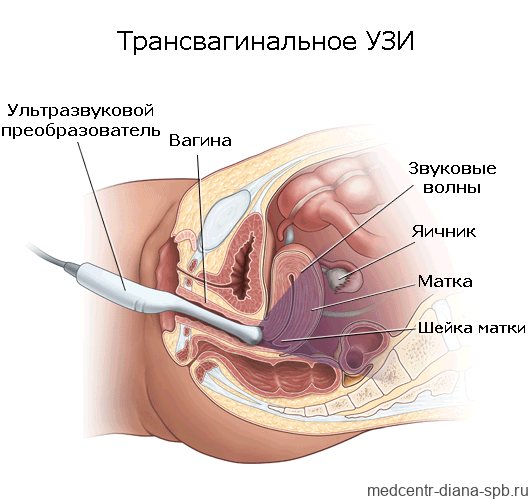
Transvaginal ultrasound (TVUS) is performed to diagnose the condition of the pelvic organs in women. The study is prescribed to identify urological and gynecological diseases, monitor their course and treatment results, as well as to determine the duration of pregnancy and exclude pathologies in the first trimester. TVUS today is the most accurate and informative method for examining the pelvic organs in women.
CLICK TO MAKE AN APPOINTMENT, TEST OR ULTRASOUND
COST OF TRANSVAGINAL ULTRASOUND 1000 RUB. CONSULTATION WITH A GYNECOLOGIST ON THE RESULTS OF AN ULTRASOUND OR ANALYSIS - 500 rubles
This type of examination has a minimum of contraindications, is absolutely painless and inexpensive.
Features of the diagnostic technique
The content of the article
Transvaginal examination differs from transabdominal examination only in that in the first case, ultrasound waves are supplied through a sensor that is located in close proximity to the organs being examined or the fertilized egg: they are separated only by a thin vaginal wall. With transabdominal ultrasound, the sensor is moved along the lower abdomen, but this technique does not provide a clear overview if the patient is obese or suffers from increased gas formation in the intestines.
The intracavitary sensor (transducer) looks like a rod 12 cm long, and its diameter does not exceed 3 cm, so its penetration during the study does not cause unpleasant sensations. The sensor has an oblique view relative to its axis, which is necessary for better visualization of the uterus, taking into account its anatomical location. At the end there is a channel with a needle, which may be needed in case of tissue biopsy.
Intravaginal ultrasound examination is absolutely safe, so it can be done multiple times. Sometimes TVUS is prescribed several times during one menstrual cycle.
WE DO ALL TYPES OF ULTRASOUNDS 2D, 3D, 4D with DOPPLER / We do all kinds of ultrasound - 2D, 3D, 4D diagnostics with Doppler
We use one of the best ultrasound scanners with Doppler SonoAce X8 from SAMSUNG MEDISON. This device combines a maximum range of functions and a wide range of diagnostic capabilities - it includes all types of sensitive Doppler, it has an excellent degree of visualization, the ability to panoramic scanning of organs and constructing images in real time in 2D, 3D and 4D formats. The kit contains all the sensors necessary for performing any type of ultrasound - transavaginal, transabdominal and transrectal. We use one of the best ultrasound scanners with the SonoAce X8 doppler from the company SAMSUNG MEDISON. The device for the diagnostic combines the maximum set of functions and a wide range of diagnostic capabilities. SonoAce represents all kinds of sensitive Doppler, has an excellent degree of visualization, the possibility of panoramic scanning and the construction of images in real time in 2D, 3D and 4D formats. The kit includes all necessary ultrasound sensors of any type – transvaginal, transabdominal and transrectal.
ATTENTION! IN THE CLINIC IS A DOCTOR SPEAKING IN ENGLISH LANGUAGE!
Modern ultrasound 3D, 4D with Doppler from Samsung Medison
How is a vaginal ultrasound performed?
A woman undresses, as if for an examination by a gynecologist. Then he lies down on his back, on a medical couch, spreads his legs and bends them at the knees. A sterile condom is put on the transducer, which is additionally lubricated with lubricant. The probe for research is approximately 12 cm long with a rod diameter of 3 cm. It usually has a slightly curved handle and an additional channel into which a needle is inserted to collect tissue for histology.
The transducer is inserted to a shallow depth into the vagina. This procedure is painless and if pain occurs, you should immediately inform your doctor. The sonologist turns the sensor at different angles. If it is necessary to collect tissue for analysis, a needle is inserted into the channel of the device, with the help of which the manipulation is carried out. The duration of the procedure is no more than 15 minutes. Transvaginal ultrasound does not cause complications.
Indications for TVUS
Transvaginal ultrasound examination is prescribed for suspected diseases of the pelvic organs, emergency conditions, and also to assess the results of treatment. Indications for this diagnostic technique are:
- Severe pain during menstruation.
