What is perinatal screening
The content of the article
Perinatal screening is a set of diagnostic measures that allow prenatal examination of the fetus and identify expectant mothers with an increased risk of congenital pathologies and child development disorders. This screening in many countries is recognized as a basic test that provides the most complete information to the specialist managing the pregnancy and future parents regarding the health of the baby.
Many women, speaking about this examination, often confuse two concepts - prenatal and perinatal. So, prenatal diagnosis is carried out before conception, i.e. in this case, the expectant mother is examined. Doctors use different methods to determine the risks of having a sick child. Perinatal screening is an examination during pregnancy and the object of study in this case is the fetus. The importance of such a study, especially in the early stages, is undeniable: if the screening shows disappointing results, the patient always has a choice - to continue the pregnancy or terminate it.
What is pregnancy screening? When is screening done?

Abbreviations:
CA - chromosomal abnormalities
PDP - fetal malformations
Screening (from the English screening - “selection, sorting”) is a set of necessary activities and medical studies, tests and other procedures aimed at the preliminary identification of individuals among whom the likelihood of having a certain disease is higher than the rest of the population being examined.
Currently, it is considered advisable to carry out screening in the 1st and 2nd trimester of pregnancy, while the third screening in the Russian Federation, as a mandatory stage of prenatal examination, has been canceled since 2021.
The purpose of screening during pregnancy is to identify abnormalities or diseases in the fetus, such as malformations or markers of chromosomal abnormalities (CA), as early as possible.
Screening for chromosomal abnormalities:
- Every woman has the risk of giving birth to a child with a chromosomal pathology
- Baseline or initial risk is determined by the age of the pregnant woman and the length of pregnancy
- Individual risk is calculated by multiplying the baseline risk by the likelihood ratios of the screening tests
- The likelihood ratio for a specific ultrasound or biochemical marker is equal to the ratio of the percentage frequency of occurrence of this marker in fetuses with chromosomal pathology to that with a normal fetal karyotype
- Each time a new screening test is performed, the baseline risk for a particular patient is multiplied by the likelihood ratio of that test, resulting in an individual risk of fetal chromosomal abnormality.
- If the test results are not independent, then more sophisticated statistical methods must be used to calculate the combined likelihood ratio
During pregnancy, there are two types of screening:
1. Ultrasound screening - examination of the fetus using the ultrasound method for malformations and markers of chromosomal abnormalities (CA).
2. Biochemical screening (study of the amount of PAPP-A hormones in maternal blood serum, St. beta - hCG).
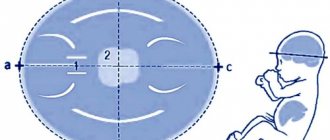
Rice. 1. Pregnancy 12 weeks 0 days. Fetal profile. Norm.
Rice. 2. Pregnancy 13 weeks 2 days. Fetal profile. Norm.
Screening during pregnancy is an essential part of prenatal care. Among the various screening tests currently carried out for pregnant women, ultrasound has the widest diagnostic capabilities. There is no other technique that can detect as many fetal anomalies and pregnancy pathologies as ultrasound. Another important advantage is the low cost of the study. In addition to the early detection of a normal singleton pregnancy, ultrasound can also detect multiple pregnancies and pregnancy complications at an early stage, for example, non-developing pregnancy, incomplete abortion, hydatidiform mole, ectopic pregnancy, etc. An ultrasound examination at the end of the first trimester can identify major abnormalities of the embryo or detect signs that allow one to suspect fetal malformations. In the II and III trimesters, primary attention is paid to the detection of fetal malformations and disturbances in fetal growth and development, as well as the diagnosis of pathology of the placenta, umbilical cord and amniotic fluid.
In addition to accurately determining the duration of pregnancy, the detection of intrauterine pathology depends on the research conditions, the equipment used and, especially, on the experience and professionalism of the doctor.
Frequency. Data on the incidence of major congenital malformations vary considerably depending on the type of detection system used. With passive detection systems, major malformations are detected in approximately 2-3% of newborns (E. Merz, 2011). When using active detection systems, in which the newborn is systematically examined by specially trained doctors, using a special standard, unified protocol, malformations are detected much more often (7.3% of newborns). This means that out of approximately 800,000 babies, 50,000-60,000 are newborns with major fetal malformations. In the United States, 100,000 to 150,000 newborns each year have severe malformations.
The high frequency (4-6%) and random nature of the occurrence of the vast majority of congenital malformations in children determine the search, development and improvement of ways of effective prevention as a priority in the system of maternal and child health care in countries around the world.
Over the past 15-20 years in Russia, prenatal diagnosis (PD) of the fetal condition has occupied an important place in the system of obstetric care for pregnant women, as a method of secondary prevention of congenital developmental disorders. Early prenatal diagnosis makes it possible to prevent the birth of a child with an incurable disease, and in the case of a number of correctable developmental defects, to provide effective care to the newborn, subject to planned hospitalization of the expectant mother for childbirth in a specialized institution.
