List of indicators
Liver tests are a section of the biochemical panel of laboratory tests, the basis of which is a blood test. They include a range of indicators such as:
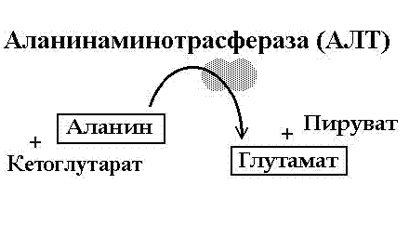
- Alanine aminotransferase (ALT), aspartate aminotransferase (AST).
- Gamma glutamyl transferase (GGT).
- Alkaline phosphatase (ALP).
- Bilirubin (total, direct, indirect).
- General protein.
- Albumen.
Sedimentary samples can be used to assess protein content: thymol, sublimate, etc. Previously, they were included in the list of studies as mandatory, but with the introduction of new laboratory diagnostic methods they became less in demand. Relevance remains for determining the activity of the process in hepatitis and cirrhosis of the liver.
Elevated liver tests mean an increase in the amount of gamma globulins and beta globulins and a decrease in the concentration of albumin and confirm the presence of an inflammatory process in the liver.
The reliability of the result is influenced by hyperlipidemia, which occurs when the patient consumes fatty foods on the eve of the study. False information can be obtained if, in addition to liver disease, there are kidney diseases and systemic connective tissue lesions.
The list of indicators required to determine often includes components of the lipid spectrum, otherwise known as lipid profiles.
These are total cholesterol, lipoproteins (cholesterol fractions) of high, low and very low density, triglycerides (esters of glycerol and fatty acids).
The atherogenicity coefficient is also calculated, which indicates the likelihood of developing atherosclerosis. An increase in triglyceride content is observed with fatty infiltration of the liver; Liver tests relative to this indicator are increased during pregnancy.
Cholesterol and lipoproteins are determined to identify cardiovascular pathology, but are not very informative regarding liver diseases.
Liver biochemical blood test parameters in some cases include serum iron. An increase in level in combination with an increase in AST and ALT indicators is a clear sign of destruction of hepatocytes (liver cells).
What do liver tests show if only serum iron increases? As a rule, this may be a consequence of excess intake or accumulation, and requires further examination.
Why is biochemistry needed?
Biochemistry helps to detect diseases of the circulatory system, internal organs, and establish the level of glucose, bilirubin and urea. These indicators can only be determined from the results of a biochemical study. It is carried out in the clinic laboratory or using a portable analyzer. This study is indicated to draw up a clinical picture of pathologies occurring in the body. It helps determine:
- Glucose level, since a decrease or increase in its levels may indicate improper functioning of the pancreas due to the development of diseases that impair its functions (diabetes mellitus, oncology, etc.);
- The level of bilirubin, a substance remaining after the breakdown of red blood cells. Its deficiency or excess indicates pathologies of the liver or gall bladder (hepatitis, acute cholecystitis and others);
- Hemoglobin level, an increase or decrease in which is a sign of poor coagulation, anemia, leukemia, HIV infection, etc.;
- The level of urea, which characterizes the function of the kidneys and liver, and any deviations from the norm indicate the malfunction of these organs;
- The level of protein, the increase of which in the body threatens obesity and the development of rheumatoid arthritis, and the decrease - problems with the heart and coronary vessels, which is confirmed by a cardiogram.
Biochemistry is often prescribed to those who have undergone chemotherapy or have problems with the circulatory system, heart pathologies and vascular diseases.
Typically, a doctor prescribes a test during an examination and doubts about the diagnosis, so it is not recommended to undergo it yourself. Biochemical analysis and general analysis differ significantly, so they are prescribed based on the patient’s health condition and the expected diagnosis.

Collection of material for biochemistry
Rarely defined indicators
Lactate dehydrogenase and its isoenzymes are not included in the standard liver tests, but are important for deciphering blood tests in normal and pathological conditions. An increase is observed in patients suffering from viral and toxic hepatitis and liver cirrhosis.
A liver blood test for copper and ceruloplasmin levels is necessary for diagnosing a severe genetically inherited pathology - Wilson-Konovalov disease.
Bile acids accumulate in body tissues during cholestasis (stagnation of bile). Liver blood tests can become more informative if the concentration of bile acids is determined in a disease with a cholestatic component.
Serum cholinesterase (pseudocholinesterase) belongs to a class of enzymes. Due to liver diseases such as hepatitis, cirrhosis, as well as liver metastases and congestion in heart failure, its concentration in the blood serum decreases.