- Lack of menstruation or irregularity.
- Suspicion of hormonal imbalance in the body.
- The appearance of bleeding outside the menstrual cycle.
- Presence of symptoms of inflammation of the uterus or ovaries.
- Pathological changes in the endometrium: hyperplasia, polyps, chronic endometritis, submucosal nodes.
- Diagnosis of endometriosis of the uterus or adjacent organs.
- Determination of the presence of pathological fluids in the fallopian tubes.
- Suspicions of underdevelopment of the pelvic organs.
- Identification of neoplasms suspected during a gynecological examination.
- Diagnosis of neoplasms and tumor processes of the uterus and bladder.
- Detection of ovarian tumors and cysts.
- Suspicion of ruptured ovarian cysts.
- Infectious diseases of the urinary tract.
- Suspicion of uterine fibroids.
- Diagnosis of the causes of urological diseases, urinary incontinence and other urinary disorders.
- Determining the location of the intrauterine device.
- Monitoring the effectiveness of treatment.
- Monitoring the condition of the endometrium with an intrauterine device installed or taking hormonal drugs.
- Inability to conceive for six months.
- Preparation for IVF and support of the procedure.
Transvaginal ultrasound allows a woman to know when she is ready to conceive a child. To do this, during a TVUS, a special substance is injected into the fallopian tubes, which, as a contrast, shows the patency of the tubes on the day of the study.
No other method, except TVUS, is capable of recording the baby’s heartbeat as early as the 5th obstetric week of pregnancy. Therefore, transvaginal ultrasound in early pregnancy can confirm the fact of successful conception.
Indications and contraindications
An ultrasound of the pelvic organs in the presence of problems in the sexual sphere or previous gynecological diseases is carried out annually as part of preventive purposes.
Additionally, a vaginal examination is prescribed for:
- bloody discharge in the absence of a menstrual cycle;
- absence of pregnancy for 6 months with active sexual activity;
- the presence of pain in the lower abdomen in the absence of menstruation;
- the need to establish an ectopic pregnancy;
- suspicion of the presence of neoplasms and various types of cysts in the pelvic organs;
- determining the anatomical structure of the uterus and measuring its length;
- pain during sexual intercourse;
- determining the shape and diagnosing the functioning of the ovaries.
Transvaginal ultrasound also helps to detect the presence of pathologies in obese individuals. With other types of diagnostics, the presence of fatty deposits does not make it possible to fully see the condition of the pelvic organs.
A vaginal ultrasound helps identify the following diseases and conditions:
- Endometriosis.
- Ovarian cyst and possible ruptures on it.
- Bubble drift.
- Chorionepithelioma.
- Excess fluid in the fallopian tubes, lower abdomen and pelvis.
- Myoma and/or malignant tumor of the uterus.
- Endometrial polyposis.
- Ovarian cancer.
Diagnostics also determines the presence of pregnancy, both uterine and ectopic.
There is only one contraindication for prohibiting the study - an allergy to latex.
For girls who have not been sexually active, a vaginal examination is performed not through the vagina, but through the rectum.
TVUS during pregnancy
Since the intravaginal examination procedure is associated with a certain irritation of the walls of the vagina and pelvic organs (including the uterus), it is allowed only in the first trimester - up to 13 weeks of pregnancy. TVUS makes it possible to detect the very fact of pregnancy and determine its exact date. But there are other indications for conducting such a study:
- monitoring the fetus and its development over time;
- determination of intrauterine and ectopic pregnancy;
- early diagnosis of fetal and pregnancy pathologies;
- identification of threats of miscarriage;
- suspicion of detachment of the ovum;
- distinguishing the fertilized egg from a pathological formation in the uterus;
- assessment of the condition of the scar that remained on the uterus after a previous cesarean section;
- selection of the method of delivery based on the data obtained;
- complete and partial hydatidiform mole;
- determination of the position of the fetal egg in the uterus, the state of its attachment (presentation, low location).
TVUS during pregnancy allows you to determine the number of fetuses in the uterus, heart rate, and possible malformations. This type of study accurately determines the gender of the unborn child.
During pregnancy, transvaginal ultrasound can be done on demand as many times as needed. The sensor and ultrasound radiation are not able to affect the condition of the fetus and the pregnant woman herself.
Types and Applications of Ultrasonic Sensors
Authorship of Rus-exp LLC. Copying text without permission of the copyright holder is prohibited.
| Convex ultrasonic sensors: |
Convex sensors are mainly used as basic sensors for diagnosing the abdominal area (abdominal cavity: liver, kidneys, gallbladder, pancreas, spleen) and pelvic organs (bladder, uterus, ovaries), and the fetus in the late stages of pregnancy.
