What fluids are examined when testing for mycoplasma?
Blood and urine are used to examine the patient's body. During PCR, you can take almost any liquid. But blood gives a clearer picture. This diagnosis allows you to identify the presence of microorganisms at the genetic level. The results are as accurate and reliable as possible. There is no need to retake material.
ELISA requires blood sampling from a vein. It is done in the morning and on an empty stomach. If the results reveal immunoglobulins, this confirms the course of the disease in an acute form. These antibodies may appear half a month after the onset of the disease. They remain in the body, even if the patient is completely cured.
Blood is taken in the morning; the patient should not eat the day before. The collected portion cannot be stored for a long time. It should not be cooked or exposed to low temperatures. Only fresh liquid provides data that most fully confirms the presence of the disease.
Urine allows you to determine the presence of bacteria in the body. This liquid is used in a diagnostic method such as culture. The number of microbes and the body's response to antibiotics can be determined. The finished result is released only after two weeks. The collected material must be transported to the laboratory under special conditions. This requires liquid nutrient media (sucrose phosphate, with the addition of agar).
How does a person become infected with ureaplasmosis?
The source of infection is a patient with ureaplasma infection or a carrier of ureaplasma. You can get infected in several ways:
- Antenatal
- intrauterine. Up to 23% of unborn children become infected from sick mothers. - Intrapartum
- infection during childbirth. Only 50% of newborns have a chance to remain healthy. Once in the genital tract of a newborn, ureaplasma can remain there in an inactive state for an unlimited time. If there is a normal microflora - a kind of physiological barrier, the infection does not manifest itself in any way. - Contact-household
- this happens very rarely, since the pathogens are not viable in the external environment. And yet, this is possible if the microorganism is in humid, warm conditions, with poor air access, for example, in a public shower that is not cleaned or ventilated. Slippery walls, slimy from dampness, which do not get hot water, are very reminiscent of the conditions in the body. - Sexual
is the main route of infection. A sick person can infect a healthy partner during sexual intercourse. Most often, carriers of ureaplasmosis are women.
Infection is not yet a disease, but already a carrier state. Those. a person is already capable of infecting sexual partners.
How to test for mycoplasma
Laboratory cultures are taken by taking material from the urethra in men and the vagina in women. Or they use the material in the form of a morning urine sample. The patient comes to the laboratory. He collects a portion of liquid in advance. It would be better if it was the middle part. It will give a more correct result. Sometimes doctors recommend taking both a smear and urine. This way you can get a more complete picture of the disease.
Blood tests are performed only on an empty stomach. It is better if the patient does not eat after nine in the evening the night before. Do not drink alcoholic beverages or take antibiotics for at least one month. In general, there are no special requirements for preparing for the study. The blood must be fresh. Otherwise, the survey results will give a distorted picture. ELISA and PCR examinations are carried out simultaneously.
Treatment of ureaplasmosis
If ureaplasma is detected, treatment is carried out if the microbe is the cause of chronic inflammation, infertility, etc. If the cause of the disease is ureplasma, treatment is prescribed with antibiotics. The choice of antibiotic should be made by a doctor, since self-medication of ureaplasmosis often not only does not bring the desired result, but can also lead to the development of microbial resistance to the antibiotic. Thus, over the past few years, the number of tetracycline-resistant strains of Ureaplasma urealyticum and parvum has been increasing.
Of particular importance is the treatment of ureaplasma (parvum, urealiticum) in men and women when planning pregnancy. The decision to treat ureaplasma parvum and others during pregnancy is made taking into account its duration, as well as after carefully weighing the possible risks for the child and mother from ureaplasma and antibiotic therapy. Usually, they try to treat ureaplasma during pregnancy at a later stage (after 20 weeks), when the effect of antibiotics on fetal development becomes minimal.
Indications for testing for mycoplasma
As soon as the patient detects signs of the disease, he should immediately undergo examination. Symptoms may appear due to:
- Contact with an unfamiliar partner without the use of protective equipment;
- Miscarriage;
- Infertility;
- A woman is pregnant;
- Manifestations of pain in the form of a mild sexually transmitted infection. It becomes clearly expressed in any stressful situation.
