Scintigraphy (radionuclide diagnostics) is a modern method of radiation diagnostics, which is used to assess the functioning of various organs and tissues. Diagnostic methods such as X-ray, ultrasound, CT or MRI are focused on identifying structural changes in the tissues of the body, and are not always able to distinguish the disease in its early stages, when deviations manifest themselves at the level of biochemical changes in the tissues. At this time, scintigraphy comes to the rescue, which is why it is called molecular diagnostics. Radionuclide research methods are indicated for diseases of the heart, brain, kidney and liver diseases, and are also an indispensable method in identifying and assessing the prevalence of oncological processes.
Benefits and preparation for scintigraphy:
An advantageous difference between scintigraphy and other diagnostic methods is the recognition of the pathological process in the early stages of the disease, i.e. before the disease had time to manifest itself.
Information about the function of the organ and obtaining quantitative characteristics of the degree of its damage at the earliest stages.
In most cases, scintigraphy does not require special preparation, and the only contraindication to scintigraphy is pregnancy.
The radiopharmaceutical administered during the study usually does not cause any side effects, and the radiation exposure during scintigraphy is comparable to radiographic studies.
Contraindications
Mammoscintigraphy should not be performed on pregnant, nursing mothers, or patients whose weight exceeds 120 kg.
A contraindication to manipulation is any severe condition of the patient that prevents him from being placed in the tomograph or remaining still during scanning.
Scintigraphy is a safe procedure with high diagnostic value. It helps to identify foci of malignant cells long before the first symptoms of the disease appear. Some women refuse examination for fear of radiation exposure. You can't do this. Without a full examination, it is impossible to select the optimal therapeutic course and stop tumor growth. Modern gamma tomographs do not harm humans. The radiopharmaceutical is quickly and painlessly removed from the body without causing damage.
has been organizing high-quality individual medical care for many years.
Over the years of work, we have accumulated statistics on leading foreign clinics and are ready to recommend that patients undergo examination by a mammologist only those medical centers where the best specialists work.
How is scintigraphy performed in Moscow?
Scintigraphy is performed according to modern protocols and clinical guidelines of the European Society of Nuclear Medicine (EANM) and the Society of Nuclear Medicine and Molecular Imaging (SNMMI).
A small amount of a radioactively labeled substance is injected into the patient's blood, which accumulates in damaged or healthy tissues.
The accumulation is recorded by a special sensitive device - a gamma camera.
The gamma camera creates a “photographic” image of the human organs that have accumulated the injected drug.
The injected substance is practically safe for the patient, does not cause allergic reactions and is quickly eliminated from the body after the study, which ensures minimal radiation exposure. The procedure for scanning skeletal bones and other organs is comfortable and painless.
The procedure itself, from the administration of the radiopharmaceutical drug to the start of the scintigraphic study, takes from 30 minutes to 3 hours, depending on the type of study. This is necessary so that the injected substance is distributed throughout the human body. The study is analyzed by qualified specialists, radiologists, who work with each patient individually. If necessary, the results of the study are consulted by the staff of the Department of Radiation Diagnostics and Therapy of the Russian National Research Medical University (RNMU) named after. N.I. Pirogov in Moscow, which is located on the basis of the department. A conclusion based on the results of scintigraphy is issued on the day of the study.
You can examine almost any organ, including the bones of the skeleton, and the examination can be done in several ways. With a clearly defined task and continuous feedback between the radiologist and the doctors of the clinical departments, the possibilities of scintigraphy are almost limitless, and assistance in making complex diagnoses is invaluable, while the price of the examination is affordable for every patient.
About radionuclide VISUALIZATION (scintigraphy) for a general practitioner
The first use of radioactive tracers dates back to 1911 and is associated with the name of György de Hevesy. A young scientist living in a cheap boarding house began to suspect that the leftover food that he did not finish was being served to him again the next day. He added a radioisotope tracer to the uneaten portion and, using a radiation detector, proved to his mistress that this was the case. The hostess kicked the young scientist out of the boarding house. He continued the work he had begun, which resulted in the Nobel Prize for the use of radionuclides as indicators in biology. Radionuclide (radioisotope) diagnostics covers all types of applications of discovered radioactive substances for diagnostic and therapeutic purposes.