How to measure biochemical parameters
To quantify results, milligrams, milliliters, or even smaller units of measurement are used. To do this, a number is written on the analysis form, followed by a ten with a degree (to indicate the number of zeros).
To show the content of a certain substance dissolved in the blood, international units are used - or millimoles per liter (u/l, mmol/l). This unified accounting system has been adopted in all countries. In this case, the number indicates the molecular weight of the test substance dissolved in one liter of blood.
Typically, the analysis decoding form indicates the standards of a particular laboratory in parentheses. The doctors of the medical institution know them.
Liver test norms
The presence of pathology can only be determined by comparison with the indicators of a healthy person. The norm of liver tests is indicated in the table:
| Indicators | Men | Women |
| AST | Up to 47 U/l | Up to 31 U/l |
| ALT | Up to 37 U/l | Up to 31 U/l |
| GGT | Up to 49 U/l | Up to 32 U/l |
| Total bilirubin | 8.5 - 20.5 µmol/l | 8.5 - 20.5 µmol/l |
| Direct bilirubin | Up to 15.4 µmol/l | Up to 15.4 µmol/l |
| Bilirubin indirect | Up to 4.6 µmol/l | Up to 4.6 µmol/l |
| Total protein | 60 - 80 g/l | 60 - 80 g/l |
| Albumen | 40-60% | 40-60% |
Liver tests with significant fluctuations below or above normal and no signs of disease should be repeated to eliminate errors at all stages of the analysis.
The Importance of Standard Research
The interpretation of the blood test for the liver complex is carried out at an appointment with the attending physician, who is guided by the totality of clinical symptoms and the results obtained. It is also useful for the patient to know about the main components of the biochemical profile intended for the diagnosis of liver diseases.
The norms of liver tests are indicated on the forms, but deviations in the direction of increasing or decreasing indicators require detailed consideration.
The biochemical activity of the pathological process in the liver can be judged by taking a test for liver enzymes in the blood:
- Aspartate amine transferase. Indicative for liver diseases. In addition, it is used as a marker of damage to the heart muscle (myocardium). Deciphering the analysis of liver samples is aimed at identifying elevated levels of AST, which happens with hepatitis and liver tumors.
- Alanine amine transferase. It is the level of alanine aminotransferase that is considered to be a reliable sign of acute liver damage. An upward shift in value is observed even before the appearance of a bright clinic. With a large volume of damage to the liver tissue, the indicator increases tens of times. Both AST and ALT are enzymes localized inside the cell that take part in the metabolism of amino acids. The concentration increases with necrosis of hepatocytes. A valuable diagnostic criterion can be the de Ritis coefficient, calculated based on the ratio of ALT and AST; for viral hepatitis its value is less than 1. Chronic inflammatory diseases accompanied by degenerative changes are characterized by an indicator equal to or exceeding 1. A de Ritis coefficient greater than 2 is observed in alcoholic liver disease.
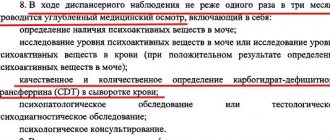
- Gamma-glutamyl transferase (gamma-glutamyl transpeptidase). How many units of GGTP in a liver test is considered an acceptable value? Normal numbers range from 8 to 61 IU/L for men and from 5 to 36 IU/L for women. The enzyme is active in cholestasis, inflammation, tumor processes and alcoholic liver disease. Its increase is also facilitated by taking medications that have a hypnotic and anxiolytic effect from the group of benzodiazepines and barbiturates, the use of narcotic substances, and contact with hepatotoxic poisons.
- Alkaline phosphatase. It is one of the most accurate markers of cholestasis and hepatocellular carcinoma (malignant tumor of the liver), but is considered as evidence of damage

liver only with a simultaneous increase in other indicators of the liver complex in the blood test. This is explained by the fact that alkaline phosphatase isoenzymes are contained, in addition to the liver, in bone tissue, the intestinal wall, etc. An isolated increase in alkaline phosphatase may be a reflection of a pathological process of extrahepatic localization.
What does an increase in liver enzyme test results mean? Excessive biochemical activity confirms the assumption of an acute pathological process. This giant entered the industry long before many other developers, being the first to offer advanced animation technologies for casino players. We are talking about software from Microgaming, it is very cool and it is simply impossible to take your eyes off the realistic animation, play here https://www.playcasinox.online/, you can trust this site, and I advise you to subscribe to their ielegram channel, there are tempting offers for gumblers. The number of fans, both of the live games themselves and of the best online casinos offering them, is constantly growing.
