Scintigraphy is a modern method of radionuclide visualization of internal organs, which is distinguished by its informativeness and reliability of the results obtained. Scintigraphic examination is non-invasive and atraumatic. The essence of the study: a radiopharmaceutical (RP) is introduced into the human body, then tissues and organs are visualized in photographs, which make it possible to determine the condition of the organs, identify pathological changes and anatomical and topographical features.
Historical information
Gyorgy de Hevesy is the founder of scintigraphy; he received the Nobel Prize for this greatest discovery. In the mid-90s, radionuclides began to be used in medicine. Various techniques have emerged that make it possible to determine the presence of a radiotracer in organs, and monitoring its movement and distribution has become real. Scanning, radiographic testing and radiometry began to be widely used.
A completely new stage in medicine was the development of a scintillation gamma camera; decades later, this examination method began to be called scintigraphy. Many medical textbooks also contain other names for the technique, for example, gamma scintigraphy.
Features of scintigraphic research
Content:
- Historical information
- Features of scintigraphic research
- Popularity of scintigraphy
- Indications for the procedure
- How to prepare for diagnosis?
- Stages of scintigraphy
- Contraindications and adverse reactions
Scintigraphic diagnostics are carried out to find hidden pathologies in the body using radioactive substances. The drug that is introduced into the human body is called a radiotracer or radiopharmaceutical. It consists of 2 main parts: a marker (isotope) and a vector molecule. The organ or tissue being examined “absorbs” the vector (special particle). The tag performs an important function - it produces gamma rays, which are recorded by a gamma camera.
Gamma cameras can be stationary or mobile. Each of the cameras consists of: a detector, replaceable lead collimators, photomultipliers and a computer, on the monitor of which images of the distribution of a special drug in the area under study appear. The images obtained during the examination are called scintigrams.
Increased or decreased accumulation of radiotracer in a specific organ or tissue can be seen in the image. An increased amount of the drug will be indicated by “hot” foci on the scintigram, and “cold foci” indicate a reduced accumulation of the drug. Radiopharmaceuticals do not have a negative toxic effect on the patient’s well-being, since a small dose of the drug is administered.
Side effects of osteoscintigraphy
A bone scan involves the use of a radiotracer, most commonly technetium −99m, which is injected into the blood. The radiation level of the radioactive tracer is very low, much lower than that of a CT scan. The radiopharmaceutical is quickly eliminated from the body: after 1-2 days it completely leaves the body. Therefore, there are no radiation-related side effects.
There is a small risk of an adverse reaction caused by technetium-99m. After administration of the drug, the patient may experience:
- soreness or redness at the injection site;
- feeling of a strange taste in the mouth;
- chest pain or discomfort;
- cardiopalmus;
- change in odor perception.
These side effects occur in only 1% of patients. In most cases, they soon go away on their own without treatment.
Popularity of scintigraphy
Scintigraphic studies are widespread in America and European countries. In the United States, more than 17 million radionuclide studies were conducted in 2007. More than 15 million patients have successfully undergone scintigraphic diagnostics and been cured of serious diseases. In European countries over the same period (2007), specialists conducted more than 12 million studies.
Today in America more than 13 thousand gamma cameras are working properly. In the Russian Federation, scintigraphy is not as popular as in other countries. Only 200 gamma cameras were installed. In one year, about 1 million patients are sent for diagnostics.
Indications for the procedure

Radionuclide examination is prescribed for patients who have been diagnosed with congenital or acquired pathologies or chronic diseases. It is also advisable to carry out the procedure to clarify the degree of damage to internal organs and the activity of pathological foci. Scintigraphy is often performed to assess the effectiveness of the therapy.
Gamma scintigraphy is used to examine:
- lungs;
- lymphatic system;
- spinal cord and brain;
- digestive system;
- organs of the excretory system;
- heart;
- vessels;
- skeletal system...
Using the procedure, you can identify diseases: myocardial contractions, pulmonary embolism, inflammatory and infectious processes, tumors, Alzheimer's and Parkinson's diseases. Using a scintigram, a specialist will be able to see hidden diseases and changes in the thyroid gland, kidneys, liver and other vital organs.
Skeletal bone scintigraphy (osteoscintigraphy)
Scintigraphy of skeletal bones (osteoscintigraphy) is a study of metabolism (metabolism) of bone tissue using radiopharmaceuticals (RPs), which accumulate in the bones of the skeleton.
Advantages of the method : the ability to detect bone tissue pathology before the development of clinical and radiological signs of bone damage.