The clinical use of radiotracers came into practice in the 50s. Methods are being developed that make it possible to detect the presence (radiometry), kinetics (radiography) and distribution (scanning) of a radiotracer in the organ under study. A fundamentally new stage in radioisotope imaging is associated with the development of devices with a wide field of view (scintillation gamma cameras) and a visualization method - scintigraphy. Often the term “scintigraphy” refers to studies performed using both a linear scanner and a scintillation gamma camera. This terminological stereotype is associated with the formation of misconceptions about the diagnostic capabilities of the methods.
Scanning and scintigraphy are different radioisotope imaging techniques. Scintigraphy is significantly superior to scanning in terms of volume and accuracy of diagnostic information. Modern scintillation cameras are computer-scintigraphic complexes that allow obtaining, storing and processing images of an individual organ and the entire body in a wide range of scintigraphic modes: static and dynamic, planar and tomographic. Regardless of the type of image obtained, it always reflects the specific function of the organ being examined. Essentially, it is mapping functioning tissue. It is in the functional aspect that the fundamental distinguishing feature of scintigraphy from other imaging methods lies. An attempt to look at the results of scintigraphy from an anatomical or morphological point of view is another false stereotype that affects the expected effectiveness of the method.
The diagnostic focus of a radioisotope study is determined by the radiopharmaceutical drug (RP) used. What is RFP? A radiopharmaceutical is a chemical compound with known pharmacological and pharmacokinetic characteristics. It differs from conventional pharmaceuticals not only in its radioactivity, but also in another important feature - the amount of the main substance is so small that when introduced into the body it does not cause side pharmacological effects (for example, allergic ones). The specificity of the radiopharmaceutical in relation to certain morphofunctional structures determines its organotropy. Understanding the mechanisms of radiopharmaceutical localization serves as the basis for adequate interpretation of radionuclide studies. The administration of a radiopharmaceutical is associated with a small dose of radiation, which is unable to cause any adverse specific effects. In this case, it is customary to talk about the danger of overexposure, but this does not take into account the pace of development of modern radiopharmaceuticals.
Radiation exposure is determined by the physical characteristics of the radiotracer (half-life) and the amount of radiopharmaceutical administered. The present day of radionuclide diagnostics is the use of short-lived radionuclides. The most popular of these is technetium-99m (half-life 6 hours). This artificial radionuclide is obtained immediately before the study from special devices (generators) in the form of pertechnetate and is used to prepare various radiopharmaceuticals. The amounts of radioactivity administered for one scintigraphic study create radiation exposure levels within 0.5-5% of the permissible dose. It is important to emphasize that the duration of the scintigraphic study, the number of images or tomographic sections obtained no longer affect the “given” radiation dose.
l Clinical application
Let us briefly look at the real diagnostic capabilities of the most common (“routine”) scintigraphic studies.
Visualization of the skeletal system (osteoscintigraphy) is the most accurate method for identifying areas of impaired bone metabolism. Osteotropic radiopharmaceuticals (Tc-phosphonates) have a high affinity for calcium phosphate crystals, so they bind predominantly to the mineral component of bone tissue. The level of accumulation of radiopharmaceuticals in various types of bones and areas of the skeleton is determined by the degree of osteoblastic and metabolic activity, the amount of blood flow, which must be taken into account when differentiating normal and pathological accumulation of radiopharmaceuticals. In particular, increased accumulation of radiopharmaceuticals is observed in the metaepiphyseal sections of long bones, in areas with constant physical activity.
Bone diseases are accompanied by pathological reorganization of bone tissue, reactive or tumor bone formation - the main mechanisms causing changes in bone metabolism and the accumulation of osteotropic radiopharmaceuticals in the affected areas. Depending on the combination of these processes, the level of accumulation of osteotropic radiopharmaceuticals increases in tumor, inflammatory, degenerative, and traumatic diseases.