A long-term, but not so pronounced increase in liver tests may indicate chronic inflammation, narrowing of the lumen of the bile ducts due to incomplete obstruction (overlap).
Among the bile pigments, to decipher the analysis of liver samples, it is necessary to evaluate the level of bilirubin. It is divided into the following types:
- general;
- direct (conjugated, connected);
- indirect (unconjugated, free).
The total bilirubin indicator increases due to one or both fractions (direct, indirect), the level of which determines its value.
Liver tests in blood biochemistry are needed for the differential diagnosis of conditions accompanied by jaundice.
Hemolytic jaundice is characterized by an increase in the fraction of indirect bilirubin, while with mechanical jaundice the value of the direct fraction increases. Parenchymal jaundice is spoken of in the case of a significant increase in both direct and indirect, and in general total bilirubin.
Protein levels in blood serum are also included in the analysis of liver samples:
- Total protein. The normal level of total protein in liver tests for women and men is 60–80 g/l. Hypoproteinemia (decrease in total protein) accompanies chronic liver diseases. Hyperproteinemia is observed during physical activity and dehydration.

Albumen. Albumin is a transport protein whose task is to transport hormones, vitamins, fatty acids and other substances between cells. Liver tests are slightly elevated during pregnancy and lactation (breastfeeding), which applies to albumin and is within normal limits. Albumin decreases with chronic liver pathology.
Pigment fractions in human metabolism
Biochemistry and modern medical science are not the simplest areas of knowledge; an accessible presentation of the material is associated with the problem of the reader’s double request - one person wants to receive the most accurate, objective, scientific data, and the other wants the most simplified description of a phenomenon, a parameter, allowing one to understand the essence of what is happening in changes in the body. We will try to satisfy both requests by providing both scientific and simplified data on the topic.
General information about bilirubin
The term bilirubin comes from the combination of the Latin words bilis - “bile” and ruber - “red”. Bilirubin is a pigment, one of the main components of bile. In medical practice, it is called a liver and bile marker, since the amount of its content can be used to track the health of the liver and gallbladder. This pigment appears in the blood after the death of erythrocytes - red blood cells, whose main mission is to transport oxygen to the tissues of the human body.
Pigment is an organic compound that can give color to the environment in which it is contained. The pigment fraction - biliverdin - colors the medium in a characteristic green color. Indirect bilirubin will color the medium yellow. Depending on the concentration of NB, the color of the medium will vary from pale yellow to deep orange-red. The pigment fraction - stercobilin - colors the medium brown; the degree of concentration of the substance determines the color saturation.
Metabolic mechanism of biochemical transformations of indirect bilirubin
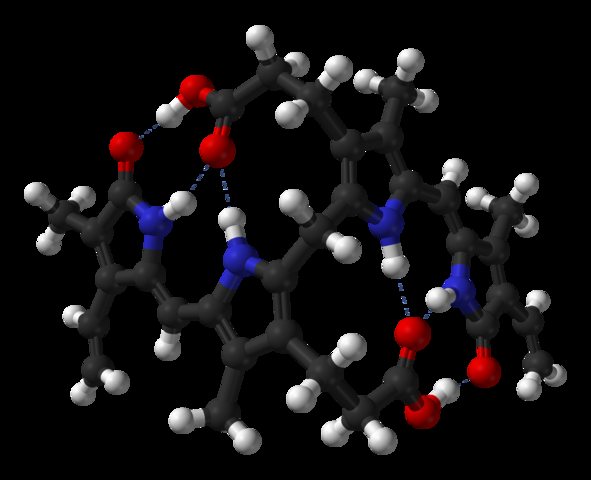
The red blood cell - the erythrocyte - is capable of transporting oxygen only because it contains the complex polypeptide “hemoglobin”. This protein contains a divalent iron atom, which makes it possible to retain oxygen atoms. Divalent iron atoms are the strongest natural poison, deadly to any living organism. It is not dangerous to humans because the peptide chains securely hold it.
The red blood cell lives in the body for 3-4 months and then dies. Moreover, it dies, and does not die - the death of red cells is not natural. During the reticular circulation cycle, red blood cells undergo something of a fitness test in the spleen - as long as the red blood cell membrane is flexible and allows it to squeeze through the reticular cells of the blood capillaries, it is considered fit. If the membrane of an erythrocyte has lost its flexibility and it is “stuck,” then a macrophage comes to “pick it out” - a protective cell of the body that destroys harmful substances and microorganisms, an active participant in the process of homeostasis.