In 2000, Order No. 457 of the Ministry of Health of Russia approved the procedure for prenatal examination of pregnant women, methods of prenatal diagnosis, algorithms for the interaction of doctors of various specialties: medical geneticists, obstetricians-gynecologists, neonatologists in determining the prenatal diagnosis and prenatal/postnatal tactics depending on the results of prenatal diagnosis. However, the effectiveness of prenatal diagnosis of congenital and hereditary diseases (CHDs) remains low, the frequency of births of children with severe forms of congenital malformations (CHDs) does not decrease, the rates of perinatal morbidity and mortality due to CHDs remain high, while the number of ultrasound examinations in obstetrics is quite large .
In this regard, on January 1, 2021, a new Order of the Ministry of Health of the Russian Federation dated October 20, 2020 No. 1130n came into force and is valid until January 1, 2027.
According to this order, at 11-14 and 19-21 weeks of pregnancy, pregnant women are assessed for antenatal development of the fetus in order to identify disorders: fetal growth restriction, risk of preterm birth, risk of preeclampsia, chromosomal abnormalities (CA) and fetal malformations (FDM) .
Ultrasound at 11-13 weeks can reveal a wide range of major fetal malformations:
- Major heart defects
- Congenital diaphragmatic hernia
- Omphalocele
- Megacystis
- Body stem abnormality
- Skeletal abnormalities
- With other defects, TVP is usually normal:
- Acrania/anencephaly
- Ventriculomegaly
- Holoprosencephaly
- Meningo-myelocephaly
- Gastroschisis
Anomalies of the heart and great vessels are the most common congenital malformations with a birth prevalence of 8 per 1,000. In general, more than half are asymptomatic and the other half are classified as major because they are either fatal or require surgery or invasive cardiac catheterization; major heart defects are responsible for 20% of stillbirths and 30% of neonatal deaths.
Twins account for approximately 1% of all pregnancies. Of these, 2/3 are twin (dizygotic), and 1/3 are identical (monozygotic)
- The incidence of dizygotic twins is higher in black (vs. white) women and also increases with maternal age and method of conception (20% with ovulation induction)
- The frequency of monozygosity is the same in all ethnic groups and does not change with maternal age, but can be 2-3 times higher after IVF
The incidence of twins has increased over the past 20 years. This increase is more pronounced in dizygotic twins. 2/3 of the increase in frequency is associated with the use of artificial reproductive technologies, and 1/3 with the age of the mother. With dizygotic twins, each fetus has its own placenta and amniotic sac. Monozygotic twins may share a placenta (monochorionic twins), a common amniotic sac (monoamniotic twins), or even share organs (conjoined or conjoined twins). A third of monozygotic twins are dichorionic (DC), and 2/3 are monochorionic (MC). Therefore, all MH twins are monozygotic, and 6 out of 7 DH twins are dizygotic.
The period of the first screening examination is the 1st trimester of pregnancy, namely the period of intrauterine development strictly from 11 to 14 weeks. At this stage, the pregnant woman is sent to the interdistrict (intermunicipal) office of antenatal fetal care at the obstetric medical organization of the second or third group (level) for an ultrasound examination (ultrasound) by medical specialists who have undergone advanced training in conducting screening ultrasound of pregnant women in the first trimester ( diagnosis of fetal developmental disorders), and collection of maternal venous blood samples to determine serum markers (pregnancy-associated plasma protein A (PAPP-A) and free beta subunit of human chorionic gonadotropin (hCG).
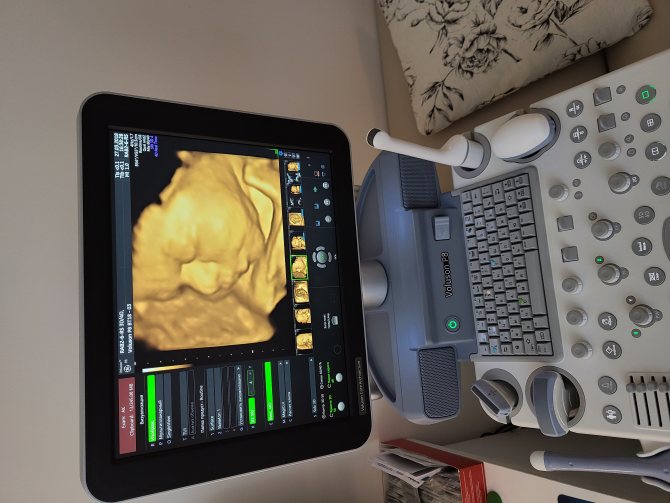
Rice. 4. Three-dimensional (3D) reconstruction of the fetus at 11 weeks.
In order to determine the risk of fetal growth restriction, premature birth and pre-eclampsia during a gestational age of 11-14 weeks, a pregnant woman in an inter-district antenatal fetal care office undergoes measurement of height, weight, blood pressure, Doppler ultrasound examination of the uterine arteries with determination of the pulsation index, transvaginal ultrasound cervicometry .