Indications for osteoscintigraphy:
- oncological pathologies with bone metastasis;
- diagnosis of fractures and tumor processes in bones;
- control of treatment dynamics;
- identification of areas with altered bone tissue during degenerative-dystrophic processes.
- osteomyelitis, myeloma
Preparation for skeletal bone scintigraphy: not required.
Within an hour after administration of the radiopharmaceutical, it is necessary to drink 1 liter of drinking water to improve the accumulation of the drug in the skeletal bones and reduce radiation exposure. Immediately before the test, be sure to empty your bladder.
Contraindications: Pregnancy.
Breastfeeding must be interrupted for 48 hours from the moment of administration of the radiopharmaceutical.
Features of scintigraphy of skeletal bones:
The study is carried out 1.5 to 3 hours after administration of the radiopharmaceutical. Takes from 30 minutes. The conclusion is issued on the day of the study.
Metastases of various tumors in the bone:
Many tumors metastasize to the bones. First of all, suspicion of metastatic damage to the skeleton arises in breast and prostate cancer, lung cancer, kidney cancer and some others. Particular caution should be exercised when the level of tumor markers increases, for example: PSA (prostate-specific antigen), CA 15-3 and some others. After conservative treatment or surgical removal of the tumor, dynamic monitoring of the condition of the bone tissue is recommended. Scintigraphy should be performed the first 2 times with an interval of 6-8 months, then, if the study result is normal, after 1-2 years. You should clarify the need for repeat studies with a radiologist or your attending physician.
Inflammatory and traumatic changes in bone tissue:
One of the indications for radionuclide studies of the skeletal system (bone scintigraphy) is inflammatory changes in bone tissue. The method allows you to determine the prevalence of the process by identifying foci of inflammation in the bones and joints throughout the skeleton, even in the early stages of the disease. Radiographs of osteomyelitis usually reveal a less widespread process than it actually is. Scintigraphy shows the true size of the inflammatory focus.
Osteoscintigraphy in orthopedics and vertebrology:
When replacing joints or installing metal structures in the spine, scintigraphy of the skeleton bones allows us to detect mechanical instability of the prosthesis components (looseness) or an inflammatory process around the prosthesis or metal structure. Unlike other research methods (X-ray, CT, MRI), scintigraphy of skeletal bones makes it possible to determine the intensity of the inflammatory process in various parts of the bone.
Cost of radioisotope research:
| Service code | Name of service | Cost, rub. |
| A07.03.001.001 | Whole body bone scintigraphy | 8 700 |
| A07.03.001.002 | Whole body bone scintigraphy combined with single photon emission computed tomography of bones and computed tomography of the thoracic spine | 20 500 |
| А07.03.001.003 | Whole body bone scintigraphy combined with single photon emission computed tomography of bones and computed tomography of the lumbosacral spine | 27 500 |
| A07.03.001.004 | Whole body bone scintigraphy combined with single photon emission computed tomography of bones and computed tomography of the pelvic bones | 27 500 |
| A07.03.003 | Single photon emission computed tomography of bones | 7 400 |
| A07.09.004 | Single photon emission computed tomography of the lungs (perfusion) | 14 000 |
| A07.09.004.001 | Single-photon emission computed tomography of the lungs (perfusion), combined with computed tomographic angiography of the pulmonary artery and its branches | 29 300 |
| A07.10.003 | Single-photon emission computed tomography of the myocardium at rest | 8 800 |
| A07.10.003.002 | Single-photon emission computed tomography of the myocardium, perfusion with functional tests | 15 700 |
| A07.10.005 | Single photon emission computed tomography combined with myocardial computed tomography | 18 800 |
| A07.14.002 | Scintigraphy of the liver and spleen | 9 800 |
| A07.14.002.002 | Liver scintigraphy with labeled red blood cells | 22 200 |
| A07.14.004.001 | Single-photon emission computed tomography of the liver and spleen combined with computed tomography of the hepatobiliary zone | 19 800 |
| A07.22.002 | Thyroid scintigraphy | 6 500 |
| A07.22.010 | Single photon emission computed tomography of the parathyroid glands | 9 600 |
| A07.22.010.001 | Single photon emission computed tomography of the parathyroid glands combined with computed tomography of the parathyroid glands | 29 700 |
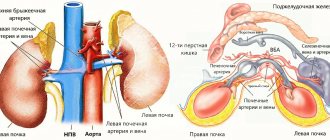
| А07.28.002 | Scintigraphy of the kidneys and urinary system | 8 700 |
| A07.28.004 | Angionephroscintigraphy | 8 000 |
| A07.30.031 | Three-phase scintigraphy of soft tissues and bones | 11 400 |
How to prepare for diagnosis?