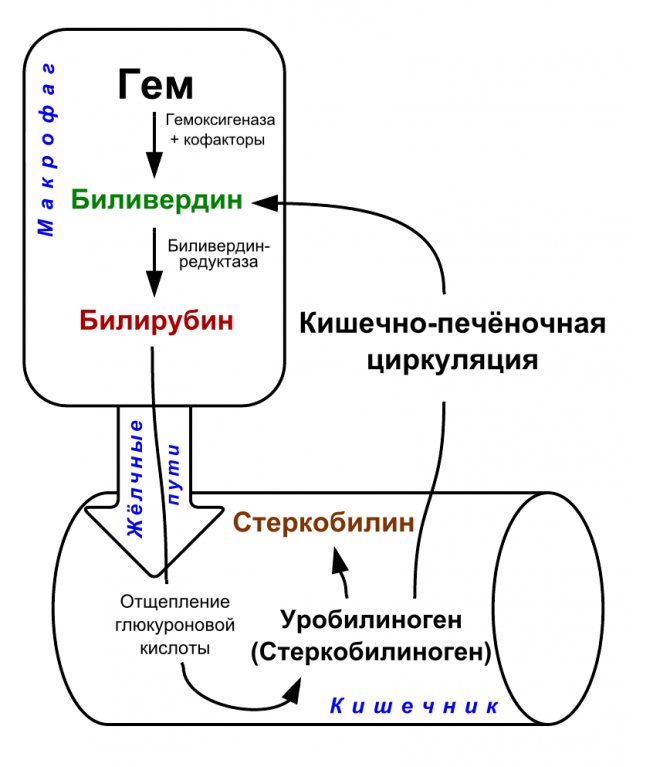
In the body of a macrophage, the hemoglobin of a dead red blood cell breaks down into two substances - “heme” and “globin”. The first is a chemical compound containing dangerous iron, the second is a protein compound that will be broken down into amino acids by the body over time. Heme will break down to biliverdin, and then biliverdin will become indirect bilirubin under the influence of enzymes.
Attention! NB is extracted from the macrophage body and enters the blood - it is a very toxic substance that actively interacts with lipids. Lipids are organic compounds that partly make up the cells of the body's tissues. Interaction with unbound bilirubin kills them.
Metabolic mechanism of biochemical transformations of direct bilirubin
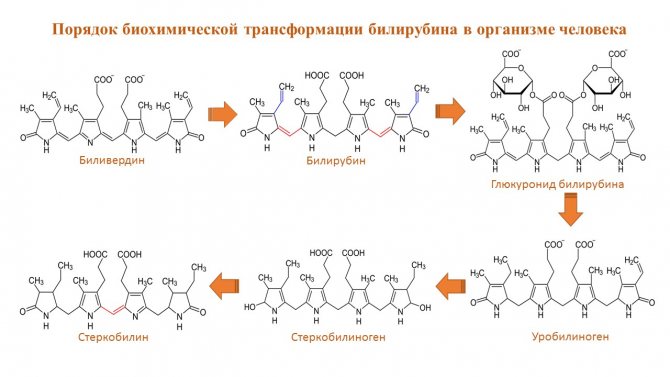
In the blood, NB is attached to an albumin molecule (polypeptide) and thus becomes relatively safe. The situation changes dramatically for the worse when the amount of NB exceeds the albumin content in the blood. There are two ways of cleansing in the body. The first route for fat-soluble substances is the liver and gall bladder, the second for water-soluble substances is the kidneys. NB, as a fat-soluble substance, is excreted by the liver.
In the liver, NB is transformed into direct bilirubin, which, after interaction with glucuronic acid, is converted into bilirubin glucuronide - this fraction is already water-soluble. Bilirubin glucuronide, along with bile, enters the small intestine, where it is reduced to urobilinogen, another pigment fraction. Then urobilinogen from the small intestine enters the large intestine, where, under the influence of intestinal flora and fauna, it becomes first stercobilinogen and then stercobilin. Stercobilin leaves the body along with feces, completing the process of clearing the body of bilirubin.
Biliverdin, bilirubin and stercobilin are pigments. They are able to color tissues and waste of the body in a specific color. Stercobilin colors feces brown. Biliverdin colors tissues green during the healing of bruises - this substance is responsible for the “green” stage of restoration of the body’s soft tissues. Bilirubin is a yellow-red pigment. During the healing of a bruise, it is responsible for the “yellow” stage of soft tissue regeneration. It can turn human skin yellow (jaundice) if its amount in the blood exceeds the norm. Having become water-soluble, it begins to be excreted through the genitourinary system, coloring the urine in the appropriate color.