A blood sample with a referral coupon for the study of serum markers PAPP-A and St.-hCG in a woman at 11-14 weeks of pregnancy with ultrasound data to calculate the risks of chromosomal abnormalities, fetal growth restriction, preterm birth, preeclampsia, drawn up in the form according to Appendix N 8 to this Order, are delivered to an obstetric medical organization of the third group (level) or a medical genetic center (consultation) that has licenses in the fields of “obstetrics and gynecology (except for the use of assisted reproductive technologies and artificial termination of pregnancy)”, “ultrasound diagnostics” “and “clinical laboratory diagnostics”, where a biochemical blood test is performed to determine the level of maternal serum markers (pregnancy-associated plasma protein A (PAPP-A), free beta subunit of human chorionic gonadotropin (hCG). Based on the results of the analysis Maternal serum markers and referral coupon information are used through software to carry out a comprehensive calculation of the individual risk of having a child with CA, fetal growth restriction, as well as the risk of premature birth and preeclampsia.
The conclusion based on the results of individual risk calculation is sent to the medical organization where the first stage of the antenatal assessment of the fetal condition was carried out, in electronic form (via a secure communication channel on the Internet information and communication network) and is placed in the patient’s medical record (electronic record) or issued on patient's hands.
If a high risk (1/100 or higher) of fetal growth restriction, premature birth and preeclampsia is determined, further pregnancy management tactics are determined by the attending obstetrician-gynecologist at the antenatal clinic based on clinical recommendations. A pregnant woman should be consulted at a remote obstetric consultation center for further monitoring of the course of pregnancy in order to prevent the above complications.
If a pregnant woman is identified as having a high (1/100 or higher) risk for the presence of CA and/or PRP based on screening results at 11-14 weeks of pregnancy, she is sent to a third group (level) obstetric medical organization or a medical genetic center (consultation), having licenses in the profiles of “obstetrics and gynecology (except for the use of assisted reproductive technologies and artificial abortion)”, “ultrasound diagnostics” and “clinical laboratory diagnostics”, which carries out a comprehensive calculation of individual risk to clarify the diagnosis through repeated ultrasound with recalculation of the individual risk of having a child with CA based on repeated ultrasound data.
If a high risk of CA and/or PRP associated with CA is confirmed, the patient is recommended to undergo an invasive examination (chorionic villus aspiration/biopsy).
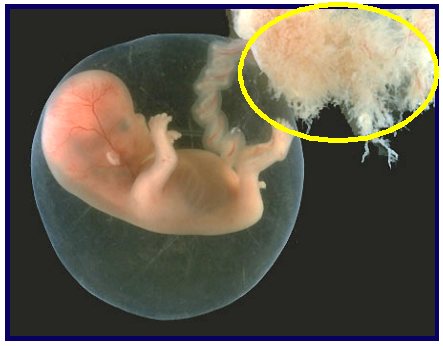
Rice. 5. Chorionic villi.
Chorionic villus aspiration/biopsy is carried out in a third group (level) obstetric medical organization or a medical genetic center (consultation) that has licenses in the fields of “obstetrics and gynecology (except for the use of assisted reproductive technologies and artificial abortion)”, “ultrasound diagnostics” " and "clinical laboratory diagnostics", on an outpatient basis, in a day or round-the-clock hospital setting. The resulting material is delivered to a genetic laboratory for genetic diagnosis and a conclusion from a geneticist.
The results of the genetic study (the conclusion of the geneticist) are sent to the office (department) of antenatal fetal care in electronic form (via a secure communication channel on the Internet) and are placed in the patient’s medical record (electronic record) or handed over to the patient .
If the diagnosis of CA and/or PRP is confirmed, recommendations for further pregnancy management tactics are provided by a council of doctors. The conclusion is drawn up in writing and sent to the attending physician electronically (via a secure communication channel on the Internet) and placed in the patient’s medical record (electronic record) or handed over to the patient.
Screening for preeclampsia
Preeclampsia (PE), which affects approximately 2% of pregnant women, is a leading cause of perinatal and maternal morbidity and mortality.
Compared with preeclampsia, which begins late in pregnancy, preeclampsia from early pregnancy requires delivery before 34 weeks and is associated with an increased risk of perinatal morbidity and mortality, as well as acute and chronic maternal complications. Identification of women at high risk for developing PE can potentially improve pregnancy outcomes, since intensive maternal and fetal monitoring in these patients will lead to early diagnosis of disease symptoms and fetal growth retardation associated with PE. Early diagnosis, treatment with antihypertensive drugs and early delivery can prevent the development of serious complications. Early identification of women at high risk for developing PE will also be important for future studies examining the potential role of pharmacological agents administered from the first trimester to improve placental circulation and reduce the incidence of this disease.
Second screening
According to Order No. 1130n, the second screening is carried out at 19-21 weeks of pregnancy.
At this stage, at a gestational age of 19-21 weeks, pregnant women with a low risk of CA and/or PRP, as well as those who have not undergone a screening examination at a gestational age of 11-14 weeks, are sent to the antenatal fetal care office at a medical organization with an obstetric profile of the second or third group ( level), high-risk pregnant women - to the office (department) of antenatal fetal care at a medical organization of obstetric profile of the third group (level) or a medical genetic center (consultation) licensed in the profiles of “obstetrics and gynecology (except for the use of assisted reproductive technologies and artificial termination of pregnancy)", "ultrasound diagnostics" and "clinical laboratory diagnostics", with the aim of conducting ultrasound and software risk recalculation to exclude ultrasound markers of CA that late manifest PRP.
Ultrasound results are documented in the form of a screening ultrasound protocol for women at 19-21 weeks of pregnancy in accordance with Appendix No. 9 to this Order.
