, constipation may be present. |
| Form | Shaped, cylindrical | If the material is in the form of a pulp, the child eats a large amount of protein and a small amount of plant fiber. |
| Smell | Fecal | The severity of the indicator increases with the consumption of large amounts of protein. With a strong foul odor, putrefactive processes in the intestines may develop. A sour smell indicates infectious diseases or disturbances in the production of enzymes. |
| Color | Light shades, brown (including dark brown), yellow-green allowed | Dark shades indicate the consumption of a large amount of meat. Light colors indicate the consumption of lactic acid products. The absence of color indicates problems with the liver or blockage of the bile ducts. Red color indicates the presence of bleeding in the lower gastrointestinal tract, black indicates bleeding in the upper gastrointestinal tract. |
| Reaction | Neutral, less often - weakly acidic | High acidity levels indicate the development of bacterial infections. With a high alkali content, problems arise with the breakdown of protein compounds. |
| Blood | – | The presence of blood indicates internal bleeding in the digestive tract. |
| Slime | Absent or traces present | High mucus content indicates inflammatory reactions. |
| Leftover undigested food | – | Undigested food indicates disturbances in the production of enzymes or diseases in the biliary system. |
| Muscle fibers (modified) | Absent, minor concentration possible | An increased content indicates insufficient production of gastric juice or enzymes, which results in disturbances in the breakdown of proteins. |
| Muscle fibers (unmodified) | Absent, minor concentration possible | High levels are characteristic of disturbances in intestinal motility or disorders of enzyme production. |
| Detritus | Absent, minor concentration possible | Indicates inflammatory processes in the gastrointestinal tract. |
| Plant fiber (digestible) | Absent or traces present | Possible disorders: putrefactive processes, enzymatic disorders, blockage of the bile ducts. |
| Fatty acid | – | Light maintenance in infants is the norm. In adults, this indicator may indicate various problems with the gastrointestinal tract. |
| Neutral fat | – | In infants, fatty acids may be present in small quantities. In adults, the presence of neutral fats indicates various intestinal disorders. |
| Starch (extracellular and intracellular) | – | With a low amylase content, starch is found in the stool. |
| Soap | Absent or traces present | The presence of soaps in stool indicates insufficient enzyme production. |
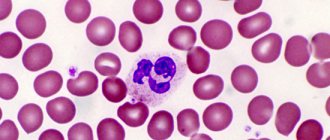
| Leukocytes | Minor units detectable by microscopic examination | The presence of leukocytes in the stool indicates infectious processes. |
| Red blood cells | Minor units detectable by microscopic examination | The presence of red blood cells indicates internal bleeding in the gastrointestinal tract. |
| Crystals | – | The presence of crystals is characteristic of various diseases. |
| Iodophilic flora | – | This indicator may indicate the presence of fermentation processes. |
| Clostridia | Absent or few cells present | They are formed due to enzymatic failures, which, in turn, causes the development of putrefactive processes. |
| Epithelial cells | Absent or few cells present | Their presence indicates inflammatory processes. |
| Yeast-like fungi | – | Indicate the presence of dysbiosis caused by taking antibacterial drugs, infectious processes or decreased immunity in the child. |
If there are suspicions of other internal gastrointestinal diseases, additional studies are prescribed.
Stool analysis main indicators
The study of feces and determination of its chemical composition and physical properties is called a coprogram.
This analysis is prescribed to diagnose pathological conditions of the digestive system.
The main indicators included in the study include:
- Form
- Color
- Smell
- Consistency
- Presence of mucus or blood
- Fecal reaction
- Unchanged and modified muscle fibers
- Leftover undigested food
- Red blood cells
- Digestible fiber (vegetable)
They also look at the absence or presence in the biological material of extracellular and intracellular starch, leukocytes, proteins, bilirubin, yeast-like fungi, crystals, fatty acids, detritus, clostridia, iodophilic flora, neutral fat.
Regarding starch in feces, two types of complex carbohydrate can be found in biological material:
Features of stool analysis in a child, main indicators
If gastrointestinal dysfunction is suspected, the doctor prescribes a stool test, since amilorrhea cannot be suspected by the appearance of the child. With the help of stool analysis, the diagnosis will not only be confirmed, but also treatment will be selected. When conducting tests, the following indicators are taken into account:
- amount of material (depending on the age and weight of the person);
- shape (normally cylindrical);
- consistency (with sufficient water consumption it is soft);
- Brown color);
- specific smell;
- leftover food;
- secretions that are absent in healthy people (red blood cells, pus);
- parasites and their eggs.
Chemical studies are carried out to determine the acidity (ph) of feces and breakdown products that should be absent (red blood cells, proteins, bilirubin). In healthy children, stool acidity (ph) varies from slightly alkaline to slightly acidic. For an accurate result of stool coprogram, stool is examined under a microscope. It detects the presence of complex saccharides, which look like grains under a microscope.
The cause of amilorrhea depends on the type of starch detected in the baby's stool, any of which should not be observed in the feces.
- Intracellular starch is covered with a membrane that is broken down by enzymes. Completely digestible. The presence of this type indicates impaired intestinal function and decreased peristalsis. The carbohydrate is evacuated without having time to be absorbed.
- Extracellular starch - found when there is a lack of amylase in parts of the digestive system, insufficient production of gastric juice.
Based on the obtained stool coprogram, the attending physician will select therapy based on the collected medical history. It takes into account the patient's age.
Important! When transferring the collected material, the patient’s age is signed; the presence of a small amount of complex carbohydrates (starch) in children under 2 years of age is the norm.