In women, the disease can manifest itself in heavy vaginal discharge. The body experiences an unpleasant itching and burning sensation the next time you pass urine. During sex, pain appears in the abdominal area. In a pregnant woman, the disease can lead to miscarriage or premature birth.
Men feel nagging pain in the lower abdomen. Transparent discharge comes out of the urinary canal. If the appendages are affected, then redness of the skin around the testicle is observed. Pain occurs between the perineum and in the scrotum area.
Preparation for PCR research
A test for ureaplasma is taken from women in the middle of the menstrual cycle, and not before the start of menstruation or after its end, as with a bacteriological smear. To obtain a reliable result of a PCR study, you must adhere to simple rules:
- Before taking the test, it is prohibited to treat with antibiotics;
- 2 days before the study, stop using local medications and contraceptives;
- wash themselves the evening before the test without using soap, and in the morning before the test, intimate hygiene and douching with antiseptic solutions are prohibited;
- 2 days before the study, sexual activity is completely excluded;
- it is forbidden to urinate for 3 hours before taking the test;
- It is not recommended to do a smear immediately after taking colposcopic samples to determine cervical tumors.
Blood tests for mycoplasma
Laboratory blood testing for this type of disease gives a more complete result. This liquid is used as a starting material for diagnostic procedures such as PCR, ELISA. The first refers to the most effective and modern methods. It identifies a section of bacterial DNA found even in small quantities. This analysis can determine the presence of infection in the body, even if the patient does not experience pain.
Ready results are obtained within a day. This method is so accurate that there is no need to donate blood again. Diagnostics will immediately give a 100 percent result. Inaccuracies can only arise if the research technology is violated.
Enzyme-linked immunosorbent assay (ELISA) does not detect bacteria. It can be used to find antibodies that arise upon contact with pathogens. Diagnostics allows you to determine the form of the disease (acute or chronic). The results can be 80 percent accurate. Because sometimes antibodies produced can arise during another infection.
Definition of research
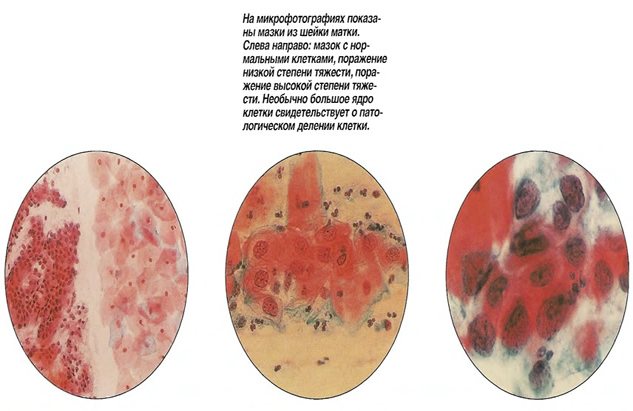
A smear is a collection of cells from the mucous membrane of a certain organ for the purpose of diagnosing infectious diseases.
To study the collected material, various laboratory diagnostic methods are used, which make it possible to identify the causative agent of the infection:
- microscopy of bacteriological smear;
- PCR method;
- cultural sowing.
How long does it take to test for ureaplasmosis? The period required to obtain results depends on the research methodology. The fastest way is smear microscopy. However, its results are preliminary and are not used to make a final diagnosis. The choice of method for determining ureaplasma in a smear is made by a doctor depending on the clinical situation.
Urethral smear for mycoplasma
This type of analysis makes it possible to identify only one type of mycoplasma - hominis. Material from men is taken from Urerta. Nutrient media are used for sowing. Then you need to cultivate the microorganisms for several days. Then the identification process occurs. The degree of sensitivity of bacteria to drugs of antimicrobial nature is determined.
Based on the culture, the doctor can count the number of pathogens. The degree of the disease and the extent of the damage are determined. The picture that appears during treatment with certain antibiotics is revealed. Such an analytical study gives a hundred percent probability of correct data. The patient receives the finished result in at least five days, and sometimes he has to wait longer.
