Features of the procedure
Ultrasound usually begins with an assessment of the fetal head, and the following parameters are determined:
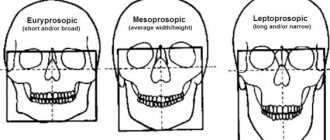
- Biparietal size of the fetal head (BPR)
is the distance from the outer surface of the upper contour to the inner surface of the lower contour between the parietal bones (Figure 1, line bd). - Fronto-occipital size (FOR)
is the distance between the outer contours of the frontal and occipital bones (Figure 1, line ac).
Figure 1 – Scheme for measuring biparietal and fronto-occipital dimensions:
1 – cavity of the transparent septum, 2 – visual thalamus and cerebral peduncles,
bd – biparietal size, ac – fronto-occipital size
Measurement of BPR and LZR is carried out with strictly transverse scanning
at the level of brain structures: the cavity of the transparent septum, the cerebral peduncles and the visual thalamus, as shown on the right side of Figure 1. When measuring, the doctor evaluates the structures of the brain, the integrity of the bones of the skull, and the presence of tumors.
The biparietal and fronto-occipital dimensions increase in proportion to the duration of pregnancy, by the end of which the growth is not as pronounced as in the first and second trimesters (see table).
Dimensions of the fetal head by week of pregnancy
| Gestation period, weeks | Fronto-occipital size (LZR), mm | Biparietal size (BPR), mm | ||||
| Percentiles | Percentiles | |||||
| 10 | 50 | 95 | 10 | 50 | 95 | |
| — | — | — | 13 | 17 | 21 | |
| — | — | — | 18 | 21 | 24 | |
| — | — | — | 20 | 24 | 28 | |
| — | — | — | 23 | 27 | 31 | |
| — | — | — | 27 | 31 | 35 | |
| 41 | 45 | 49 | 31 | 34 | 37 | |
| 46 | 50 | 54 | 34 | 38 | 42 | |
| 49 | 54 | 59 | 37 | 42 | 47 | |
| 53 | 58 | 63 | 41 | 45 | 49 | |
| 56 | 62 | 68 | 43 | 48 | 53 | |
| 60 | 66 | 72 | 46 | 51 | 56 | |
| 64 | 70 | 76 | 48 | 54 | 60 | |
| 67 | 74 | 81 | 52 | 58 | 64 | |
| 71 | 78 | 85 | 55 | 61 | 67 | |
| 73 | 81 | 89 | 58 | 64 | 70 | |
| 77 | 85 | 93 | 61 | 67 | 73 | |
| 80 | 88 | 96 | 64 | 70 | 76 | |
| 83 | 91 | 99 | 67 | 73 | 79 | |
| 86 | 94 | 102 | 70 | 76 | 82 | |
| 89 | 97 | 105 | 71 | 78 | 85 | |
| 93 | 101 | 109 | 73 | 80 | 87 | |
| 95 | 104 | 113 | 75 | 82 | 89 | |
| 98 | 107 | 116 | 77 | 84 | 91 | |
| 101 | 110 | 119 | 79 | 86 | 93 | |
| 103 | 112 | 121 | 81 | 88 | 95 | |
| 104 | 114 | 124 | 83 | 90 | 97 | |
| 106 | 116 | 126 | 85 | 92 | 98 | |
| 108 | 118 | 128 | 86 | 94 | 100 | |
| 109 | 119 | 129 | 88 | 95 | 102 | |
| 110 | 120 | 130 | 89 | 96 | 103 | |
Additional fetometric parameters
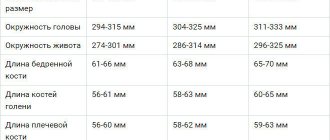
By the end of the 12-13th week of pregnancy, it is possible to determine parameters such as head and abdominal circumference, biparietal size, and femur length. These parameters are not mandatory for the first screening ultrasound, however, deciphering the results with these indicators will provide a more accurate picture of fetal development.
