Editor
Anna Sandalova
Pulmonologist, doctor of the highest category
Diagnosis of pneumonia, in addition to a clinical examination and chest x-ray in children, includes various types of tests, ranging from a simple blood test to a PCR test to determine specific pathogens.
In the article below, we will briefly review diagnostic methods and dwell in detail on changes in the general blood count and ESR index characteristic of pneumonia.
We urge you not to self-medicate and consult a doctor in a timely manner! Please do not use the described treatment regimens without consulting a doctor - it is dangerous to your health!
Types of research
Parents know their child well and therefore, at the slightest change in his general condition, they begin to worry. And in some cases you should take a closer look at the baby. Pneumonia is caused in 90 out of 100 cases by bacteria (for example, streptococcus or chlamydia), and in 10 by viruses and fungi.
You need to go to a clinic to diagnose pneumonia if you have several symptoms, which are presented in detail in this article.
Any diagnosis of pneumonia contains two types of research - laboratory tests and radiation diagnostics.
Laboratory tests include the following diagnostic procedures:
Sputum examination
- clinical blood test;
- Analysis of urine;
- blood biochemistry;
- sputum microscopy.
The following procedures are included in radiation diagnostics:
- X-ray examination;
- fluorography;
- fluoroscopy;
- tomography.
In this case, the appointment of one or another diagnostic procedure is carried out depending on the age of the child and the severity of the disease.
Online test for pneumonia detection
Complexes with this research
Examination during pregnancy.
3rd trimester 5,730 RUR Composition Male anti-aging diagnostics Monitoring of basic indicators in men aged 40+ 8,210 RUR Composition
Entry into IVF Examination when a woman enters the IVF procedure RUB 15,030 Composition
IN OTHER COMPLEXES
- Advanced anti-aging diagnostics in postmenopause RUR 20,420
- Expanded hospital complex 4,520 RUR
- Your immunity RUR 2,040
- Future dad 5,370 RUR
- Iodine deficiency RUB 1,370
Features depending on age
Children under 3 years are a special category of patients, and in order to diagnose them with pneumonia, you need to follow this plan:
- Visual assessment of the baby's current condition.
- A complete, careful examination by a pediatrician, tapping the chest and listening with a phonendoscope. A qualified doctor will determine whether a baby has pneumonia without tests. Also, in most cases, the doctor additionally prescribes laboratory tests.
- Clinical (general blood test) is a standard diagnosis.
- Analysis of urine. It is carried out to diagnose the condition of the kidneys and the severity of intoxication.
- Bacteriological blood test.
- Study of the composition of a child's sputum.
Expert opinion

Lyudmila Sokolova
Pediatrician, doctor of the highest category
Ask a Question
If the presence of community-acquired pneumonia is suspected, as well as if there are symptoms of mild pneumonia in a child under 3 years of age, X-ray diagnostics is not a mandatory study.
children aged 4 to 10 years undergo standard measures: listening to the lungs with a phonendoscope, blood tests (general clinical, biochemical and bacteriological), urine, and sputum. When, after passing these tests, difficulties in diagnosis are observed, there are suspicions of complications and signs of a severe course of the disease, children of this age are prescribed an X-ray examination.
Starting from the age of 10, all diagnostic procedures are allowed.
Sputum examination is carried out only in older children. It is difficult to collect sputum from babies because they swallow it. Using this diagnostic method, the number of neutrophils, red blood cells, and fibrin is determined. In this way, you can find out what was the cause and causative agent of the disease. But this research result cannot be called sufficiently informative, since when collecting sputum there is a high probability of bacteria and microbes entering from the oral cavity or bronchi.
Treatment of pneumonia
Treatment of pneumonia is aimed at suppressing the infection and preventing complications.
People with community-acquired pneumonia can usually be treated at home with medications. Most symptoms disappear after a few days or weeks, but the feeling of fatigue may persist for a month or more. Specific treatments depend on the type of pathogen and the severity of the pneumonia, the age and general health of the patient. Options include:
Antibiotics . These medications are used to treat bacterial pneumonia. Typically, a broad-spectrum antibiotic is prescribed before receiving the results of a microbiological examination. It may take time to determine the type of bacteria causing pneumonia and choose the appropriate antibiotic to treat. If the patient's condition does not improve, usually within 2-3 days, the antibiotic is changed.
Cough medicines . Because coughing helps clear phlegm from the lungs, you shouldn't completely eliminate the cough. Additionally, you should know that very little research has been done on the effectiveness of over-the-counter cough medications. If you decide to take a cough suppressant, use the smallest dose possible to help you rest. Special mention should be made of expectorant drugs, which facilitate the passage of sputum and do not suppress the cough reflex.
Antipyretics/Painkillers . You can take them as needed to reduce fever and chest discomfort due to pleural pain. These include drugs such as paracetamol, aspirin, ibuprofen and other anti-inflammatory drugs.
Indicators and standards
When diagnosing pneumonia in children, an important point is a blood test. For example, knowing the indicators of leukocytes and lymphocytes, you can determine the etiology of the disease: viral or bacterial.
The most significant in diagnosing pneumonia are serological, biochemical and general blood tests. Let's look at each of them in more detail.
Determination of the etiology of the disease by blood parameters
Serological
Allows you to quickly identify microorganisms and infectious agents in cases where the results of other tests are called into question. It is done quite rarely. It is used to diagnose atypical pneumonia caused by chlamydia or mycoplasma. This study makes it possible to determine what was the source of the disease and correctly prescribe a course of antibiotics for treatment.