Tests for mycoplasma after treatment
After a course of treatment procedures, you should not take control tests immediately. You need to wait at least a month. And only then make an appointment. Post-treatment examination can be carried out in the following forms:
- Bacteriological culture;
- Blood testing using PCR;
- Serological diagnostic method;
The first diagnosis is the most likely. It makes it possible to compare the initial results and data obtained from the study at the end of treatment. The degree of reduction in the percentage of bacteria is determined. Since the body does not develop a protective barrier for such microorganisms, special attention should be paid to improving immunity in general.
Polymer chain diagnostics are carried out very rarely. Because the material taken for research may not reveal bacteria. Instead of real microorganisms, DNA from dead particles can be taken. ELISA may also not give correct results. Immunoglobulins can be present in the body of a healthy person for a long time. The patient will struggle with a disease that no longer exists.
Symptoms of sexually transmitted diseases:
- Discharge from the urethra
- Vaginal discharge
- Itching in the vagina
- Discharge from the genitals
- Pain in the scrotum
- Pain when urinating
- Itching in the urethra
- Blood in sperm
- Itching of the vulva
- Pus on the labia
- Burning in the urethra
- Perineal pain
- Redness of the glans penis
- Frequent urination
- Itching of the glans penis
- Itching of the scrotum
- Rectal prolapse
- Foreskin rupture
What happens if you don’t get tested on time and delay treatment?
Timely detection and treatment of sexually transmitted infections is the key to sexual health, quality sexual life and fertility.
Long-term presence of ureaplasma in the genitourinary tract can lead to chronic urethritis, prostatitis, vesiculitis, epididymitis in men, which is accompanied by the development of pelvic pain, impotence and infertility. Also, with a deep disturbance of the microflora of the skin of the glans penis, the development of chronic balanoposthitis is possible.
Women most often develop severe vaginal dysbiosis, bacterial vaginosis and inflammation of the cervical canal and fallopian tubes, leading to difficulties in childbearing, painful menstruation and discomfort during sexual intercourse.
Deciphering the analysis for mycoplasma
As a result of decoding laboratory results, the following conclusions may be:
- Negative;
- Positive;
- Asymptomatic carrier status.
In the first case, all norms for the presence of microbial elements on one tampon indicate a complete absence of disease. The second confirms the presence of clinical signs of inflammation. The organs of the reproductive system are affected by this disease. The course of the disease in an asymptomatic form is expressed in the third formulation. To obtain more accurate results, you need to undergo not one type of examination, but several studies.
Culture for Ureaplasma species with determination of titer and sensitivity to antibiotics
A microbiological study that allows one to identify ureaplasma in biomaterials and determine their sensitivity to antibiotics.
When microbiological methods detect microorganisms that constitute normal microflora or opportunistic microorganisms in a titer less than the diagnostic one, sensitivity to antibiotics and bacteriophages is not determined, since this amount is not significant and does not require treatment with antimicrobial drugs.
Synonyms Russian
Ureaplasmosis, ureaplasma infection, parvum, T-960, mycoplasmosis.
English synonyms
Ureaplasma species culture, bacteria identification and susceptibility.
Research method
Microbiological method.
What biomaterial can be used for research?
Urogenital smear, single portion of urine, ejaculate, prostate secretion.
How to properly prepare for research?
- Women are recommended to take a urogenital smear or urine before menstruation or 2 days after its end.
- Men should not urinate for 3 hours before submitting a urogenital smear or urine test.
General information about the study
Ureaplasmas are microorganisms that can parasitize the membrane of sperm and the epithelium of the mucous membrane of the genitourinary organs. They belong to the transient microflora of the genitourinary system. They are distinguished from other mycoplasmas by the presence of urease activity, that is, the ability to break down urea into ammonia, which is where their name comes from. Ureaplasmas include U. Urealyticum and U. Parvum, the term U. species is used to refer to both species. The route of transmission is predominantly sexual; in addition, contact and household transmission is possible, as well as vertical - from a sick mother to a child during pregnancy or childbirth. The source of infection is a patient with ureaplasma infection or a carrier of ureaplasma.