Attention! The richness of the color of feces, urine, and skin will indicate a dangerous concentration of bilirubin in the human body. Normal urine should be clear yellow, not dark yellow or red. The stool should not be black. The skin should be pink, not yellow.
Features of biochemical blood analysis
Reliability of analyzes is the basis of quality treatment. The patient needs to know how to take a liver test and strictly follow the rules. It is also important to have an understanding of how liver samples are taken.
A biochemical blood test is carried out on an empty stomach, before radiography, ultrasound, otherwise the interpretation of liver tests changes, even if the indicators are normal. The period of abstinence from food is 8–12 hours. Tea, coffee, even without sugar, alcohol are prohibited, water is allowed.
Fatty foods should also be excluded. The time is selected in the morning - liver test results may fluctuate throughout the day.
More than two hours should pass between smoking and donating blood. If the patient is taking medications that cannot be stopped, the attending physician must be informed. Physical activity on the eve of the analysis, as well as psycho-emotional stress, can prevent reliable interpretation of liver tests due to incorrect results.
Blood is drawn from a vein, after which the formed elements are separated from the serum by centrifugation. The manipulation is performed using a disposable needle and mandatory treatment of the puncture site with an antiseptic.
Hemolysis (destruction of red blood cells) and chylosis (fat particles) in the blood serum interfere with the quality of the test. The results of liver tests and blood tests in general cannot be deciphered; the material must be re-taken.

Changes in the course of the disease are reflected in the data of liver blood tests; this allows you to monitor the dynamics of the disease and evaluate the effectiveness of therapy.
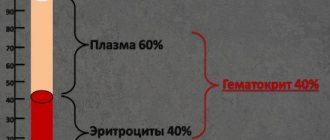
Blood plasma volume
By 6-12 weeks of pregnancy, blood plasma volume increases by approximately 10-15%. The fastest rate of increase in blood plasma volume is observed in the period from 30 to 34 weeks of pregnancy, after which plasma volume changes slightly. On average, blood plasma volume increases by 1100-1600 ml per trimester, and as a result, plasma volume during pregnancy increases to 4700-5200 ml, which is 30 to 50% higher than plasma volume in non-pregnant women.
During pregnancy, plasma renin activity tends to increase, while the level of atrial natriuretic peptide decreases slightly. This suggests that the increase in plasma volume is caused by vascular insufficiency, which is caused by systemic vasodilation (dilation of blood vessels throughout the body) and an increase in vascular capacity. Since it is the volume of blood plasma that initially increases, its effect on the renal and atrial receptors leads to opposite effects on hormonal levels (a decrease in plasma renin activity and an increase in natriuretic peptide). This hypothesis is also supported by the observation that increasing sodium intake does not further increase plasma volume.
After delivery, plasma volume decreases immediately but increases again after 2–5 days, possibly due to increased aldosterone secretion occurring at this time. Plasma volume then gradually declines again: at 3 weeks postpartum it is still elevated by 10-15% relative to the normal level for non-pregnant women, but is usually completely normal by 6 weeks postpartum.
Which doctor should I contact?
Biochemical research is sometimes carried out on healthy people - for example, during preventive examinations. But most of the blood tests that determine the indicators of the liver complex are prescribed to identify their deviations from the norm if there are corresponding patient complaints.
The issues of diagnosis and treatment of diseases in which liver tests are elevated are dealt with by doctors such as a therapist, an infectious disease specialist, a hepatologist, and a surgeon. Before sending the patient to the laboratory, he should be familiarized with the rules for taking tests and warned about the consequences that violating them may have.
Liver tests are elevated for various reasons; Individual consideration of each case is required.
Deciphering a blood test for liver tests is possible, as a rule, within a few hours or the next day after donation - it depends on the time of blood sampling, the range of tests, their complexity and the technical capabilities of the laboratory.
The attending physician explains exactly which liver test parameters differ from the norm and develops a plan for further examination and treatment.
Hematological complications during pregnancy
- Iron-deficiency anemia.
- Thrombocytopenia.
- Neonatal alloimmune thrombocytopenia.
- Acquired hemophilia A.
- Venous thrombosis.
- Rh and non-Rh alloimmunization. For diagnosis, an analysis is performed for Rh antibodies and anti-group antibodies.
- The manifestation of a previously unrecognized disorder of the coagulation system, such as von Willebrand disease, most often manifests itself in women during pregnancy and childbirth. To screen for von Willebrand disease, a test is performed to evaluate platelet aggregation with ristocetin.
- Aplastic anemia.
Tags:
complete blood count, anemia, pregnancy, iron, platelets, erythrocytes, leukocytes
Back to section