They have a curved surface, which is due to their anatomical applicability. They are characterized by the radius of curvature, frequency range and electronic scanning angle. The radius of curvature R varies from 40 to 70 mm. Sometimes, instead of the radius of curvature, characteristics such as aperture and scanning surface (footprint) are used. There is an important difference between them: the scanning surface is the area of the sensor that looks like a rubber surface on the outside (gray, blue, black or red depending on the sensor manufacturer). Aperture is a scanning area that is displayed on the instrument screen and can only be measured in width on the screen. The aperture is always smaller than the scanning surface. The electronic scanning angle for convex sensors varies mainly from 60 to 70 degrees, although recently devices have appeared with the function of expanding the scanning field (up to 110 degrees). The frequency range of convex sensors can be as follows: 1-5 MHz or 2-6 MHz - for adult obese patients, deep organs, fetus; 2-8 MHz or 3-8 MHz - for fetal examination and diagnostics in pediatrics (with such sensors the fetus can be visualized more clearly, however, for deep organs such as the liver, the beam penetration depth is not enough, so this sensor is recommended only for obstetric applications); 5-10 MHz or 5-13 MHz - for neonatal diagnostics or specific studies. Example: C251/C35 sensor for FUJIFILM (HITACHI)
| Microconvex intracavitary sensor |
Microconvex ultrasonic sensors are analogous to convex sensors in their design, but with a much smaller scanning head compared to convex sensors. Microconvex sensors can be for external and intracavitary use. Intracavitary microconvex sensors are divided into three types: transvaginal, transrectal and universal recto-vaginal. Transvaginal sensors are used for diagnosing the pelvic organs and fetus at an early stage of pregnancy (first trimester), have an oblique view relative to the sensor axis (this is done taking into account the anatomical shape and position of the uterus), the radius of curvature is usually from 9 to 14 mm, the frequency range is 4- 9 MHz (higher frequencies are not required, since the uterus is located at a certain, very specifically defined depth). Transvaginal sensors can have a straight or beveled handle. The beveled handle is used for ease of diagnosis in the gynecological chair. Also, the beveled handle is convenient when taking a biopsy or performing an in vitro fertilization (IVF) procedure. The scanning angle for transvaginal sensors is from 120 to 140 degrees (the uterus falls into this field). Transrectal intracavitary microconvex probes are used to diagnose the prostate gland (prostate) and take prostate biopsies. They have a direct view (end-fire), a straight handle and a symmetrical head (to make it easier to rotate the sensor around its axis to examine different projections). Often such sensors have additional devices for performing prostate biopsy: for example, a biopsy channel, a biopsy guide included in the basic kit. FUJIFILM / HITACHI / ALOKA sensors also have a dismountable handle for installing a syringe and measuring ruler. They have a radius of curvature of 8-11 mm, a wide scanning angle (from 120 to 150 degrees). The frequency range required for prostate scanning is 5 to 10 MHz (or higher). Also, such sensors usually have a shorter working (inserted) part compared to transvaginal and universal rectovaginal sensors. Universal rectal-vaginal sensors are a combination of transrectal and transvaginal sensors into one. This is convenient for mass screening, when specific procedures such as IVF and biopsy are not required. In addition, such sensors are cheaper than highly specialized ones separately. They have a straight handle, a small radius of curvature of 8-11 mm, and a direct, wide view. Versatility is achieved by a large scanning angle from 150 to 210 degrees, covering any needs, as well as a wide frequency range of 4-9 MHz (or wider depending on the manufacturer).

| Microconvex outdoor and operational sensors |
Microconvex sensors for external use have a radius of curvature of less than 30 mm and are mainly used either for the diagnosis of newborns (mainly neurosonography) or for specific purposes: operating and surgical applications, lithotripsy monitoring, veterinary medicine. Ultrasonic frequencies: 2-5 MHz, 1-6 MHz - low-frequency sensors for monitoring lithotripsy and liver surgery. 5-10 MHz (or wider) - high-frequency sensors for neonatology, neurosonography of newborns, surgical applications (including on the liver).
Depending on the application, they can have a direct view (usually 60-80 degrees, although there are 110-150 degrees) - for neonatology and veterinary medicine, biopsy control and surgery. Or they can have a side view: T-shaped (for example, Professor Makuuchi’s operating sensors for liver surgery) or I-shaped.