Infection does not necessarily lead to disease. The development of infection is facilitated by various immunodeficiencies (including vaginal dysbiosis in bacterial vaginosis in women or impaired production of prostatic antimicrobial factor in men with chronic prostatitis), impaired local defense factors, as well as concomitant infections (chlamydia, gonorrhea, bacterial vaginosis, etc.). ).
The incubation period is 2-5 weeks. Clinical symptoms of ureaplasma infection may be mild or even absent (typical for women).
In men, ureaplasmas can cause inflammation of the urethra (non-gonococcal urethritis), bladder (cystitis), prostate (prostatitis), damage to the testicles (orchitis) and their appendages (epididymitis), as well as a violation of the composition of sperm - a decrease in motility and sperm count, which threatens infertility . Sometimes reactive arthritis and urolithiasis develop.
In women, ureaplasma can cause inflammation of the vagina (vaginitis), cervix (cervicitis), as well as its neoplasms. When the immune system is weakened, inflammation of the uterus (endometritis) and its appendages (adnexitis) is possible, which leads to damage to the fallopian tubes and the development of adhesions in them. This contributes to ectopic pregnancy or infertility. In addition, ureaplasmas lead to cervical insufficiency, miscarriages, chorioamnionitis, the birth of children with low body weight (less than 2500 g), as well as bronchopulmonary diseases (pneumonia, bronchopulmonary dysplasia), bacteremia and meningitis in newborns.
Ureaplasma (U. species) can be considered as a cause of inflammatory diseases of the genitourinary system if laboratory testing does not reveal other pathogenic microorganisms that can cause these diseases. In this case, the method of cultivation on nutrient media (seeding) is used. In 80% of cases with ureaplasma infection, mycoplasma, chlamydia and anaerobic flora are also detected.
What is the research used for?
- To establish the cause of chronic inflammatory diseases of the genitourinary system.
- For differential diagnosis of diseases that occur with similar symptoms: chlamydia, gonorrhea, mycoplasma infection.
- To select rational antibacterial therapy and evaluate its effectiveness.
- For preventive examination.
When is the study scheduled?
- If a ureaplasma infection is suspected, including after casual sexual intercourse, with symptoms of inflammation of the genitourinary system.
- When planning a pregnancy (for both spouses).
- For infertility or miscarriage.
- With an ectopic pregnancy.
- If necessary, evaluate the effectiveness of the ongoing antibacterial therapy (on the 10-14th day after discontinuation of the drug).
What do the results mean?
Reference values: no growth.
Positive result
The detection of ureaplasma in large quantities (more than 104 CFU/ml) in combination with clinical signs of inflammation of the genitourinary system in the absence of other pathogenic microorganisms indicates the presence of ureaplasma infection and that it was the cause of the inflammation.
A small amount of ureaplasma, not more than 104 CFU/ml, provided that there are no symptoms of the diseases they cause, is regarded as carriage.
Negative result
The absence of ureaplasma growth in the culture indicates the absence of ureaplasma infection.
What can influence the result?
Previous antibacterial therapy.
Important Notes
- People at increased risk of developing ureaplasma infection include people who have multiple sexual contacts, pregnant women, smokers, women taking oral contraceptives, and people with low socioeconomic status.
- When planning pregnancy for prevention, a woman should be examined for ureaplasma infection, since treatment of this disease with antibiotics during pregnancy, especially in the early stages, is dangerous. It adversely affects the fetus and can lead to miscarriage.
- Culture for ureaplasma does not allow determining its type. It is possible to distinguish U. urealyticum from U. parvum only using PCR testing.
Also recommended
- Ureaplasma species, DNA quantitative [real-time PCR]
- Ureaplasma parvum, DNA [real-time PCR]
- Ureaplasma urealyticum, DNA [real-time PCR]
- Ureaplasma urealyticum, IgA, titer
- Ureaplasma urealyticum, IgG, titer
- Chlamydia trachomatis, DNA [real-time PCR]
- Mycoplasma genitalium, DNA [real-time PCR]
- Mycoplasma hominis, DNA [real-time PCR]
- Spermogram
- Microscopic examination of prostate secretion (microflora)
- Microscopic examination of the discharge of the genitourinary organs of men (microflora)
- Microscopic examination of discharge from the genitourinary organs of women (microflora)
Who orders the study?