Features of preparation depend on what kind of scintigraphy will be performed. You need to carefully prepare for the examination of the thyroid gland, skeleton, heart and lungs. The doctor often stops taking medications that can negatively affect the final diagnostic results. It is necessary to temporarily discontinue medications that accumulate and remain in tissues and organs.
When examining the thyroid gland, it is not recommended to take medications containing iodine a month before the procedure. You can eat any food during the examination of the heart, lungs, skeleton and thyroid gland. During scintigraphy, the patient should not feel hungry or thirsty, so it is advisable to eat something before starting the procedure. In order for the results of the heart study to be reliable, the gallbladder must be emptied (the patient must eat several cubes of chocolate before starting the procedure). But the organs of the gastrointestinal tract are examined exclusively on an empty stomach. You should not eat food 8-12 hours before the procedure.
Scintigraphy of the parathyroid glands
Scintigraphy of the parathyroid glands is a radionuclide diagnostic study, the purpose of which is to detect pathologically altered neoplasms (tumors, hyperplasias, adenomas), indicate their location and clarify violations of their functional activity.
Today, scintigraphy of the parathyroid glands is considered to be one of the most effective diagnostic methods, which is based on the use of radiopharmaceuticals, which have the unique ability to selectively accumulate in the tissue structure of the organ under study.
The information content of scintigraphy is an order of magnitude higher than other examination methods.
Indications for parathyroid scintigraphy
Indications for parathyroid scintigraphy are those situations where accurate diagnostic information is required:
- Osteoporosis of unknown origin;
- Formation of kidney stones;
- The patient has elevated levels of parathyroid hormone;
- Suspicions of the presence of abnormalities in the development of the gland, as well as adenoma, hyperplasia, organ carcinoma, etc.;
- Treatment planning for hyperparathyroidism.
How is scintigraphy performed?
Before conducting a study of the parathyroid glands using the scintigraphy method, no special preparation is needed, and there is no need for the patient to follow any diet or refuse to take medications on the eve of the procedure.
The only thing that the doctor may require is not to take iodine-containing medications several days before the planned procedure - this is important so that the results of the study are the most informative.
During the procedure, an isotope is introduced into the patient’s body, which produces radiation that is recorded on special equipment.
The radiopharmaceutical administered to the patient is actively absorbed by the tissues of the parathyroid glands.
After the substance is distributed throughout the tissues, the specified area is scanned using a special detector on a gamma camera. Using the resulting image, one can draw conclusions about the structural structure of the glands, their functional state, the presence of individual nodal changes, disruption of the organ and cell viability.
The scanning procedure itself takes no more than 20 minutes, but the examination process itself lasts at least 2 hours.
The radioisotopes that were used during scintigraphy disintegrate in a short time, their ability to irradiate disappears, they leave the body quite quickly and unhindered, so it can be argued that the radiation exposure to a person is very insignificant.
Scintigraphy is carried out as follows:
- The patient is injected intravenously with a radioactive isotope in the manipulation room.
The research process takes place in several stages:
- the first 10 minutes from the minute of intravenous administration of the substance;
- 2 hours after administration of the substance;
- 3 hours after administration of the substance.
- The duration of the study, its beginning and end, as well as the number of projections are strictly regulated by the doctor.
- During the examination, the patient must lie still on his back with his head slightly tilted back.
- After the drug is introduced into the body, and the first stage of the study is over, in agreement with the attending physician, the patient can remain in the medical institution, or may leave it for a while until the start of the next stage of the study.
- The patient can receive all scintigraphy results in his hands 30-60 minutes after the final stage of the study.
Benefits of scintigraphy
- The high sensitivity of the method allows us to examine pathological changes in the organ in the early stages of their development, which makes it possible to quickly make a diagnosis and begin adequate therapy appropriate to the stage of the disease.
- Radiopharmaceuticals used during scintigraphy do not have side effects.
- Possible complications of parathyroid scintigraphy may be the development of individual intolerance or an allergic reaction to a radiopharmaceutical.
Even though this diagnostic procedure is harmless to humans, it has its own limitations and contraindications. So, it is undesirable to perform scintigraphy in the following cases:
- Very obese patients
- A woman is pregnant or breastfeeding.
- The patient is too weak to perform the procedure.