Examples (from left to right): Neonatology and Veterinary Microconvex Probe, C22T/C42T T-Probe, UST-9132I I-Probe
| Linear ultrasonic sensors: |
Linear sensors have a flat emitting surface. They differ in aperture and frequency range. 80-100 mm - extra-long sensors. Previously, such sensors were used to diagnose the abdominal cavity, when convex sensors did not yet exist. At the moment, their use is limited to specific areas. For example, the low-frequency FUJIFILM (HITACHI) ALOKA UST-5045P-3.5 probe with a cutout in the working surface is used for abdominal biopsy, and the high-frequency FUJIFILM (HITACHI) EUP-L53L probe is used for ductal radial diagnostics of the breast. 50-60 mm - sensors for studies of superficial small organs. For a given sensor size, these are the breast and thyroid glands. The aperture of 50-60 mm is determined by the anatomical dimensions of these glands. However, for the diagnosis of blood vessels, eyes, and joints, such an aperture will not be convenient or not applicable at all. It is also worth considering that 50-60 mm is the aperture, and the scanning surface (footprint) is even wider by 10-15%, so the physical width of such a sensor can reach 6-7 cm. The frequency range is 5-13 MHz. FUJIFILM (HITACHI) ALOKA has developed the UST-567 sensor for diagnosing the breast and thyroid gland, which is characterized by its ultra-light weight and super-elastic cable, which greatly reduces the load on the doctor’s hand during this diagnosis. 35-45 mm are the most versatile linear sensors for mass screening. Convenient for both blood vessels and small organs (glands, joints, muscles, eyes). The small field of electronic scanning (aperture) is compensated by such modern modes as trapezoidal scanning (trapezoid), or virtual convex (virtual convex), expanding the scanning area at the edges. Panoramic scanning (EFV) and B-beam tilting technologies (steering) can also be used to expand the area. For studies of superficial vessels, such sensors have an electronic tilting mode of the Doppler window (steering) for the correct location of the blood flow relative to the sensor (previously, angled adapters-nozzles were used for this). Sensors with a 35-45 mm aperture can have different frequency ranges: 3-8 MHz for deep vessels (veins of the lower extremities), 5-13 MHz for small organs and vessels, 7-18 MHz for superficial structures, muscles, nerves. . 20-30 mm - linear sensors for musculoskeletal studies (muscles, joints) and subcutaneous vessels, have frequencies of 7-18 MHz. 5-20 mm - intraoperative and microtissue sensors having a specific T-, L-, I-shape, laparoscopic or finger sensors. Their shape and characteristics are determined by the specific application for each specific case.
Examples of linear transducers (from left to right): L441 38 mm aperture universal transducer, L53K intraoperative stick transducer, EUP-L53L extra-long linear transducer
| Sector phased sensors (phased array): |
These sensors have different imaging technology. If in the convex and linear sensors discussed above, the scanning area is determined by the geometry of the sensor, then in phased sensors this is not the case. Each element of these sensors operates independently of each other. The resulting image has a very narrow near field and a wide far field. The scanning surface is small in size, which allows scanning in hard-to-reach places (the heart between the ribs, the brain through “windows” in the skull). The scanning angle is 90 degrees (allows you to capture the heart) in most cases, although premium cardiac ultrasound systems offer an extension of up to 120 degrees and a virtual apex mode (near field extension). These sensors have a high frame update rate. They are used in cardiology (EchoCG) and for transcranial Doppler (TCD / TCD): - Frequencies 1-5 MHz, 2-5 MHz, 2-4 MHz, scanning surface 19-25 mm. Such sensors are used for transthoracic echocardiography and transcranial diagnostics in adult patients. Sensors with a frequency of 5 MHz can also be used in pediatric patients from 6 years of age. — Frequencies 3-7 MHz, 3-8 MHz, scanning surface 10-15 mm. Used for transthoracic echocardiography in pediatrics and neonatology. — Frequencies 5-10 MHz, scanning surface 10 mm. Used for transthoracic echocardiography in newborns. A distinctive feature of phased-phase sensors is that they can operate in constant-wave (continuous wave) CW Doppler mode, which is necessary when examining the heart. It is also worth noting the relatively low reliability of these sensors due to technological features. Typically their service life is much shorter than other types of sensors.
| Transesophageal/transesophageal echocardiography (TEE) sensors: |
Transesophageal echocardiography (TEE) is a transesophageal examination of the heart. Unlike transthoracic echocardiography, where there are enough muscles and ribs between the sensor and the heart that complicate diagnosis, from the esophagus to the mitral valve the distance is measured by a centimeter and there are no bones. The TEE sensor is inserted into the esophagus through the mouthpiece. The sensor has a flexible working part and a flexible distal tip, and is very similar in appearance and control to a gastrofibroscope. The distal tip can move in different directions, which allows you to obtain high-quality images of the heart in dynamics in various projections. Modern TEE sensors have a rotating (rotating) emitter, which also makes it possible to obtain different projections of the heart. Such sensors are available with manual or automated (motorized) drive. Matrix TEE transducers are available in premium echocardiographic ultrasound systems for real-time three-dimensional cardiac reconstruction (4D-TEE). TEE sensors have a frequency range of 3-8 MHz or 2-9 MHz, electronic scanning angle is 90 degrees. Adult, pediatric and neonatal TEE sensors differ in working length, insertion diameter and distal tip diameter. Like fiberscopes, such sensors require special disinfection and storage, and very careful handling. G
| Bi-plane and tri-plane transrectal sensors: |
Such sensors have two or three emitters. Their application: diagnosis, as well as planning and monitoring of prostate brachytherapy. The use of several emitters is due to the need to obtain sections of the prostate in distinct projections. Transrectal access, due to anatomical features, does not provide sufficient degrees of freedom when manipulating a standard transrectal sensor. In bi-plane sensors, linear + microconvex emitters or microconvex + microconvex emitters are placed on one sensor. Each emitter scans in its own projection (for example, one in the sagittal projection, the other in the frontal projection). Specialized urological ultrasound devices from BK Medical also have three-plane sensors with three emitters. Bi-plane sensors are mainly used to monitor prostate biopsy or brachytherapy. You can read an article about prostate brachytherapy here. It is also worth noting that with linear emitter rectal probes, only transperineal prostate biopsies are available (i.e., through the perineum, not transrectally).