If a high (1/100 or higher) risk of CA and/or PRP associated with CA is detected (confirmed), the patient is recommended to undergo an invasive examination (placentocentesis, amniocentesis, cordocentesis).
Based on the results of the examination, the attending physician provides the pregnant woman with information about the results of the examination, the presence of CA and/or PRP and the prognosis for the health and life of the newborn, treatment methods, associated risks, possible options for medical intervention (including intrauterine surgical correction), their consequences and results the treatment performed, on the basis of which the woman decides to carry or terminate the pregnancy.
Conclusion
Thus, screening in the 1st and 2nd trimester of pregnancy makes it possible to:
- Identify a prenatal diagnosis in the early stages of pregnancy and inform the woman about the existing developmental anomaly in her fetus, explain to the patient the severity of the congenital disease in her unborn child and the possible outcomes of pregnancy
- Change obstetric tactics if a woman and her family decide to refuse prolongation (preservation) of pregnancy in case of lethal (deadly) and non-correctable malformations and chromosomal abnormalities
- If a woman decides to continue the pregnancy, through a prenatal consultation, determine the timing and place of delivery to provide the necessary diagnostic and therapeutic measures to a newborn with a congenital malformation.

Literature:
1. Mertz E. Ultrasound diagnostics in obstetrics and gynecology: in 2 volumes. M.: MEDpress-inform, 2011
2. Zhuchenko L.A. and coll. authors. Prenatal (antenatal) diagnosis of child development disorders in institutions of the state and municipal healthcare systems of the Russian Federation. Modern concept and algorithms. 2010
3. Nicolaides K. Ultrasound examination at 11–13.6 weeks of pregnancy. / Translation from English by A. MIKHAILOV, E. NEKRASOVA - St. Petersburg: LLC Publishing House "Petropolis", 2007
4. Order of the Ministry of Health of Russia (Ministry of Health of the Russian Federation) dated October 20, 2021 No. 1130n “On approval of the Procedure for providing medical care in the field of obstetrics and gynecology”
Sincerely, ultrasound diagnostics doctor, Barto Ruslan Alexandrovich, 2021
All rights reserved®. Quoting only with the written permission of the author of the article.
Stages of perinatal screening
The entire complex of activities within the framework of perinatal research is divided into three stages, each of which the woman must go through at a certain stage of pregnancy. The first part of the diagnostic procedures occurs at 11-13 weeks of pregnancy, the second time you need to go for diagnostics upon reaching 18-24 weeks, the third perinatal screening is carried out at 30-34 weeks of pregnancy. The first 2 stages consist of two basic diagnostic procedures, each of which helps to identify genetic abnormalities
- Ultrasound – Ultrasound gives the most complete picture of the structure of organs, the functioning of the heart, as well as the external signs of the baby and its position in space.
- Biochemical blood test - this analysis is aimed at identifying in the patient’s blood certain substances of a protein nature that are produced by the fetus and amniotic membranes and may indicate the presence of chromosomal pathologies and disorders of the formation of the neural tube.
In our medical center, fetal examination is carried out using a modern 3D, 4D device with Doppler from SAMSUNG MEDISON
More about the service
Prenatal screening is a complex procedure aimed at identifying pathologies of fetal development in the 1st and 2nd trimesters of pregnancy.
Thanks to screening, a specialist can assess the health status of an unborn baby and determine the possible risk of developing genetic diseases. The procedure is not the final verdict on whether the baby will be born with an abnormality or disease. It provides information about the presence of the risk itself. After studying the results of prenatal screening, the geneticist may prescribe additional clarifying studies. Only after this are final conclusions made.
Stage I of perinatal screening (11-13 weeks)
Examination of the expectant mother during this period allows us to obtain a huge amount of information regarding the condition of the baby and the general course of pregnancy. Ultrasound examination at 11-13 weeks of pregnancy in modern clinics is carried out using three-dimensional echography - 3D ultrasound (3D), thereby obtaining the following data regarding pregnancy:
- The number of viable embryos implanted in the uterus.
- Determining the exact duration of pregnancy.
- The presence or absence of gross malformations.
- Nuchal translucency thickness TVP (used as an indicator of some chromosomal syndromes).
- Visualization of the nasal bone is important to exclude the possibility of Down syndrome.
After undergoing a classic ultrasound, a pregnant woman undergoes a biochemical blood test, which at this stage is called a “double test”, due to the fact that the quantitative levels of two protein components are measured: PAPPA and hCG (free β subunit).
hCG (human chorionic gonadotropin)
- one of the main pregnancy hormones contained in the mother’s blood serum. Its reduced level indicates placental pathologies, and its increased content may indicate chromosomal abnormalities in the fetus.
PAPP-A – also called protein A
. Its concentration in maternal blood may indicate the presence of chromosomal diseases such as Down and Edwards syndromes.
Stage II of perinatal screening (16-18 weeks)
At this stage, it is quite possible to conduct a 3D or 4D ultrasound, which makes it possible to evaluate all the external aspects of the baby, and also, in the case of four-dimensional echography, determine the mobility of the fetus and its gender.
The biochemical component of the second stage is a “triple” test, which involves identifying and measuring the following protein components in the blood of the expectant mother:
- Free β subunits of hCG.
