Indications for cardiac scintigraphy
Doctors can recommend cardiac scintigraphy both to patients who have already identified certain heart pathologies, and to patients for whom it is impossible to make a diagnosis due to lack of information. After receiving the results, the doctor will plan further treatment tactics and determine the diagnosis. It is worth noting that this method can act as both primary and additional.
First of all, representatives of the risk group for developing IHD (coronary heart disease) should think about undergoing a heart scintigraphy procedure as a preventive measure:
- long-term heavy smokers;
- people with high cholesterol;
- patients with hypertension and/or diabetes;
- men over 45 years of age and women over 55 years of age.
This diagnosis is prescribed in situations where it is necessary to assess the effectiveness of the prescribed course of treatment as accurately as possible. In addition, the study is recommended for athletes before competitions and patients who are scheduled for surgery or other manipulations on the heart.
Scintigraphy is also prescribed to patients who have had a heart attack, because the technique allows you to assess the performance of the heart muscle. Angina pectoris is also an indication for scintigraphy.
Very often people complain of pain of unknown origin in the chest area. Most people do not pay attention to this, although this may be the first signal of the development of a dangerous heart disease. Doctors recommend that when the first such symptoms appear, immediately contact a specialist who will most likely give you a referral for heart scintigraphy, because this technique is the most informative and reliable. Today, scintigraphy in Moscow is done in almost every large medical center, so no one should have problems finding a suitable institution.
Single-photon emission computed tomography of the myocardium is a radionuclide research method designed to assess the blood supply to the myocardium at the microcirculation level. The method is based on assessing the distribution of intravenously administered radiopharmaceuticals in the heart muscle, which is incorporated into intact cardiomyocytes in proportion to coronary blood flow. Areas of the myocardium with normal blood supply create a picture of uniform distribution of radiopharmaceuticals, and areas of myocardium with a relative or absolute decrease in blood flow due to ischemia or scar damage have a decrease in the inclusion of radiopharmaceuticals due to perfusion defects.
The distribution of radiopharmaceuticals in the myocardium depends both on the perfusion itself and on the integrity of the sarcolemma and the preservation of cellular metabolism (viability). Due to the similarity in the distribution of potassium in the myocardium and the radiopharmaceuticals used, it is possible to combine the assessment of early and delayed inclusion of radiopharmaceuticals. The early distribution pattern is proportional to blood flow, while the late distribution pattern indicates tissue with an intact intra-extracellular gradient, allowing differentiation between viable and nonviable (scar, necrosis) myocardium.
Among radiopharmaceuticals labeled with 99mTc, the most widely used is MIBI, known in foreign literature as Sestamibi, which, like potassium, enters cardiomyocytes through the K-Na-ATP pump. Myocardial viability is determined by increased isotope accumulation both on delayed images and upon repeated administration. Areas of viable myocardium are characterized by so-called semistable perfusion defects. They are characterized by the return of the myocardial image to normal on late delayed scintigrams and after reinjection of radiopharmaceuticals at rest. If the area of hypoperfusion persists, then this zone corresponds to non-viable areas of the myocardium. A number of studies have shown the high informative value of perfusion scintigraphy in combination with a pharmacological test with dobutamine in assessing the presence of viable myocardium.
The most common method used to verify viable myocardium is the administration of the synthetic beta-1 adrenergic agonist dobutamine, which in small doses (5-10 mcg/kg/min) can increase the contractility of viable myocardium without significantly increasing heart rate. Single-photon emission computed tomography of the myocardium performed with a dobutamine test assesses the degree of myocardial viability and the sensitivity of the scintigraphy method (from 89% to 100%).
Figure 1-3 shows scintigraphic studies of the myocardium of a 58-year-old patient who was hospitalized at the Republican Scientific and Practical Center "Cardiology" with a diagnosis of CHF and atherosclerosis of the heart vessels. SPECT of the myocardium was performed according to a one-day protocol with a stress pharmacological test with dobutamine, then 3 hours later SPECT of the myocardium at rest (Fig. 1-2). When analyzing the information obtained after the administration of dobutamine, it is determined that there is an uneven accumulation of radiopharmaceuticals throughout the myocardium of the left ventricle with varying degrees of percentage in the segments of the heart muscle. Perfusion of the medial-basal section of the posterior, lateral wall and interventricular septum of the myocardium of the left ventricle shows signs of severe ischemia of 20% of the myocardium of the entire left ventricle with severe impaired perfusion, respectively, in the Rightcoronary arteries basins 49% with severe impaired perfusion and 10% of the aperfusion zone.LeftCircumflex 46.5 % and LeftanteriorDescending 0.1%
Fig. 1 SPECT of the myocardium of a 58-year-old patient with a pharmacological test with dobutamine
When repeated after 3 hours at rest, an increase in the percentage of hypoperfusion zones in the left ventricular myocardium is observed. 34.5% of the myocardium of the entire left ventricle with severe perfusion impairment, respectively, in the Rightcoronary arteries basins 81.7% with severe perfusion impairment and 10% of the aperfusion zone. Left Circumflex 51% and Left anterior Descending 10.9%.