| Mechanical sensors: |
Mechanical sensors have a moving emitter. Previously, in the absence of electronic scanning technology, these sensors were used to obtain a two-dimensional image. Currently, mechanical sensors are sometimes used for specific intracavitary studies: anorectal zone, transurethral, intravascular - radial mechanical scanning is used in such studies.
| Volumetric 3D/4D real-time three-dimensional scanning sensors: |
Mechanical sensors with angular rotation. Used for three-dimensional scanning. Due to the mechanical rotation of the emitter, a cross-sectional scanning of the organ occurs, after which the data in the scanner is reconstructed into a three-dimensional image. With one rotation of the emitters, a static 3D image is obtained; with constant rotation, a dynamic three-dimensional scanning in real time is obtained (Real Time 3D, 4D). The emitter itself in such sensors can be anything: convex, microconvex, linear, phased, depending on their application. As well as conventional sensors, 3D convex sensor is used for the abdominal cavity and fetus, 3D microconvex sensor for early stages of pregnancy and uterine diagnostics, 3D linear for small organs, 3D phased for the heart. In addition to three-dimensional scanning, 3D sensors allow you to obtain sections (projections) in 2D mode, which are not available with other types of sensors. For example, a volumetric transvaginal sensor, which allows you to obtain two-dimensional projections that cannot be obtained with a standard transvaginal sensor due to the anatomical features of transvaginal access. A 3D linear sensor allows you to obtain a coronal projection of the mammary gland (see article here).
| Matrix sensors: |
Unlike the types discussed above, such sensors have a grid with several rows of piezoelements (emitters). Matrix sensors are divided into two categories: - 1.5D (one and a half dimensional) - for such sensors the number of elements in the aperture width is much less than in the length. For example, 3 x 128 or 5 x 192 elements. This was done to improve thickness focusing and reduce noise associated with the scattering of ultrasonic waves on parallel layers “invisible” to devices (in conventional one-dimensional sensors this is done using an acoustic lens or other methods). But three-dimensional volume cannot be obtained with such sensors. Not all manufacturers use matrix sensors in their product range. This is due not so much to the technological difficulties of development, but to the high cost of their production (and correspondingly high price for the end user) and only a slight improvement in image quality (signal-to-noise ratio). Many sensors with 192 elements can produce significantly better images than 1.5D matrix sensors with more elements. FUJIFILM (HITACHI) uses full-aperture apodization technology instead of matrix technology and Smart Probe multilayer crystal sensors, which achieves similar imaging quality. — 2D (two-dimensional). The aperture is a matrix with a large number of elements along the length and width of the aperture. These sensors allow you to obtain a three-dimensional image of the heart in real time, as well as simultaneously display multiple projections and slices in real time.
Example: 4D-TEE transesophageal matrix sensor FUJIFILM (HITACHI) MXS2ESLL1
| Monocrystal sensors |
Monocrystal sensors use piezoelectric elements made and cut from a single grown crystal. This allows you to obtain more consistent characteristics of the piezoelectric elements (frequency response). The images obtained from such sensors are less noisy. Monocrystal sensors can be either convex or linear, phased sensors.
Example: single-crystal cardiac sensors FUJIFILM (HITACHI) S211 / S12 / S121
| CMUT membrane sensors |
CMUT (from the English “Capacitive Micro-machined Ultrasound Transducer” or “ultrasonic sensor on moving capacitive microelements”) is a new generation of ultrasonic sensors that use a matrix of micromembranes instead of piezoelectric crystals (piezoelements). The use of this technology has made it possible to radically expand the range of ultrasonic frequencies available on a single sensor. The FUJIFILM (HITACHI) SML44 sensor with linear emitter CMUT has a frequency range of 2-22 MHz, which allows it to be used for almost the whole body. Expansion of the scanning area is achieved through the use of virtual convex (trapezoidal scanning).