| Gestation period (weeks) | 12 | 13 | |
| Biparietal size (mm), percentile | 5th | 18 | 20 |
| 50th | 21 | 24 | |
| 95th | 24 | 28 | |
| Head circumference (mm), percentile | 5th | 58 | 72 |
| 50th | 72 | 84 | |
| 95th | 84 | 86 | |
| Abdominal circumference (mm), percentile | 5th | 50 | 58 |
| 50th | 61 | 69 | |
| 95th | 72 | 80 | |
| Average abdominal diameter (mm), percentile | 5th | 15 | 19 |
| 50th | 19 | 23 | |
| 95th | 23 | 27 | |
| Femur (mm), percentile | 5th | 4,0 | 7,0 |
| 50th | 7,3 | 9,4 | |
| 95th | 10,6 | 11,8 | |
| Exhaust/coolant ratio | 1,22 (1,10-1,30) | 1,21 (1,12-1,31) |
Measuring biparietal fetal size
Biparietal size of the fetal head
Produced from the outer edge of the parietal bone on one side to the inner edge of the parietal bone on the opposite side. A symmetrical increase in all parameters, including biparietal size, is a sign of the formation of a large fetus. If only this parameter is increased, then the development of hydrocephalus and brain tumors is possible.
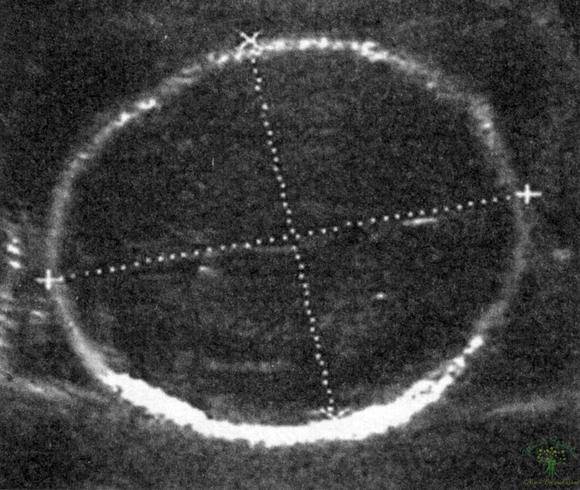
Fetal head circumference
Represents the circumference of the head. Measured along the outer contour. Based on this parameter, together with the biparietal size, the development of the brain and bone structures of the skull is assessed.
Abdominal circumference
Measured similarly to head circumference. Measurements are taken during a transverse scan while visualizing a section of the umbilical vein.
The average abdominal diameter is calculated as the arithmetic mean of the sum of the transverse and longitudinal diameters of the abdomen. These indicators are used to diagnose intrauterine growth retardation and its type (symmetrical or asymmetrical). During the first and second trimester, ultrasound often reveals a symmetrical developmental delay, in which all fetometric parameters are reduced.
Measuring the length of the femur
It is carried out on two limbs. In addition to measuring linear size, it is necessary to evaluate tissue structure, echogenicity, bone shape, as well as symmetry of development. Such a thorough study of bone structures makes it possible not to miss skeletal dysplasias, including reduced unilateral lesions, during ultrasound. During the second screening study, other bone structures (humerus, shin bones, fingers of the upper and lower extremities) are also measured. But at 10-14 weeks their visualization is problematic, so they are not included in the first screening ultrasound protocol.
The doctor conducting the study should not limit himself to measuring fetometric parameters. It is necessary to decipher the obtained ultrasound data, based on a comprehensive assessment of fetometric data, tissue echogenicity, as well as the state of blood supply and uterine structures. This will allow us to identify risk groups among pregnant women, set the date for the next ultrasound examination, and also predict the course of pregnancy.
The established normative values of fetometric indicators are very arbitrary and vary in different countries.
These indicators depend not only on the duration of pregnancy, but also on the physical characteristics of the future parents, and what kind of pregnancy it is. With the development of a multiple pregnancy, there is also often a discrepancy between parameters and established standards, even with its physiological course. Date: January 8, 2021
Biparietal size of the fetal head
To monitor intrauterine development during pregnancy, 3 ultrasound examinations are performed. During the ultrasound, fetometry is performed - measurements of the child’s body parameters.
Biparietal, or large transverse, size (LTS) is one of the indices by which the gestational age is determined. Among them, using the BPR, the deadline can be most accurately determined. This indicator is most informative from 3 to 7 months. BDP is measured using ultrasound examination.