Polymerase chain reaction (PCR)
This test is the most effective tool for identifying atypical pathogens and viruses (mycoplasma, chlamydia). The study allows you to determine the DNA of any microorganism. The advantage is the ability to quantify the microbe in the body and the ability to detect several infections or viruses at once.
Enzyme-linked immunosorbent assay (ELISA)
Unlike PCR, this test does not detect viral agents or bacteria, but measures the amount of antibodies produced by the human immune system. Antibodies, in turn, fight the pathogen. For example, in the first 10 days of illness, the test shows the presence of class “M” immunoglobulins, later with the development of the disease – class “A”. A protracted course of infection may be indicated by the body’s production of class “G” immunoglobulins.
Biochemical
It is of great importance in diagnosing the disease. Blood biochemistry indicators are nonspecific, but enable the doctor to determine the severity of the inflammatory process and the functional activity of internal organs during pneumonia.
It is important to pay attention to the following blood parameters:
- Total protein. In the normal state of the body, the protein content is 65-85 g/l. With pneumonia, it does not increase or decrease and is within acceptable limits.
- Alpha and gamma globulin . The value of these indicators significantly exceeds the norm. This is evidence that the body is fighting inflammation.
- Fibrinogen. Slightly exceeds the norm.
- C-reactive protein . This indicator is above the norm.
- Lactate dehydrogenase (LDH) . The presented figure is slightly higher than normal.

Biochemical blood test standards
General blood analysis
The CBC has the greatest diagnostic value and contains the following indicators:
- Leukocytes. If bacterial pneumonia is present, the white blood cell count will be higher than normal. With viral pneumonia, there is a significant decrease in the number of leukocytes (leukopenia). In children, the leukocyte norm depends on age. For newborns - 9.2-13.8 x 10 to 9 degrees U/l, from one year to 3 years 6-17 x 10 to 9 degrees U/l, from 3 to 10 years - 6.1-11.4 x 10 to the 9th degree U/l.
- Leukocyte formula and its shift. When the disease is caused by bacteria, pronounced granular neutrophils are found in the blood. A significant amount of their immature (band) forms indicates bacterial pneumonia. This is the so-called shift of the leukocyte formula to the left. When there are few neutrophils in the blood and more lymphocytes than normal, this indicates the viral nature of pneumonia in a child.
- Red blood cells. With a mild course of the disease, their slight decrease is possible; with a more severe degree of pneumonia, the number of red blood cells is increased. The norm of erythrocytes for children up to one year is 4-5.3 x 10 to the 12th power g/l, from one to three years old – 3.7-5.3 x 10 to the 12th power g/l, up to 12 years – 3.7 -5.0 x 10 to 12 degrees g/l
- Lymphocytes. With a reduced number of lymphocytes, we can talk about the bacterial nature of pneumonia.
- Platelets. With pneumonia, they are within acceptable limits characteristic of age.
- Erythrocyte sedimentation rate (ESR).
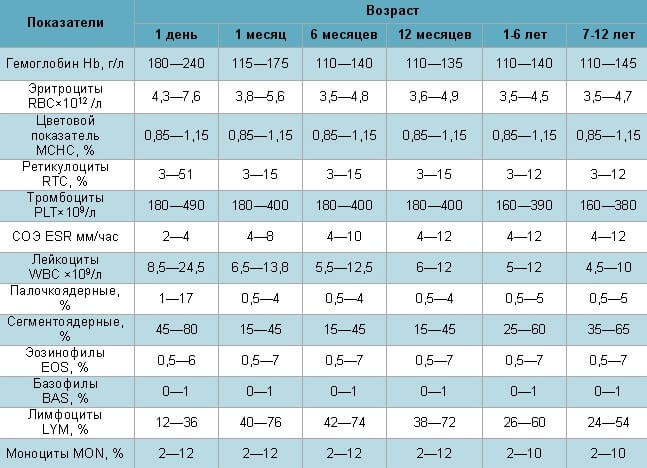
Norms of general blood test in healthy children
Erythrocyte sedimentation rate (ESR) - norm and deviation
In acute pneumonia, one of the most important signs of the presence of the disease in a child’s body is the erythrocyte sedimentation rate.
In children, this indicator varies depending on age. An increase in ESR is one of the most characteristic signs of pneumonia. At the same time, the erythrocyte sedimentation rate in the child’s blood is increased and can exceed 30 mm/h .
For comparison, ESR norms in children depending on age are as follows:
- for newborns – 2-4 mm/h;
- children under one year old - from 3 to 10 mm/h;
- children aged from one to 5 years - from 5 to 11 mm/h;
- children aged 6-14 years - from 4 to 12 mm/h.
Lifestyle and Home Remedies
These tips will help you recover faster and reduce the risk of complications:
Take more time to relax . Do not return to school or work until your temperature is normal and your coughing has stopped. Be careful even when you start to feel better: since pneumonia can recur, it is best not to return to daily work until you have fully recovered. In all actions, consult your doctor.
Drink plenty of fluids , especially water.
Take your medications as prescribed by your doctor. Until complete recovery.
Sources and reference materials
| # | File | file size |
| 1 | Diagnosis and treatment of community-acquired pneumonia. Infectious Diseases Society of America Guidelines | 833 KB |
| 2 | Diagnostic algorithms and protocols for providing medical care for pneumonia | 3 MB |
| 3 | Clinical guidelines for the diagnosis and treatment of acute respiratory diseases (ARI), treatment of pneumonia in children | 990 KB |
| 4 | Laboratory and instrumental standards | 145 KB |
| 5 | Laboratory standards (blood, biochemical, feces, respiratory function, etc.) | 218 KB |
| 6 | Diagnosis of respiratory diseases. Hams | 9 MB |