Rice. 2 SPECT of the myocardium of a 58-year-old patient with CHF at rest.
Subsequently, CABG surgery was performed, and after 6 months, SPECT of the myocardium was performed (Fig. 3) at rest there was no noticeable increase in the percentage of hypoperfusion zones in the myocardium of the left ventricle. The total amounted to 22.7% of the myocardium from the entire left ventricle with severe perfusion impairment, respectively, in the Rightcoronary arteries basins 58.1% with severe perfusion impairment and 10% of the aperfusion zone. Left Circumflex 26.6% and Left anterior Descending 3.4%.
Rice. 3 SPECT of the myocardium of a 58-year-old patient after CABG
The test we used for diagnostic purposes with the pharmacological drug dobutamine (dipyridamole) with SPECT allows us to identify areas of viable myocardium.
RADIONUCLIDE DIAGNOSTICS IN THE STUDY OF MYOCARDIAL FUNCTIONAL STATE
Thanks to the development of new highly informative computer technologies, modern non-invasive radionuclide research methods are widely used in cardiology today. The development and improvement of radionuclide methods for studying the cardiovascular system was facilitated by both the development of radiopharmaceuticals (RPs) with a specific affinity for healthy or ischemic myocardium, and devices that present information about the passage of the indicator not only in graphical, but also in visual form. The main device in radionuclide diagnostics is the gamma camera created in 1963 by H. Anger.
The progressive development of nuclear cardiology is due to the creation of gamma tomographs with high counting speeds and the use of computer technology for collecting and processing information. In cardiology, radionuclide research methods are aimed at studying:
- state of intracardiac hemodynamics, aorta, large vessels with assessment of the nature of blood flow in them;
- myocardial perfusion with assessment of its local disorders;
- contractile function of the myocardium;
- determination of regional metabolic activity of the myocardium.
Of the radionuclide methods for assessing the functional state of the myocardium, the most widely used in world practice today are radionuclide tomoventriculography (RTVG), perfusion single-photon emission computed tomography of the myocardium (SPECT) and positron emission tomography (PET).
Single photon emission computed tomography of the myocardium (SPECT).
A special place among the methods of nuclear medicine is occupied by perfusion single-photon emission computed tomography of the myocardium (SPECT), which allows one to obtain unique information about the blood supply to the myocardium at the level of microcirculation and has been used in world practice for more than 20 years.
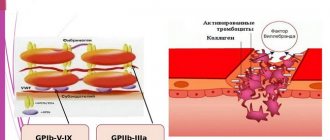
Myocardial SPECT is a radionuclide research method based on assessing the distribution of intravenously administered radiopharmaceuticals in the myocardium, which occurs in proportion to coronary blood flow. Myocardial SPECT is designed to identify areas of relative or absolute reduction in blood flow resulting from ischemia or scar damage to the myocardium. To visualize myocardial perfusion, radiopharmaceuticals are used, which are extracted and retained by the myocardium for various time intervals.
Currently, the following radiopharmaceuticals are used: thallium chloride (201Tl), 99mTc-MIBI (2,4,methoxyisobutyl isonitrile, Russian-made Technetril, Cardiolite USA) and 99mTc-TF (tetrofosmin), 99mTc-TEBO (teboraxim) .
The use of 201Tl is based on its biological similarity to potassium; after intravenous administration, it quickly leaves the bloodstream and enters cells in quantities proportional to the initial blood flow. About 4% of the administered dose penetrates the myocardium for some time, and thanks to this, the heart is clearly visible against the background of low background lung activity. 99mTc-MIBI is intensely concentrated in sympathetic nerve receptors, and since the myocardium is well innervated by sympathetic fibers, a decrease in the inclusion of 99mTc-MIBI in them is an indicator of myocardial dysfunction.
Local disturbances of myocardial perfusion during single-photon emission computed tomography are assessed by the percentage of radiopharmaceutical accumulation in myocardial segments or on a 4-point scale of a 13–20 segmental model of the LV: in this case, the LV is divided into 13–20 segments along four walls: anterior, lateral , lower and septum, and 3 regions: apex, middle third and base (Fig. 1.).
Rice. 1. Perfusion 17-segment map.
When analyzing local contractility disorders, 0 points are assessed as normal accumulation of radiopharmaceuticals, 1 point - slightly reduced accumulation of radiopharmaceuticals with uptake of more than 75% of the maximum inclusion in the myocardium, 2 points - from 50 to 75% of inclusion of the isotope, 3 points - significantly pronounced perfusion defects less than 50%, 4 points – from 0 to 25% inclusion of the isotope (scar zones).