The BDP is represented by the distance from one parietal bone to the other (between the temples). We can say that the BPR is the width of the child’s head.
As pregnancy progresses, the head of the unborn child grows, and, accordingly, the BPD increases. Specialists in the field of obstetrics have developed BPR standards. At the end of pregnancy, the rate of increase in this indicator decreases slightly.
Determining the gestational age using BDP is informative only up to the 22nd week; within this period, the accuracy of the determination reaches 5–10 days. But starting from the 28th week, the reliability of this method in terms of determining the period is questionable.
Moreover, after 38 weeks, the shape of the baby’s head changes, and the compliance of the BPR with established standards will depend on its configuration. For example, if the child's head has an elongated (dolichocephalic) configuration, then the BPD will be reduced compared to the norm.
BPD is considered one of the main indicators of child development, since the enlargement of the skull can be used to judge the enlargement of the brain, and, consequently, the development of the fetal nervous system.
In addition, BDP in combination with abdominal circumference and thigh length makes it possible to determine possible body weight. This indicator is very important before childbirth, since taking it into account, among others, determines the method of labor and obstetric care.
Baby's weight
This measurement is of great importance for the developing and growing embryo.
With its help, the obstetrician-gynecologist monitors the child’s condition and assesses the likelihood of abnormalities. With timely detection of abnormalities, the development of many intrauterine diseases can be prevented. The increase should be up to 100 g weekly, and several kilograms between screenings. It must be remembered that the individual characteristics of the child’s body can shift the size of the increase up or down from the table values.
Fronto-occipital size
The fronto-occipital dimension (FOR) is represented by a segment connecting the frontal and occipital bones. This is a line that is perpendicular to the BPR.
LZR is measured by scanning brain structures in a transverse direction. In addition to measurements of the BPR and LZR, the specialist notes the structure of the brain, skull bones (their integrity), and the presence of neoplasms.
Having measured the parameters, a cephalic index is derived, equal to the quotient of dividing these indicators, expressed as a percentage. This index gives an idea of the shape of the baby's head.
Both BPR and LZR increase proportionately during intrauterine development, then closer to childbirth their growth slows down.
What to do if the BPR and LZR are not normal?
If the BPD and LZR differ slightly from normal indicators, then this is most likely a developmental feature of a particular child.
When the size of the head exceeds the norm, it is necessary to evaluate other parameters (abdominal circumference, length of limb bones). If a large fetus
(over 4 kg), then all sizes will be increased by 1 or more weeks. In addition, children do not always grow proportionally, so the head may be larger relative to other sizes, but after 2-3 weeks it will level out.
An increase in BPR and LZR may also indicate the presence of pathology: space-occupying formations of the brain or skull bones (tumors), the presence of cerebral hernias, hydrocephalus
(excessive accumulation of cerebrospinal fluid in the ventricular system of the brain). In case of large formations or hernias, termination of pregnancy is suggested, since such deviations are often incompatible with life.
Hydrocephalus, as a rule, is a consequence of intrauterine infection, so a course of antibiotic therapy is carried out, and if there is no effect of treatment and the head grows in size, pregnancy is terminated. If hydrocephalus does not increase, pregnancy can be prolonged under ultrasound control over time. After birth, the child may need bypass surgery (implantation of a special tube into the brain with the other end in the abdominal cavity to drain excess fluid), which significantly complicates future life.
A decrease in the size of the fetal head may indicate underdevelopment or absence of anatomical structures of the brain (cerebral hemispheres, cerebellum). This is an indication for termination of pregnancy at any stage. It is necessary to look at the proportionality of the sizes of the head and other parts.
With reduced BPD and LZR, especially in the third trimester, intrauterine growth retardation syndrome
, which requires immediate correction, as it can lead to fetal death. The correction is carried out with drugs that improve uteroplacental blood flow, increasing the delivery of nutrients to the fetus (Actovegin, pentoxifylline, chimes), under mandatory ultrasound control after 7-10 days.
Additionally Summarizing the above, we can conclude that BPD and LZR are important parameters for assessing fetal development, establishing the anatomy of brain structures and excluding the diagnosis of FGR.