Nowadays, scintigraphy is a very common diagnostic method for people suffering from diseases of the endocrine system.
The method is not at all dangerous for the patient, since the radiopharmacological substance is introduced into the body in a specially calculated dosage in advance.
The radiation emitted by radio tags is not capable of causing any damaging effects on nearby healthy tissues of the body.
The radiation dose will be comparable to an x-ray examination.
Typically, this study is prescribed as an additional test after ultrasound diagnostics and fine-needle biopsy.
Over the past twenty years, the scintigraphy method aimed at studying altered parathyroid glands has become more advanced.
Its disadvantages include the cost of the procedure - scintigraphy is several times more expensive than an ultrasound examination.
Scintigraphy of the parathyroid glands can be repeated no earlier than two months after the previous one, and no more than several times a year.
Stages of scintigraphy
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
A radiotracer is injected into the patient’s body, and it enters the organs through the bloodstream. When the substance has completely spread throughout the organs, pictures will be taken, which are recorded and processed by a computer. Images can be: dynamic, static, synchronized and tomographic. Using the images, the specialist studies the anatomical location, parameters, shape and other features of the area under study.
The dosage of the drug directly depends on the internal organ or system being examined. For a detailed and informative diagnosis of the heart, skeleton and brain, a large dosage of radiopharmaceuticals is required. Even a large amount of radioactive substance does not have a negative effect on the patient’s health, because the radiopharmaceuticals continuously disintegrate and are quickly eliminated from the body.
The duration of the procedure can vary from 15-20 minutes to 2.5-3 hours. The skeletal examination takes the most time – 2.5-3 hours. You can examine the heart within 50-60 minutes. It will take at least half an hour to diagnose the kidneys, liver and biliary tract. The thyroid gland can be examined in 20-40 minutes. The duration of the manipulation depends on how quickly the radiopharmaceuticals accumulate in the organ or system being examined.
The main advantage of the technique is its information content and low radiation dose. During the procedure, the patient receives less radiation than with radiography. Allergies to medications occur very rarely. To make sure that the patient does not have an allergic reaction to the radiopharmaceutical, an allergy test is done.
Decoding the results takes from 15 to 30 minutes. The specialist describes the condition of the organs, the pathologies found and writes his conclusion. Next, the patient is sent to the attending physician, who will make an accurate diagnosis and prescribe a course of treatment.
Methods
During bone scintigraphy, a small amount of a radioactive substance called a radiotracer is injected intravenously into the patient. Over time, the indicator accumulates in bone tissue. Depending on the state of the latter, the rate and intensity of accumulation differs. It is due to these parameters that the difference between normal and pathological is determined.
Bone scintigraphy is performed in three main ways. The simplest one is called planar scintigraphy. It displays the distribution of radioactive material in a single two-dimensional image, like that produced by a standard X-ray. This scanning method is most often used to detect primary tumors and metastatic bone lesions.
The second type of scan, single-photon emission computed tomography (SPECT), produces a series of contiguous two-dimensional images of the distribution of the radioactive tracer.
The third method, SPECT-CT, involves combining images obtained from different types of scans. This approach combines information about the function of the area of interest obtained from nuclear diagnostics with information about what the area looks like and where it is located from CT.
Contraindications and adverse reactions
Scintigraphy is contraindicated in patients with allergies to radioactive substances and pregnant women. If a woman is feeding her baby with breast milk, it is necessary to stop feeding for at least 24 hours to allow the medication to leave the body.
Side effects after the procedure include: allergies, increased or decreased blood pressure, frequent urination. At the first occurrence of symptoms, you should inform your doctor and undergo a course of symptomatic treatment.
More fresh and relevant information about health on our Telegram channel. Subscribe: https://t.me/foodandhealthru
We will be grateful if you use the buttons:
Contraindications
Due to the good tolerance of the examination, it can be performed quite often. To monitor cancer treatment, the procedure is done several times a year. Despite the relative safety of the study, there are a number of limitations for its conduct:
- Pregnancy is an absolute contraindication to scintigraphy due to the risk of harmful effects on the fetus. If there is a danger to the life of the pregnant woman, the examination can be done at a later stage.
- The lactation period is a relative contraindication. Since radionuclides are excreted in breast milk, a woman is advised to stop breastfeeding for a day and express milk.
- The procedure should be performed with caution in patients with a history of anaphylactic shock and angioedema.
- The limitation is early childhood. However, if the benefit outweighs the harm, then the child can be examined.
- Terminal stage of cardiac, renal, liver failure - due to the risk of fatal complications.