Myocardial perfusion scintigraphy is performed at rest and in combination with various stress tests, which are necessary to identify the arterial basin that is not able to provide an adequate increase in coronary blood flow in response to an increase in cardiac work.
Indications for the use of myocardial perfusion SPECT.
Since the distribution of radiopharmaceuticals in the myocardium occurs in proportion to the coronary blood flow and its inclusion in intact cardiomyocytes is a reflection of the normal blood flow of the myocardium and there will be a uniform image of the distribution of radiopharmaceuticals in the LV. A reflection of the limitation of blood flow and ischemic or scar damage to the heart muscle will be a decrease in the distribution of radiopharmaceuticals in a particular area of the myocardium, a perfusion defect.
Thus, myocardial perfusion scintigraphy makes it possible to determine the presence, localization, extent and severity of cicatricial or ischemic damage to the myocardium, the functional significance of the anatomical lesion of the coronary arteries identified during angiography, and to assess the viability of the myocardium.
With the help of myocardial perfusion scintigraphy it is possible to:
- diagnosis of atherosclerotic lesions of the coronary arteries (presence, localization, prevalence);
- assessment of the degree of coronary artery stenosis and its effect on regional myocardial perfusion;
- assessment of myocardial viability (ischemic or scar changes, prediction of improved function after revascularization);
- assessment (prognosis) of the degree of risk in patients: after myocardial infarction, for preoperative assessment of the degree of risk before major surgical interventions in patients with a high risk of developing coronary complications;
- monitoring and evaluation of treatment effectiveness after: coronary revascularization; drug therapy for heart failure or angina, and lifestyle changes.
Stress tests are most often used in combination with myocardial perfusion SPECT.
The use of stress testing significantly increases the sensitivity, specificity and accuracy of diagnosing coronary artery disease. Physical stress tests and pharmacological tests are used as stress tests. In patients with reduced coronary blood flow due to impaired vascular reactivity or stenotic damage, an area of reduced radiopharmaceutical concentration is determined in the zone of reduced perfusion. If a zone of reduced radiopharmaceutical concentration appears or increases when administered during exercise or after the administration of positive inochronotropic adrenergic drugs (compared to rest), then ischemia is the likely cause. If the zone of reduced radiopharmaceutical concentration does not change either during exercise or at rest, the most likely cause of this should be considered cicatricial damage to the myocardium.
Myocardial perfusion scintigraphy in combination with exercise testing (EST).
It does not differ significantly from the conventional PFN protocol used for cardiac ECHO. It is necessary to observe precautions and clearly know the contraindications for the test. In the absence of contraindications to the test, if patients are receiving drug therapy, then β-blockers are canceled 48-72 hours before, long-acting nitrates and calcium antagonists are canceled 24 hours before. When studying the effectiveness of treatment, it is carried out against its background.
PFN is usually performed on a bicycle ergometer or on a treadmill. For patients with expected high tolerance to physical activity, the initial power is selected in advance so that the total time of physical activity does not exceed 12-15 minutes. During the study, ECG and blood pressure are recorded. When the criteria for stopping the test are reached, a radiopharmaceutical is administered intravenously, after which the patient continues to perform physical activity for another 2 minutes. to achieve an ischemic equilibrium state, the so-called ischemicsteadystate. If an attack of angina occurs that is not relieved by rest, if possible, a radiopharmaceutical is administered before taking nitroglycerin and other antianginal drugs to eliminate the ischemia-masking effect. When performing PFN in the absence of reliable criteria for a positive test, it is important to achieve a heart rate of at least 120-135 beats/min.
Myocardial perfusion scintigraphy in combination with pharmacological tests.
When conducting pharmacological tests, the following drugs are used:
a) drugs that cause vasodilation and lead to coronary hyperemia (dipyridamole and adenosine);
b) positive ino-chronotropic adrenergic drugs (dobutamine and arbutamine) in order to increase the myocardial oxygen demand. The vasodilatory effect of dipyridamole during a pharmacological test is associated with an increase in the content of extracellular adenosine and prostacyclin, resulting in a decrease in the tone of small myocardial arteries and arterioles and coronary vascular resistance, the peak of which occurs after 2-5 minutes. after intravenous administration of dipyridamole.
Dipyridamole is administered intravenously slowly at a dose of 0.56 mg/kg over 4 minutes. with the patient lying on his back. The radiopharmaceutical is administered intravenously until the test termination criteria are reached. In the absence of indications for immediate relief of the effect of dipyridamole, euphilin is administered no earlier than 5 minutes after administration of the radiopharmaceutical. Please note that side effects may occur within 30 minutes. after administration of dipyridamole.