Obstetrician-gynecologist, urologist, venereologist, pediatrician-neonatologist, infectious disease specialist.
Literature
- Karamova A. E. The significance of Ureaplasma urealyticum and Mycoplasma genitalium as causative agents of inflammatory diseases of the urogenital tract / A. E. Karamova, A. V. Polyakov, I. V. Khamaganova // Klin. microbiol. antimicrobial chemotherapy – 2004. – T. 6, No. 4. – P. 365-370.
- Khaldin A. A. Urogenital chlamydia and ureaplasmosis: diagnostic issues and new treatment options / A. A. Khaldin // Infections and antimicrobial therapy. – 2004. – No. 3. – P. 93-95.
- Kenny GE Genital Mycoplasmas: Mycoplasma genitalium, Mycoplasma hominis, and Ureaplasma Species. In: Principles and practice of infectious disease / GL Mandell, Bennett JE, Dolin R (Eds) ; 6th ed. – Churchill Livingstone, Philadelphia, PA 2005. – 2701 p.
- Non-chlamydial non-specific genital infection. In: Oxford handbook of genitourinary medicine, HIV, and Aids / R. Pattman [et al.] (Eds) ; 1st edition. – USA: Oxford University Press, 2005 – 580 p.
- Ureaplasma urealyticum intrauterine infection: role in prematurity and disease in newborns / GH Cassell // Clin. Microbiol. Rev. – 1993. – Vol. 6, N 1. – P. 69-87.
- Larsen B. Mycoplasma, Ureaplasma, and adverse pregnancy outcomes: a fresh look / B. Larsen, J. Hwang // Infectious Diseases in Obstetrics and Gynecology. Electronic journal. – Vol. 2010. – Article ID 521921.
Where to get tested for mycoplasma
Clinical laboratories today operate in many private clinics, which allows their patients to undergo examination without wasting time. In addition, many even offer their patients additional services, for example, home visits or anonymous testing.
You can find out where the clinic closest to your home or work is located, when it opens and what services it provides, on the website of the “Your Doctor” service. It also supports a feedback function, and you can call a doctor or make an appointment with him using a special form on the website.
Publication date: 2020-01-27
Useful information on the topic:
- Calling a venereologist to your home
- Venereal diseases
- Syphilitic rash
- Discharge from the genitals
- How does a consultation with a venereologist work?
- Wart removal
- Removal of condylomas
- Tests for STIs
- Removal of papillomas
- Cervical smear
- Urethral swab
- Genital warts
- Mushroom tests
- Diagnosis of sexually transmitted infections
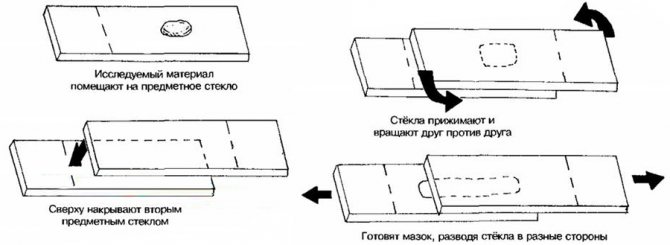
Bacteriological smear
A smear for ureaplasmosis is taken in the presence of an inflammatory process on the mucous membrane of the vagina or urethra. How is a smear taken? To do this, the gynecologist first inserts a speculum into the vagina. The manipulation itself is not painful, but causes the woman minor discomfort. During the procedure, the patient’s breathing should be calm and deep, and the vaginal muscles should not be strained. This will help reduce discomfort.
Where do they get the material for analysis? Using a sterile probe, a smear is made from 3 places: from the mucous membrane of the cervical canal of the cervix, vagina and urethra. The doctor applies the material taken in this way onto a glass slide. The smear is stained with a special paint and examined under a microscope. Each type of bacteria gets its own shade.
A bacteriological smear from a healthy patient reveals not only beneficial microorganisms, such as lactobacilli, but also a small amount of streptococci, staphylococci, and fungi. Such indicators are considered to be the norm. The presence of an infectious disease is indicated by a change in the composition of the vaginal microflora and the presence of inflammatory processes in the genital area.