Reducing BPR and LZR
If the BPR and LZR indices are below normal, then the following may be observed:
- underdevelopment of parts of the fetal brain;
- absence of some parts of the brain;
- when the head is proportional to the entire body in comparison with normal values, intrauterine growth retardation syndrome is diagnosed.
In the first two cases, termination of pregnancy is necessary, regardless of the period. In the latter case, timely correction is required, since without it intrauterine fetal death is possible. For treatment, medications are prescribed that activate uteroplacental circulation, which improves fetal trophism (chimes, actovegin, pentoxifylline). After 7–10 days from the start of treatment, ultrasound diagnostics are performed again.
The diagnosis of developmental delay is made based on ultrasound results. Intrauterine growth retardation is considered to be a deviation of the established fetal weight from the standards presented in the tables of the ratio of fetal weight and its age by gestational age. Pathology is considered to be weight less than the 10th percentile of the tables.
There are cases when even with such a diagnosis there is no need to worry, since the child is simply small in size (the child’s parents, for example, may be short and light in weight). Then low weight is considered a peculiarity of the baby, which does not indicate reduced activity or mental and physical development. In this case, no special treatment is carried out either during pregnancy or after childbirth.
If this is not the case, then such a delay can lead to developmental deviations and even intrauterine death. With IUGR, it can be assumed that the nutrition of the fetus is impaired, so it does not receive the necessary nutrients and oxygen. Violation of fetal trophism is caused by:
- chromosomal abnormalities;
- smoking, alcohol or drug addiction of the mother;
- maternal hypertension, anemia or cardiovascular disease;
- improper attachment of the placenta;
- multiple births;
- taking certain medications without the advice of a specialist;
- long pregnancy (more than 42 weeks);
- maternal malnutrition;
- toxoplasmosis, rubella, syphilis and some other infections.
Increase in BPR and LZR
If during ultrasound diagnostics the dimensions of the head are determined to be larger than normal values, this is interpreted as follows:
- a proportional increase in all parts of the fetal body indicates that it is a large fetus (all parameters of its body are increased by 1 or more weeks). A fruit is considered large if its weight exceeds 4 kg;
- the head can grow faster than the rest of the body, so the situation is considered normal when within 14 to 21 days the parameters of the fetus become proportional;
- an increase in size may indicate pathologies: tumors of the brain or skull bones, brain hernias, hydrocephalus (accumulation of cerebrospinal fluid in the ventricles of the brain).
If tumors or hernias are diagnosed, termination of pregnancy is necessary; such disorders usually lead to fetal death. If hydrocephalus is diagnosed, an intrauterine infection is usually suspected. Therefore, antibiotics are prescribed for hydrocephalus. If hydrocephalus progresses, the pregnancy should be terminated. If progression of hydrocephalus is not observed, further pregnancy is carried out under the control of ultrasound diagnostics. After childbirth, shunting is possible to drain excess cerebrospinal fluid.
If deviations of the BDP and LZR from the norm are small, then they are considered developmental variations.
Determining the parameters of the fetal head is very important, since most often during childbirth it is the first to pass through the birth canal. Since the baby's head is dense and large in comparison with the rest of his body, it is with it that the main difficulties of the baby passing through the birth canal are associated. After the head has passed, the birth canal is ready for the passage of other parts of the baby's body.
Therefore, studying the size and shape of the child’s head is extremely important from the point of view of preparation for childbirth and prognosis of its course.
Categories
Planning
- Conception
- Infertility
- Preparing for pregnancy
- Late pregnancy
Pregnancy
- Examinations and procedures
- Fitness for pregnant women
- Personal care
- Lifestyle during pregnancy
- Nutrition and pregnancy
Childbirth
- Preparing for childbirth
- Recovery after childbirth
- Life after childbirth
Care and education
- Newborn care
- From 1 year to 3 years
- From 3 to 6 years
- From 6 to 11 years
- Education in other countries
Feeding
- Breast-feeding
- Artificial feeding
- Lure
- Baby food
Diseases
- Diseases during pregnancy
- Children's health
When copying materials, a link to the “Encyclopedia of Motherhood” is MANDATORY!
- About the site
- Rules
- Feedback
- Catalog of houses
- Children's website directory