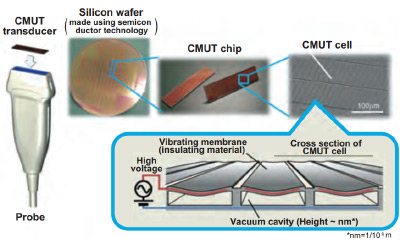
Example: CMUT sensor FUJIFILM (HITACHI) SML44
| Pencil Doppler (blind CW) sensors: |
Sensors with separate receiver and emitter. Such sensors operate only in constant wave (continuous wave) CW Doppler mode. They do not work in B-mode or color mode, so they are often called “blind”. The doctor finds the required vessel “by touch” and obtains a spectrum. Used for large arteries and veins of the limbs, neck - 4-8 MHz, or for the heart - 2 MHz. Pencil sensors were often used in the past when there were no other ways to obtain the CW spectrum, but CW Doppler can now be used on phased sector sensors. Therefore, the popularity of pencil sensors has fallen sharply. However, even now they are sold for modern devices, have a low price, and are usually connected to the device through a separate mini-port.
| Video endoscopic sensors (EUS): |
Sensors that combine a video gastrofibroscope or video bronchofibroscope and ultrasound. They are called EUS (Endoscopic Ultrasound, or endoscopic ultrasound). They work together with a video endoscopic stand from a third-party manufacturer - OLYMPUS, PENTAX. According to their purpose, they are distinguished between gastroscopic (for diagnosing the gastrointestinal tract) and bronchoscopic (for diagnosing the lungs). They can be equipped with an internal instrumental channel for taking biopsies and manipulations. By type of emitter there are convex / micro-covex and radial (with a 360-degree view). They are an example of multimodal image acquisition, when an image from two dissimilar imaging systems is displayed on one screen—ultrasound and video from an endoscope. Such systems are very expensive (more expensive than the ultrasound machine and video endoscopic stand taken separately).
| Needle (catheter) sensors: |
Catheter-type microsensors for insertion into hard-to-reach cavities, vessels, and the heart.
| Laparoscopic sensors: |
They are a thin tube with an emitter at the end. The sensor is used in conjunction with a trocar (usually 12 mm) and can be used for monitoring during laparoscopic operations. The tip of the sensor may bend in one or two planes, or may not bend at all (rigid laparoscope). It is controlled by a joystick similar to a flexible fiberscope. The emitter can be linear side-view (UST-5550, UST-5418, L44LA, L44LA1), convex side-view (EUP-OL531, EUP-OL334), or phased with direct view (UST-52109).
Example: L44LA laparoscopic probe with 4-way flexible tip.
Authorship of Rus-exp LLC. Copying text without permission of the copyright holder is prohibited! You can buy ultrasound machines and sensors from our official distributor of FUJIFILM (HITACHI) and ALOKA.
To order, please contact us by email. You can also contact us by phone or through the feedback form in the Contacts section. ARTICLE CATALOG USIC CATALOG OF SENSORS
How is a transvaginal examination done?
To undergo an intravaginal examination, the patient needs to undress from the waist down and lie down on the couch, spreading her legs slightly to the sides. The diagnostician usually asks why the woman was sent for an ultrasound and what complaints she has. This information is necessary in order to pay special attention and examine the most interesting pelvic organs at multiple magnification. In this case, the examination involves a complete and thorough examination of the condition of the patient’s entire genitourinary system.
The procedure is carried out as follows:
1. The doctor places a medical condom on the ultrasound sensor and lubricates it with a special gel, which facilitates its penetration into the vagina and eliminates the air space between the transducer and the organs being examined.
2. The doctor performs all movements slowly and carefully, so there is no discomfort during the procedure. A woman can feel pain only if there is an inflammatory focus in the area being examined. If any discomfort occurs, you should immediately report this to your diagnostician.
3. An exact image of the organs being examined is visualized on the monitor of the ultrasound machine; the doctor can enlarge the resulting image many times and view the elements of interest in great detail.
4. Having recorded all the necessary data, the doctor removes the sensor from the vagina. The woman can get dressed and pick up the ultrasound results, which are later deciphered by the doctor who referred for the study.
What does the sensor look like?
This special tube with a camera at the end. The diameter of the transvaginal sensor is only 3 cm, and the total length is 12 centimeters. Often there is a channel inside such a device where a biopsy needle can be placed.
You will be interested in: Neurosurgeon in Chelyabinsk: list, selection, ranking of the best, clinics, medical centers and hospitals in the city, quality of treatment and patient reviews
Due to the peculiarities of the anatomical structure of the body and the specific location of the uterus, the sensor is designed with an oblique view relative to its axis. Thanks to this, ultrasound with a transvaginal probe is more convenient.