Tests with dipyridamole or adenosine should not be performed in patients with a history of bronchospasm, pulmonary disease (bronchial asthma and pulmonary hypertension), intubation for severe pulmonary pathology, severe hypotension (systolic blood pressure less than 90 mmHg), severe valvular heart disease and hypersensitivity to adenosine and dipyridamole, and should not be administered to patients constantly taking methylxanthines for broncho-obstructive syndrome, patients with II-III degree ativentricular block or sick sinus syndrome, with AMI less than 2 days old, unstable angina with the last attack that occurred not more than 48 hours before the start of the study.
When using drugs that increase myocardial oxygen demand as a stress test in clinical practice, preference is given to dobutamine, a synthetic catecholamine with a pronounced effect on β1-receptors and a weak effect on α- and β2-adrenergic receptors. When using small doses of dobutamine (up to 10 mg/kg/min), a clear positive inotropic effect is observed due to stimulation of β1 and β receptors. When using high doses (20-40 mg/kg/min), heart rate progressively increases due to stimulation of β1-adrenergic receptors. In this case, systemic blood pressure increases slightly due to an increase in cardiac output, and peripheral resistance decreases. In areas of the myocardium supplied with blood from arteries with critical stenosis, due to inadequate blood flow in conditions of increased myocardial oxygen demand, regional ischemia occurs, detected by scintigraphy. In this case, in order to assess myocardial viability, dobutamine is used in small doses (up to 20 mg/kg/min), and for myocardial ischemia - in large doses (up to 40 mg/kg/min).
Tests with inochronotropic drugs should not be performed in patients with ventricular tachyarrhythmias, in the early period of MI, unstable angina, or obstructive hypertrophic cardiomyopathy.
Myocardial perfusion scintigraphy in combination with transesophageal electrical stimulation of the atria (TEES).
PPES is a safe alternative to PFN. TEES is performed with the patient lying on his back until the heart rate reaches 160 beats/min or until the criteria for stopping stimulation appear, after which a radiopharmaceutical is administered intravenously. In the absence of clinical and ECG criteria for myocardial ischemia, the duration of TEES at the last stage is about 2 minutes. After cessation of stimulation, heart rate almost immediately returns to its original value and signs of myocardial ischemia decrease or disappear quickly. Therefore, when performing TEES in combination with myocardial perfusion SPECT, stimulation after administration of radiopharmaceuticals is continued for at least 3 minutes.
Limitations of the test include side effects such as burning or painful pulsation in the epigastric region, or in the lower third of the sternum; it is contraindicated in patients with diseases of the esophagus.
Precautions when performing myocardial perfusion scintigraphy in combination with pharmacological tests.
Stress tests are performed in radionuclide departments equipped with a set of instruments and drugs for resuscitation measures; the studies should; carried out in the presence of a doctor who has undergone special training in resuscitation measures. Constant monitoring of hemodynamic parameters (blood pressure and heart rate) and recording of a 12-lead ECG are required.
Application of myocardial SPECT
The sensitivity of the SPECT method with 99mTc-MIBI and 201Tl for diagnosing CAD using stress tests is more than 90%. This method can be used not only to diagnose myocardial ischemia, but also to determine the functional significance of coronary artery stenosis or collateral flow detected by angiography. Another important application of this study is to assess the prognosis of patients with acute myocardial infarction, since this method can reveal not only the degree of perfusion impairment, but also the extent of scarring associated with previous myocardial infarctions. SPECT with 99mTc-MIBI and 201Tl is especially informative in the management of patients receiving cardiac glycosides with bundle branch block, i.e. in those cases, standard exercise testing fails to perform ST segment analysis.
The ability of SPECT with 99mTc-MIBI to predict long-term outcomes of the disease in patients who have suffered acute myocardial infarction, the so-called risk stratification of coronary syndrome, has been proven.
The use of SPECT with 99mTc-MIBI with a dobutamine test in the diagnosis of post-infarction LV aneurysm reveals not only the presence of an aneurysm, but also viable myocardium in the “transitional” ischemic zone.
The information content of myocardial scintigraphy with 99mTc-MIBI or 201Tl and echocardiography, performed in combination with the administration of low doses of dopamine, has been proven to identify viable myocardium in areas of post-infarction cardiosclerosis and predict the restoration of their contractility after revascularization. The sensitivity of detecting myocardial viability in areas of akinesia using echocardiography and SPECT with 99mTc-MIBI, performed at rest and in combination with a dopamine test, is 85% and 92%, respectively. Consequently, perfusion SPECT is not only a highly informative method for determining the degree and extent of circulatory disorders in the myocardium, but also allows one to determine the viability of dyssynergistic (hibernating) myocardium.