The main and most important task of osteoscintigraphy is the search for metastatic and assessment of the prevalence of tumor lesions of the skeleton. Scintigraphic manifestation of pathology may appear 3-12 months earlier than radiological signs appear. This is due to the fact that local changes in the exchange of osteotropic radiopharmaceuticals occur in the early phases of the development of pathology, even before the appearance of not only radiological, but also clinical symptoms. For this reason, radionuclide testing is most effective in the pre- and postoperative examination of patients with tumors with a high frequency of bone metastases (breast, lungs, prostate, kidneys).
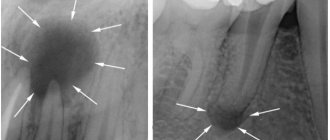
| Figure 1. Osteogenic sarcoma of the thigh. Extensive area of high radiopharmaceutical accumulation in the distal left thigh |
Scintigraphic manifestation of metastatic lesions is multiple and, less often, single local zones of high accumulation of radiopharmaceuticals (“hot” foci). The highest concentrations of radiopharmaceuticals are observed in osteoblastic and mixed metastases, low - in osteolytic ones. False-positive errors are most often associated with pronounced osteodystrophic changes, as well as traumatic injuries to the ribs and spine. Bone tumors of osteogenic origin have the highest accumulation of radiopharmaceuticals. For example, osteogenic sarcoma is characterized by pronounced hyperfixation of radiopharmaceuticals not only in the elements of the tumor itself, but also in the surrounding soft tissues due to reactive hyperemia (Fig. 1). In tumors of non-osteogenic origin, the accumulation of radiopharmaceuticals is lower. However, it is practically impossible to differentiate individual types of tumors according to the degree of accumulation of radiopharmaceuticals in them. Some tumors, as well as their metastases, can be an accumulation of radiopharmaceuticals. These tumors include, in particular, reticulosarcoma and multiple myeloma. Visualization of the kidneys (dynamic renoscintigraphy) is a simple and accurate method for simultaneous assessment of the functional and anatomical and topographical state of the urinary system. It is based on the registration of transport of nephrotropic radiopharmaceuticals and the subsequent calculation of parameters that objectify two successive stages.
Analysis of the vascular phase (angiophase) is aimed at assessing the symmetry of the passage of the “bolus” through the renal arteries and the relative volumes of blood entering each kidney per unit time. Analysis of the parenchymal phase involves characterizing the relative function of the kidneys (contribution to the total cleansing capacity) and the time of passage of radiopharmaceuticals through each kidney or its parts. Clinical interpretation is largely determined by the mechanism of radiopharmaceutical elimination. In dynamic visualization methods, two types of radiopharmaceuticals can be used: l glomerulotropic (DTPA derivatives), almost completely filtered by the glomeruli and reflect the state and rate of glomerular filtration; l tubulotropic (hippuran analogues) are secreted by the epithelium of the proximal tubules and reflect the state of tubular secretion, as well as effective renal blood flow. Indications for the study include urological and nephrological pathologies, as well as diseases where the kidneys are the target organs.
In different clinical situations, both the shape of the curves and their quantitative characteristics may change. It should, however, be emphasized that the nature and magnitude of changes are not very specific for a particular pathology and primarily reflect the severity of the pathological process. Renoscintigraphy is most informative when differentiating unilateral or bilateral kidney damage.
The leading sign that determines the side of the lesion is the asymmetry of the amplitude-time characteristics of angio-onephroscintigrams. Asymmetry of vascular parameters, and above all, a pronounced difference in the time of arrival of radiopharmaceuticals into the renal arteries, is one of the criteria for renal artery stenosis. The symmetry of changes in parenchymal function is more typical, in particular, for glomerulonephritis; asymmetry is a fairly constant sign of pyelonephritis not only with unilateral, but also with bilateral process. Similar changes may accompany various types of anomalies of the kidneys and upper urinary tract (nephroptosis, duplication of the collecting system, hydronephrosis).
The liver imaging method (hepatoscintigraphy) is based on the use of labeled colloids, which, after intravenous administration, are phagocytosed and distributed in morphofunctional structures containing RES cells in accordance with the local values of organ blood flow. Normally, more than 90% of the administered radiocolloid is localized in the liver, about 5% in the spleen, and less than 1% in the bone marrow. Depending on the nature and severity of the pathology, these ratios change. The most common indication for hepatoscintigraphy is hepato- and/or splenomegaly of unknown origin. The main objective of the study is to differentiate the nature and clarify the severity of liver damage.