There are several types of device. Some clinics prefer a straight-handle probe to perform routine gynecological procedures. Reproductive health centers almost always use a sensor that has a beveled handle, thanks to which in vitro fertilization or biopsy can be performed.
A transvaginal sensor with a beveled handle is more convenient and ergonomic for examinations in the gynecologist's chair.
Preparation for TVUS
Intravaginal ultrasound is distinguished not only by its ease of implementation with high information content, but also by the lack of preparation for this examination. There is no need to drink water to fill the bladder; the transvaginal sensor clearly visualizes the uterus, ovaries, fallopian tubes, ligaments and adjacent organs without additional manipulation.
Only patients suffering from severe flatulence need specific preparation:
1. 2 days before the test, you should limit the consumption of foods that increase gas formation in the intestines: baked goods, fresh vegetables and fruits, dairy products.2. On the day of the TVUS, the doctor may prescribe you to take Enzistal, Espumisan, activated charcoal or Smecta. The drug is selected by the doctor based on the patient’s tolerance to the active ingredients of the drug and cannot be chosen at his own discretion. Transvaginal ultrasound examination for pregnant women is recommended to be carried out on a moderately full bladder, so for such patients a preliminary visit to the toilet is not required.
Preparation
The accuracy of a gynecological examination of the pelvic organs depends on proper preparation of the body for diagnosis.
Transvaginal examination is done with an empty bladder.
Before it is carried out you must:
- do not drink an hour before the procedure;
- immediately before the ultrasound, go to the toilet;
- if you suffer from increased gas formation, take Espumisan or Smecta an hour before the test;
- a few days before diagnosis, exclude from the diet foods that contribute to gas formation (bread, confectionery, dairy products, carbonated drinks).
If gas formation occurs frequently, it is necessary to take medications that will reduce its occurrence (for example, activated carbon).
Important! Before performing a vaginal ultrasound, cleansing enemas are prohibited.
On what day of the menstrual cycle is TVUS performed?
Women often ask whether it is possible to do a transvaginal ultrasound during menstruation. For the most accurate assessment of the condition of the female genitourinary system (outside the period of pregnancy), it is worth adhering to a certain dependence of TVUS on the day of the menstrual cycle:
1. A planned transvaginal ultrasound should be done on the 5th, 6th or 7th day of the cycle, while the endometrium of the uterus is not yet in the secretory phase. If you ignore this recommendation, the doctor may incorrectly interpret the results of ultrasound diagnostics.2. To determine the presence of a fertilized egg in the uterus and the exact duration of pregnancy, a woman needs to come for a transvaginal ultrasound diagnosis no earlier than the 10th day of the delay.3. If a patient is suspected of having endometriosis, then the study should be planned after ovulation - no earlier than the 14th day of the cycle.4. If uterine fibroids are suspected, a transvaginal ultrasound is performed on days 18-24 of the cycle5. To monitor the patient’s reproductive function, monitor the ovulation process, or determine the cause of hormonal imbalance in the body, transvaginal ultrasound is recommended to be performed on the 10th day of the cycle, and then every 3 days until its end.
However, there are situations when an emergency procedure is necessary, regardless of the day of the cycle:
- sudden disruption of menstrual function: the next menstruation turned out to be more abundant and with clots, longer (longer than 7 days) or did not occur at all within 1 month;
- spotting that the patient does not associate with the onset of menstruation, i.e. they can appear before, after the next menstruation or in the middle of the cycle;
- discharge with blood in pregnant women;
- discharge mixed with blood during or after sexual intercourse;
- the appearance of bleeding in a woman during the menopausal period;
- pain in the lower abdomen.
The appearance of such symptoms should prompt a woman of any age to contact a gynecologist and further undergo a TVUS scan.
Who should undergo an ultrasound with a vaginal sensor?
Any woman can undergo a gynecological ultrasound (both transabdominal and transvaginal) if desired. The only contraindication to ultrasound examination with a vaginal probe is the presence of a hymen. Indications for manipulation:
- pain in the lower abdomen of unknown etiology;
- short term pregnancy, including ectopic;
- menstrual cycle disorders (exclude endometrial hyperplastic processes);
- neoplasms of the appendages and uterus (fibroids, cysts, cancer);
- infertility of any origin;
- follicolometry (in the treatment of infertility, monitoring of ovarian reserve);
- preventive examination);
- inflammatory processes in the pelvis (endometritis, oophoritis, salpingoophoritis, parametritis);
- adhesive disease of the pelvis;
- suspicion of congenital and acquired pathology of the uterus (intrauterine septum, duplication of the uterus, infantile uterus, posterior bending of the uterus, anterior bending, etc.);
- assessment of the position of the intrauterine device (to exclude its partial spontaneous expulsion);
- cervicometry (assessment of the length of the cervix and patency of the cervical canal for isthmic-cervical insufficiency);
- postpartum period (assessment of uterine involution, exclusion of remnants of placental tissue);
- postoperative and post-abortion periods).