- Alphafetoprotein.
- Free estradiol.
ACE (Alpha Fetoprotein)
- a specific protein that is produced directly by the fetus and enters the mother’s blood through the placenta. Its increased content may indicate defects of the fetal neural tube and defects of other vital organs. A decrease in ACE can be recorded in chromosomal diseases such as Down syndrome.
Free estradiol
is a female steroid hormone that must be produced by the placenta during pregnancy. A decrease in the level of estradiol in a woman’s blood may indicate a violation of fetal development.
Perinatal screening results
Despite the fact that perinatal genetic screening is recommended for all pregnant women, there are a number of families for whom a thorough diagnosis and consultation with a geneticist during pregnancy is mandatory:
- The spouses have relatives with severe genetic diseases.
- In a consanguineous marriage.
- During late pregnancy (mother is over 35 and father is over 40 years old);
- If the couple has already had children with genetic disorders.
- If the mother has severe somatic diseases (heart or kidney pathologies, diabetes mellitus);
- During difficult pregnancy;
- If you suspect the presence of genetic pathologies identified during ultrasound.
Evaluation of results
Data from ultrasound diagnostics and blood biochemistry are assessed together using special programs, which makes it possible to determine a woman’s individual risk. The risk group includes expectant mothers whose results are 1:300 – the risk of having a baby with a chromosomal abnormality. However, it should be understood that this result is not yet a diagnosis. To establish more accurate results, the pregnant woman is sent for additional studies in the form of invasive diagnostics. Now let's take a closer look at the most important part of perinatal screening during pregnancy - ultrasound.
Second screening
It is carried out even if there are no problems or complaints during pregnancy. At this stage, it is determined which risk groups the fetus falls into, whether there are complications, chromosomal abnormalities, or congenital pathologies. It is advisable to conduct the study starting from the 16th week, and when assessing the result, the data of the first diagnosis are taken into account.
Based on the information obtained during screening and data from the questionnaire filled out by the expectant mother, the doctor, using analytical computer programs, clarifies the timing of pregnancy and draws conclusions about the risks. If necessary, the pregnant woman is referred for additional consultation with a geneticist.
The second study can be ultrasound, laboratory (biochemistry) or combined, depending on the indications.
Ultrasound examination
It is mandatory for pregnant women at risk and is desirable for everyone, especially those working in “heavy” industries or taking medications that are not recommended during pregnancy. At this stage, the fetus is already noticeably larger, which makes it possible to study:
- the face of the fetus - how the eyes and ears develop, what size are the bones of the nasal part, are there any clefts in the oral cavity and other abnormalities;
- the distance from the baby to the uterine walls - by measuring it, the amniotic fluid index is determined (the value depends on the period);
- fetal weight - at 16 weeks it is approximately 100 g during normal development, and at 20 it is already 300 g;
- body size (the study is called fetometry) - at the time of the study it is usually 11-17 cm;
- the structure of organs, the degree of formation of the lungs, the number of fingers and toes;
- umbilical cord - the presence of two arteries and a vein, homogeneity of structure, place of attachment to the uterus;
- gender of the child - but the degree of accuracy may vary.
Also, during ultrasound screening, the condition, thickness, maturity of the placenta, and its location are assessed - it is considered normal to be attached to the back of the uterus, at the uterine fundus. The position along the anterior wall creates risks of stretching, detachment, and presentation.
The level of amniotic fluid is also checked. During normal pregnancy, their volume is sufficient to conduct a high-quality abdominal examination. After the doctor takes data using the sensor, he processes the results and compares the information with tables of standard values. The accuracy of diagnosis is determined by the characteristics of the ultrasound machine, the position of the fetus, etc.
Blood analysis
The results of an ultrasound examination are supported by a screening blood test if abnormalities are detected, but even if the indicators are at the normal level, it is advisable to carry it out. At this stage, three important new characteristics appear - the concentration of free estriol, b-hCG and AFP protein - which is why the test is called triple. Sometimes a quadruple is recommended, adding a study of the level of inhibin A.
When preparing for screening, it is worth eliminating seafood, citrus fruits, fatty and smoked foods from your diet for several days, and limiting fruits and sweets. Blood is donated on an empty stomach, the last meal is 10-12 hours before the test. If an analysis is not done at this stage of pregnancy to compare the data with previous studies, later analysis will be of little information. In this case, Doppler measurements and CT scans are performed to assess how the fetus, umbilical cord and placenta are supplied with blood.
What the results say
The second ultrasound screening, in combination with the data of the first, provides information about the presence/absence of gene pathologies, the danger of which is determined by MoM. The norm is 0.5-2.0, with a risk level of 1:380 and higher according to the second number. If it is below the value, there is a high risk of pathologies.
A screening blood test provides information about the likelihood of:
- the formation of Down, Klinefelter or Edwards syndromes - in the worst case scenario at this stage, as a rule, we are not talking about abortion, but about induced childbirth;
- neural tube defects, central nervous system;
- hypoxia and other deviations from the normal course of pregnancy.
The results may indirectly indicate an exacerbation in the course of pregnancy - changes in the structure of the placenta, etc. If the risks are high, the patient is referred for additional studies.