Diffuse liver diseases are manifested by changes in the size and shape of the image, the distribution of radiocolloid in the liver and its extraorgan accumulation, parameters of the phagocytic ability of the RES and hepatic blood flow. It should be emphasized that the study does not allow differentiation of clinical or clinical-morphological forms of liver disease (for example, chronic hepatitis). The greatest information content of the method is manifested in the possibility of identifying portal hypertension syndrome (PH).
| Figure 2. Extrahepatic portal blockade. Portal hypertension syndrome is manifested by high uptake of radiocolloid by an enlarged spleen. |
Regardless of the causes of increased pressure in the portal vein system (intra- or extrahepatic forms), scintigraphic SPH is manifested by high uptake of radiocolloid and an enlarged spleen. The combination of these signs makes it possible to identify SPG with an accuracy of up to 98% (Fig. 2). Focal liver lesions, depending on their extent, are manifested by the presence of single or multiple defects in the accumulation of radiopharmaceuticals within one or both lobes of the liver (Fig. 3). In practice, the identification of areas where there is no accumulation of radiopharmaceuticals (“cold” foci) is often strongly associated with volumetric processes, most often of tumorigenesis. This idea is false. A fairly wide range of diseases associated with the involvement of the liver in the pathological process can be scintigraphically manifested by focal changes as a consequence of local hemodynamic or functional disorders (liver cirrhosis, amyloidosis, histiocytosis). It is also necessary to remember that some organ structures (abnormally located gallbladder, mammary gland) can “screen” the image of the liver and form the scintigraphic phenomenon of “pseudotumor”. That is why, based on the nature of the radiopharmaceutical accumulation defect, without taking into account clinical information, it is almost impossible to differentiate the specificity of the focal lesion.
| A. | B. |
| Figure 3. Scintigraphic variants of nodular lesions of the thyroid gland. The “cold” node of the lower part of the left lobe is a colloid cyst (A), the “hot” node of the right lobe is a thyrotoxic adenoma (B) | |
The ability to detect focal pathology also depends on the resolution of the gamma camera. Lesions smaller than 1 cm, as a rule, are not manifested scintigraphically.
Visualization of the biliary system (hepatocholescintigraphy) is based on the use of a series of hepatotropic radiopharmaceuticals, similar in their pharmacokinetics to dyes (bromsulfalein, vofaverdine). After intravenous administration, they bind to blood proteins, are absorbed by polygonal liver cells and are excreted as part of bile. The main advantage of hepatocholescintigraphy is the continuity of visual and quantitative recording of the process of radiopharmaceutical kinetics.
Visual analysis of a series of images allows us to identify some organic changes in the bile ducts (dilation), gallbladder (deformations), as well as functional changes in the duodenum.
Analysis of the curves allows us to obtain quantitative criteria characterizing the absorption-excretory function of the liver, the filling of the gallbladder, the duration of the latent period after a choleretic breakfast, and the rate of emptying of the gallbladder. Dyskinesia of the gallbladder is differentiated based on changes in the rate of its emptying (hypo- or hypermotor dyskinesia). It should be emphasized that the accuracy of radiological assessment of the motor function of the gallbladder exceeds that of x-ray or echography. This is due to the fact that when comparing image areas of an organ before and after a fixed time after a choleretic breakfast, it is almost impossible to take into account the duration of the latent period of bile secretion and to identify the actual phase of gallbladder emptying.
Hepatocholescintigraphy has limited value in the diagnosis of inflammatory pathology and gallstones. The primary task is to assess the severity of the obstruction of the cervical duct zone and the filling of the gallbladder. When the cystic duct is completely obstructed, the scintigraphic phenomenon of a “disconnected gallbladder” occurs.
Imaging of the thyroid gland (thyroid scintigraphy) is carried out using Tc-pertechnetate and is based on the similarity in the behavior of iodine ions and pertechnetate. However, this similarity can be traced only in the initial inorganic phase of intrathyroidal transport. Pertechnetate, unlike iodine, does not enter the organic phase, that is, it is not included in the composition of thyroid hormones. This feature excludes the possibility of its use in the postoperative search for metastases of thyroid cancer (the latter is carried out only with radioactive iodine).
Nodular lesions of the thyroid gland and differential diagnosis of clinically or sonographically identified nodular formations of the neck are the most common indication for thyroid scintigraphy. The main objective of the study is to assess the degree of functioning of the nodes, identify solitary or multiple formations, and establish the connection of the nodes with the thyroid tissue. Depending on the functional activity and degree of accumulation of radiopertechnetate, nodes are traditionally divided into “hot”, “warm” and “cold”. However, this division applies only to their scintigraphic assessment.
The term “hot” node refers to a situation where radiopharmaceuticals accumulate almost exclusively in the area of the node and do not accumulate in other parts of the organ. Similar findings are typical for autonomous thyroid tissue, toxic adenoma, autoimmune thyroiditis, and congenital lobe aplasia. The lack of accumulation of radiopharmaceuticals in the surrounding tissue node is explained by the production of thyroid hormones by the autonomous node, which reduce the release of TSH and cause suppression of the function of normal tissue.
Functionally inactive (“cold”) nodes are characterized by the absence or sharp decrease in the accumulation of radiopertechnetate. This less specific finding accompanies a wide range of pathologies: nodular goiter, colloid cysts, adenoma, nonspecific strumitis, and in 15-25% of cases - thyroid cancer (Fig. 3).
The greatest difficulty is in identifying “warm” nodes. These nodes are considered a type of “hot”, but unlike the latter, they lack or have weakly expressed functional suppression of normal thyroid tissue. Because of this, the accumulation of radiopharmaceuticals in the nodes may not differ from the surrounding parenchyma and lead to false-negative interpretations of scintigraphy data.
Indications and contraindications for the study
Skeletal bone scanning is recommended in the following cases:
- to identify oncological pathologies with bone metastasis;
- for diagnosing fractures and tumor processes in bones;
- as a monitoring method for the dynamics of treatment;
- to identify areas with altered bone tissue during dystrophic processes.
Also, scanning the skeleton bones is indispensable if radiography could not detect cracks, fractures and other bone injuries.
Indications
Scintigraphy in Moscow is considered as a clarifying study and is usually prescribed at the final stage, after using radiography, ultrasound and other diagnostic methods. The purpose of scintigraphy is to assess the topography, shape and size of the organ, determine the exact location, structure and functional activity of pathological foci. The technique is used at the stage of clarifying the diagnosis, during differential diagnosis, when drawing up a plan for conservative and surgical treatment and in the process of assessing the effectiveness of treatment measures.
Skeletal bone scintigraphy is performed to assess the structure of bone tissue and identify pathological foci in joints, long bones, vertebrae, pelvic bones, sternum, shoulder blades and skull bones. The procedure allows you to detect areas of intense growth, degeneration or restructuring. Scintigraphy is indicated for suspected metastatic bone lesions in malignant tumors of various locations, rheumatic lesions, degenerative processes, inflammatory changes and difficult to diagnose fractures.
Scintigraphy of the gastrointestinal tract is carried out to study the structure and topography of hollow and parenchymal organs, to determine the functional ability of hollow organs, as well as to assess the nature, size and shape of pathological foci. Various types of static and dynamic scintigraphy are performed for dysphagia, suspected primary and metastatic neoplasms, intestinal obstruction, intestinal bleeding, diffuse liver damage (cirrhosis, hepatitis), cholelithiasis, as well as after operations on various parts of the gastrointestinal tract.
Lung scintigraphy is performed to assess regional ventilation and pulmonary capillary blood flow. The procedure is prescribed after a chest x-ray. The study is indicated for suspected pulmonary embolism, atelectasis, pneumosclerosis, pneumonia, neoplasms, obstructive processes and other pathological conditions.
Scintigraphy of the kidneys and adrenal glands is carried out to assess the structure and functional state of organs located in the retroperitoneal space. Static renal scintigraphy is prescribed to study the state of the renal parenchyma, localization, size and shape of organs, dynamic - to study the excretory function of the kidneys. Static studies are rarely carried out due to their insufficiently high information content. Adrenal scintigraphy in many cases is also not informative enough and is used mainly to identify hormone-producing tumors.