The role of 3D ultrasound in perinatal screening: 3D or 2D?
Today, no one doubts that ultrasound diagnostic techniques are the most important aspect of monitoring intrauterine development, age and position of the fetus. At the same time, the technical base of medicine does not stand still, and in addition to the classic, two-dimensional ultrasound, such a useful diagnostic practice as 3D ultrasound or three-dimensional echography has come. The advantages of this research method lie in the possibility of obtaining a three-dimensional image, which in all colors demonstrates to the specialist and future parents all aspects of the external manifestations and organs of the baby.

Differences between 3D ultrasound and classical ultrasound
All ultrasonic research methods have a common principle, which is based on the use of ultrasonic radiation, the wave frequency of which does not exceed 20 kHz. Applying such a wave load in a pulsed mode makes it possible to assess the functional normality and morphological structure of tissues, organs and systems of the fetus. At the same time, the traditional two-dimensional method displays a flat image on the dashboard monitor, which is understandable to doctors, but is not informative for non-professionals, namely for the child’s parents who are looking forward to meeting the baby for the first time. It should be noted that this method of diagnostic monitoring is important for medical specialists managing pregnancy, as it makes it possible to fully assess the structure of the internal organs of the fetus, which is incredibly important when organizing comprehensive monitoring.
Three-dimensional echography produces a full-fledged three-dimensional image that does not require decoding and clearly reflects the external features and position of the baby in the womb.
Advantages of 3D ultrasound in perinatal screening
3D ultrasound provides doctors with a number of obvious advantages:
- A clearer image
makes it possible to identify a number of defects that cannot be identified during classical ultrasound screening: hand anomalies, facial clefts, skeletal malformations, disturbances in the formation of the anterior abdominal wall, placenta anomalies, structural features of the external genitalia, non-fusion of the spinal cord, etc. . Identification of all of these abnormalities requires a change in the strategy for managing such a pregnancy. - 3D ultrasound allows you to determine the sex of the baby
more accurately in the early stages of pregnancy, which may be necessary not only to satisfy the curiosity of future parents, but also from the point of view of eliminating the likelihood of hereditary pathologies associated with gender. - The psychological readiness of the mother and father
for the birth of the long-awaited child, of course, increases after the initial acquaintance with the baby, even through a monitor and a photograph, which, at the request of the parents, can be provided after this manipulation.
Features of three-dimensional echography
According to the results of numerous medical studies, 3D ultrasound is an absolutely safe diagnostic method that is used for medical reasons. The features of 3D ultrasound during screenings during pregnancy include the following factors:
- Three-dimensional echography is most informative at 22-33 weeks of pregnancy, since during this period the external signs of the fetus are already sufficiently formed, and its size does not interfere with visual inspection.
- The duration of a three-dimensional ultrasound is about 40 minutes, which is much longer than the time required for classical two-dimensional screening.
- The bladder does not have to be full before performing a 3D ultrasound.
- The diagnostic capabilities of the technique drop significantly in the presence of such characteristics of the patient or the course of pregnancy as severe obesity of the expectant mother, oligohydramnios, the presence of scars on the woman’s abdominal wall, or uncomfortable position of the fetus.
Three-dimensional echography is a diagnostic practice that has earned the trust of doctors and patients around the world, confirming its exceptional effectiveness and safety for both women and babies. At the same time, today, 3D ultrasound remains the “gold standard” for intrauterine study of the structure of facial structures, limbs, sexual characteristics and space-occupying formations in the fetus, as well as a backup method for identifying such chromosomal abnormalities as Down syndrome, Patau syndrome, etc.
What types of screenings are there?
There are 5 types of screening during pregnancy:
- Ultrasonic;
- Biochemical;
- Immunological (testing a pregnant woman for a number of infections that potentially impair the development of the fetus. These include rubella, herpes, chicken pox, cytomegalovirus, toxoplasmosis, etc. Prescribed to everyone when registering for pregnancy);
- Cytogenetic (optional, performed according to indications);
- Molecular (detection of rare mutations occurring with a frequency of no more than 1%. Prescribed in unique cases)
Separately, invasive diagnostics are distinguished: chorionic villus biopsy (sampling a piece of tissue from the outer membrane around the embryo), amniocentesis (puncture to collect amniotic fluid), placentocentesis (biopsy of the placenta) and cordocentesis (sampling of the fetal umbilical cord blood). These are complex manipulations, they are necessary for cytogenetic research when searching for chromosomal diseases. It is carried out extremely rarely and only after a cascade of other examinations with disappointing results in order to confirm or exclude the diagnosis.
In addition to 5 types of screening, every 2-4 weeks pregnant women donate blood and urine for general clinical analysis.
Let's take a closer look at why each examination is needed.
The value of 4D ultrasound in perinatal diagnosis: advantages and features
In modern practice of medical management of pregnancy, such a procedure as 4D ultrasound has become basic, both for a specialist monitoring the course of gestation and for impatient parents who are waiting to meet their child. This technique has several significant advantages over classical two-dimensional screening and is very often used as an addition to the basic course of mandatory research.
4D ultrasound will provide an opportunity not only to fully assess the health and development of the baby, but will also give parents the joy of first visual contact with the child, who will be in the natural intrauterine environment.