Vascular scintigraphy is used to study the structure and patency of veins and lymphatic vessels. The study can be either static or dynamic. The technique allows you to evaluate the speed of blood and lymph flow, the condition of blood vessels and lymph nodes. Indications for scintigraphy are lymphostasis and chronic venous insufficiency of various origins. In addition, the procedure is performed if lymphogenous metastasis of malignant neoplasms is suspected.
The advantages of performing scintigraphy with us:
Our department is equipped with a single-photon emission computed tomograph combined with an X-ray computed tomograph, which allows us to conduct studies of almost all human organs and systems, including skeletal scanning, obtaining cross-sectional images of organs for precise localization of the pathological process.
Each report is prepared by two doctors of the department (the “double reading” method), if necessary, with the involvement of employees of the Department of Radiation Diagnostics and Therapy of the leading medical university of Russia - RNRMU named after. N.I. Pirogov.
The conclusion is issued on the day of the study, usually within 40-60 minutes after completion of the study.
If necessary, images in additional projections or SPECT are taken free of charge.
A modern department, built according to modern building and sanitary standards, equipped with a waiting room before the examination, will ensure the comfort of the procedure, whether it is scanning the skeleton or any other organ.
Scintigraphy"
Types of research
There are many types of scintigraphy used to identify the pathology of various organs and systems. The following types of studies are most widely used in clinical practice:
- Skeletal bone scintigraphy
- Scintigraphy of the gastrointestinal tract, including the stomach and esophagus, intestines, pancreas, liver, gall bladder
- Lung scintigraphy
- Scintigraphy of the kidneys and adrenal glands
- Vascular scintigraphy
Along with the listed methods, the patient may be prescribed scintigraphy of the thyroid gland, parathyroid glands, salivary glands, myocardium, brain, spleen and other organs. There are also special techniques used to detect certain types of tumors, to facilitate subsequent surgery, etc. For example, somatostatin receptor scintigraphy is used to detect tumors with a large number of somatostatin receptors, and sentinel lymph node scintigraphy is performed to place an isotope tracer before surgery intervention.
How's it going?
The radiopharmaceutical is usually administered intravenously. After this, you need to wait for several hours until the radionuclides spread throughout the body through the bloodstream. The person is then placed on a special table and scanned.
During the manipulation, you need to lie still so that the resulting image is clear. The doctor evaluates the images, determining which areas of accumulation are characteristic of the norm, and which may be the result of tumor degeneration, trauma or other processes.
Patient preparation
The list of preparatory measures is determined by the type of scintigraphy. Before conducting a study of skeletal bones, it is necessary to refrain from taking bismuth and barium preparations for 4 days. You need to take with you the results of radiography, CT or MRI of bone structures (if available). Before thyroid scintigraphy, you should undergo an ultrasound of the thyroid gland, take a hormone test, not eat seafood for 2 weeks and not take hormonal medications for 1 month. Before examining the lungs, you need to do an X-ray or CT scan of the chest.
Before examining your kidneys, you must undergo a kidney ultrasound and drink a glass of water an hour before the procedure. Scintigraphy of the biliary tract is performed strictly on an empty stomach. The doctor should provide the results of a biochemical blood test, ultrasound of the liver and gallbladder. You need to take a bottle of holosas or another similar drug with you. Liver scintigraphy is performed after liver ultrasound. Before myocardial scintigraphy, it is necessary to abstain from eating, smoking and drinking caffeine-containing drinks for 4-6 hours. The study is carried out after the ECG.
How to behave after the procedure?
Thyroid hormone T4
Thyroid scintigraphy is a safe method. It does not cause any particular negative consequences. But radiotherapy drugs are dangerous to the patient's health, since the radiation can seriously affect the cell's DNA.
To prevent complications, you must behave correctly:
- Women of reproductive age should undergo scintigraphy 20 days after the last day of menstruation. This will avoid the risk of conducting research during an unplanned pregnancy.
- The dose of radiotherapy for children is adjusted according to their body weight.
- Nursing mothers should undergo scintigraphy or suspend the lactation period.
- A person who is constantly in contact with children, pregnant or lactating women should stay away from them. The substances used for research are radioactive.