4D ultrasound - capabilities and advantages
The capabilities of the 4D ultrasound procedure are somewhat expanded in comparison with the usual two-dimensional echography. This is ensured by the fact that the examination (also called color ultrasound) allows you to evaluate the external manifestations of the fetus using four dimensions simultaneously: depth, height, length and time. As a result of the procedure, the image displayed on the dashboard monitor will resemble a video that in real time demonstrates not only the appearance and main morphological features of the baby, but also his movements, facial expressions, gestures and smile.
If the baby has not turned his back to the ultrasound scanner, such a sight evokes a lot of positive emotions among parents and provides certain diagnostic information to the specialist.
Positive aspects of 4D ultrasound for a pregnancy specialist
In addition to data that is standard for all ultrasound methods regarding the age, size and position of the fetus, 4D ultrasound gives the specialist the opportunity to determine the presence of the following anomalies in the baby’s development:
- Facial defects (facial clefts)
- Skeletal malformations (non-fusion of the spinal cord)
- Anomalies of the hands (quantitative pathologies of the fingers)
- Presence of space-occupying formations in the fetus
- Pathological changes in the placenta
- Defects of the anterior abdominal wall
- Abnormal development of the external genitalia
4D ultrasound makes it possible to track the natural movements of the fetus. This can also become important information in the process of confirming a particular developmental pathology. Thanks to the expanded review that this option of ultrasound screening implies, it is also possible to visually assess the structure of all external signs. This is especially true for facial structures (nasolabial triangle, lips, ears, chin, nose, etc.).
It should also be noted that the 4D technique provides more accurate information regarding the baby’s gender. This information is of interest to the doctor due to the presence of a hereditary pathology factor or genetic abnormalities linked to sex. And this is one of the main tasks of perinatal screening.
Positive aspects of 4D ultrasound for expectant parents:
- The opportunity to see the baby long before his birth, establish a certain psychological contact with him, and also prepare for the external characteristics of the baby.
- You can find out exactly the gender and even see the confirmation in person, on the monitor screen. This aspect almost always worries parents, as well as the developmental characteristics of the child.
- Parents can receive a video that will remain an unusual memory of such an important period in the life of every family as pregnancy. We are giving a CD with the recording as a gift!
How does 4D ultrasound work?
The procedure is practically no different from standard ultrasound screening. However, four-dimensional echography takes almost three times longer than black-and-white ultrasound (about 45 minutes). At the same time, a pregnant woman should know that filling the bladder does not affect the results obtained. In addition, it is worth understanding that the 4D technique has a maximum level of information content in the period from 22 to 33 weeks, which is due to the development and size of the fetus.
Patients suffering from severe forms of obesity or having scars on the abdomen, as well as when diagnosing a condition such as oligohydramnios, should be prepared for the fact that the picture may not be clear enough. In almost all other cases, 4D ultrasound will be an excellent way to get to know the baby and get a guarantee of its normal intrauterine development. The Diana Clinic offers its patients a 4D ultrasound procedure, guaranteeing information content and safety for the baby and the expectant mother.
Last trimester screening - third trimester requires special attention
Ultrasound diagnostics is carried out at a period of 30–34 weeks and its main function is to assess the location of the placenta, its function, study the condition of the fetus, its internal organs, as well as the degree of readiness of the maternal organs for childbirth. The final screening will show which route of delivery is safest for the baby and woman, how soon the birth will occur and whether additional prenatal preparation is needed.
The following indicators are subject to assessment:
- fetal presentation: transverse or pelvic requires cesarean section;
- gestational age, which corresponds to the size of the fetus;
- the thickness of the placenta, its structure, localization, degree of maturity - deviation from the norm of one of the indicators can cause oxygen starvation of the developing fetus;
- condition of the umbilical cord: ultrasound allows you to determine the entanglement and choose the appropriate delivery tactics in a particular case;
- the length of the cervix, the degree of its opening: if there is an opening or a short length of the cervix, the woman is indicated for corrective therapy;
- purity and quantity of amniotic fluid;
- in case of multiple pregnancy, the difference in the size of the fetuses is assessed.
At the third ultrasound, detailed fetometry of the fetus is also performed: the length of the limbs, the volume of the abdomen, chest, head are determined, the heart rate and other indicators are determined. According to the data obtained, the gestational age is determined, which is usually 1 to 2 weeks different from the obstetric period. This is associated with spasmodic intrauterine development of the fetus and cannot be a reason to suspect IUGR.
At the third ultrasound, the baby’s weight is determined, from which its approximate birth weight can be determined. The sex of the fetus is determined with great certainty if it does not cross its legs during the study.
The correct structure of the internal organs of the fetus is subject to assessment: brain, lungs, heart, abdominal organs, etc., and its motor activity is also assessed. The third ultrasound can reveal:
- developmental anomalies that are compatible with life, but may require urgent correction - medicinal or surgical - immediately after birth;
- oxygen starvation of the fetus, which is well determined by its motor activity and muscle relaxation; During the ultrasound, the child must move at least 2 times;
- fetal presentation: if it is pelvic, an external rotation is made through the abdominal wall.
Analysis for hCG β - unit for perinatal diagnosis
HCG (human chorionic gonadotropin) is a hormone whose concentration increases sharply during pregnancy. Its increase indicates that conception has occurred, which is extremely important during pregnancy resulting from infertility treatment. HCG is not strictly a “female” hormone. This substance is specifically administered to men in order to improve sperm count in cases of suspected male infertility.
What is hCG and β – hCG
This substance consists of two components:
- α-unit similar to other hormones;
- β is a unit unique to hCG, distinguishing it from other hormonal substances.
That is why it is the β - unit that is analyzed, and the analysis itself is often called β - hCG.
The hormone is produced by the cells of the embryonic membrane to stimulate hormones that support pregnancy - progesterone and estrogen. This prevents the onset of menstruation and allows the embryo to “take root.” That is why, in case of infertility, doctors analyze the level of hCG in the patient’s body. If its content drops or lags behind the norm, the woman is prescribed hormonal drugs to support pregnancy. Monitoring the level of the hormone is necessary for women who are prone to recurrent miscarriage and have had frozen pregnancies.
The concentration of hCG increases rapidly until the placenta is formed, which later takes over the hormonal function. A rapid increase in hormone levels indicates that the pregnancy has continued and the embryo is developing. Subsequently, the hormone content decreases, remaining elevated before childbirth and somewhat after it.
Normal hCG levels vary greatly between women. The doctor determines whether everything is normal by the dynamics of changes in the indicator in a particular patient.
Approximate hormone concentrations during pregnancy are given in the table
| Duration, weeks | Concentration, honey/ml |
| 1 | 20-155 |
| 2 | 100-4850 |
| 3-4 | Up to 82,000 |
| 5-6 | Up to 151,000 |
| 7-8 | Up to 230,000 |
| 9-10 | Up to 290,000 |
| 11-16 | Decreases from 290,000 to 245,000 or less |
| 17-25 | Reduces to 50,000-80,000 |
| 25-37 | gradually decreases to 40,000 or less |
Inconsistency between the level of hCG and the period is observed in pathologies of pregnancy and abnormal development of the fetus
| promotion | demotion |
| hydatidiform mole | frozen pregnancy, embryo death |
| multiple pregnancy | risk of miscarriage |
| toxicosis | fetal underdevelopment |
| congenital hereditary diseases and fetal malformations | ectopic embryo implantation |
| hormonal pathologies in the mother | in the later stages indicates post-maturity |
Unlike pregnancy, in diseases that cause an increase in hCG levels (ovarian, stomach and breast cancer), the level of the hormone increases gradually and does not decrease. Therefore, a woman is prescribed such an analysis several times during pregnancy.
How is the β-hCG screening test performed?
For this study, blood from a vein or urine is donated, but the hormone is determined in urine later, and the result is not so accurate. Therefore, it is better to rely on a blood test showing the presence of the hormone and its concentration.
The material is collected in the morning on an empty stomach; if you need to take tests urgently, you need to fast for 4-6 hours. It is advisable not to take medications at this time. If the level of hCG in the early stages begins to rapidly decrease or increase, you need to consult a doctor and identify the cause.
Tests for chronic fatigue
If signs of rapid fatigue and tiredness appear, already in the morning, you feel like you haven’t rested, and there are no obvious reasons, that is, you don’t work 12-16 hours 7 days a week, you haven’t rested for more than 2 years, you are the mother of a newborn baby who sleeps poorly at night and you do not get enough sleep, you can assume conditions for which such a symptom is very typical and undergo an examination to clarify the correctness of the assumption.
- Anemia and iron deficiency: general clinical blood test, blood test for serum iron, ferritin, TBC, vitamin B12 and B6.
- Diseases of the thyroid gland (usually decreased function - hypothyroidism, at first it can manifest itself this way): a blood test for TSH (thyroid-stimulating hormone) - at first it is enough to screen for disorders of the thyroid gland.
- Reduced sodium and calcium levels: Blood test for electrolytes (potassium, sodium chloride), calcium.
- Viral hepatitis: blood test for hepatitis B (HBsAg - Australian antigen) and C (Anti-HCV-total - antibodies to the hepatitis C virus).
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
For a more detailed examination and exclusion of diseases of the kidneys, liver, lungs, you may additionally need: R-graphy of the lungs, ultrasound of the organs of the retroperitoneal space and abdominal cavity, as well as to exclude rheumatological diseases, an additional blood test for C-reactive protein (protein), ALT, AST, total and direct bilirubin, urea, creatinine, total protein and albumin.
Such examinations should not be carried out independently, but rather contact a competent therapist to prescribe a competent and complete diagnosis.
Sometimes, even a very detailed examination does not reveal changes and does not provide an explanation for such complaints. In this case, depression or chronic fatigue syndrome should be ruled out.
Where to do perinatal screening in St. Petersburg
The Diana Clinic in St. Petersburg offers all stages of perinatal screening, guaranteeing an individual approach to each woman and maximum reliability of the results obtained. Our specialists have extensive experience in the field of diagnostics during pregnancy. The medical center’s hardware makes it possible to carry out both basic and additional stages of screening.
<
p style=”text-align: justify;”>
CLICK TO SIGN UP
If you find an error, please select a piece of text and press Ctrl+Enter