Transvaginal ultrasound: photo
Transvaginal ultrasound

Pelvic ultrasound in St. Petersburg

transvaginal ultrasound during pregnancy

transvaginal ultrasound

transvaginal ultrasound
Transvaginal ultrasound at the Diana clinic
Vaginal ultrasound and pregnancy
The study is carried out at the beginning of the term, approximately 4-6 weeks of pregnancy. The method allows you to determine the exact number and degree of viability of embryos. The presence of a fertilized egg is visible within a few days after the delay.
The specialist also checks for the presence of possible fetal pathologies, the threat of miscarriage, the likelihood of placental abruption, and assesses the condition of the periuterine space.
Important! Performing a vaginal ultrasound in the second and third trimester of pregnancy is contraindicated!
After 12 weeks, diagnostics are prescribed only in extreme cases:
- if you suspect premature birth;
- incorrect location of the placenta;
- when assessing the consistency of a scar located on the cervix (for example, obtained after a cesarean section).
In all other cases, specialists perform transabdominal ultrasound in late stages of pregnancy
Read
Also:
- Transvaginal ultrasound in women: how and when to do it, preparation
- DOUBLE - How often and when can you do a pelvic ultrasound
- Vaginal contraceptive ring: how to use it
- How to properly perform vaginal douching?
- How to decipher an ultrasound during pregnancy, what is BPD
- How often and when can you do a pelvic ultrasound?
How often should a transvaginal ultrasound be done?
You need to contact a gynecologist and undergo a transvaginal ultrasound examination every time a woman develops the symptoms and conditions described above in the indications for the procedure. A gynecologist or urologist may prescribe this type of examination if the development of a disease of the genitourinary system is suspected.
If there are no complaints and the woman assesses her condition as satisfactory, she needs to undergo TVUS for preventive purposes at the following frequency:
1. For women with the onset of sexual activity – once every 2 years.2. Women over 40 years old – annually.
If endometriosis is suspected, the procedure is performed in the second half of the cycle. If bleeding occurs in the middle of the cycle, a transvaginal ultrasound is performed urgently to determine the cause of this phenomenon.
Transvaginal ultrasound during advanced pregnancy
Transvaginal ultrasound of a pregnant woman is used only in the first trimester of pregnancy. During this period, the sensor indicates the presence of a fertilized egg, the condition of the placenta, pathologies of fetal development, etc.
During the second and third trimesters, the transabdominal ultrasound method is used predominantly, since inserting a sensor into the vagina can provoke an increase in uterine tone and premature birth. Transvaginal ultrasound is performed according to indications: for example, to determine the length of the cervix and exclude ICI.
Evaluation of TVUS results
Having transvaginal ultrasound data in hand, an experienced specialist can accurately diagnose and select the appropriate treatment for the identified pathology. The results are interpreted by a gynecologist.
About consultation with a gynecologist / Consultation of a gynecologist
Our clinic employs gynecologists of the highest and first certification categories. All doctors have certificates confirming their qualifications, issued in St. Petersburg and Moscow. The cost of an initial appointment with a gynecologist is 1000 rubles, a consultation based on test results or ultrasound is 500 rubles. Appointment with a gynecologist You can make an appointment with a gynecologist without an insurance policy, registration in St. Petersburg and Russian citizenship. We have gynecologists and ultrasound specialists who speak English. You can apply to us without having an insurance policy, registration in St. Petersburg and Russian citizenship. ATTENTION! IN THE CLINIC IS A DOCTOR SPEAKING IN ENGLISH LANGUAGE! Sign up for an appointment with the doctor
During a TVUS, the diagnostician evaluates the following indicators:
Uterus size and position
The size of the organ depends on the individual characteristics of the anatomical structure, the number of pregnancies, childbirths and some other factors. In women who have given birth, the dimensions of this organ are approximately 70 x 60 x 50 mm. If these sizes are much larger than acceptable, the doctor looks for the cause of this pathology.
When performing a transvaginal ultrasound, the position of the uterus is also taken into account. If it is slightly tilted forward, this is considered normal. If its position is shifted back, they speak of a pathological location of the organ.
Echogenicity of the uterus
Here, the structure of the walls and cavity of the organ itself is important; the clarity of the boundaries of the uterus also determines. The presence of hyperechoic areas in the picture may indicate the presence of neoplasms in the uterus.
Endometrial thickness, cervix and endocervix
The inner layer of the uterus changes its thickness depending on the day of the menstrual cycle: at the beginning the endometrium has a thickness of about 3 mm, and at the end it can reach 2 cm. The data obtained on the thickness of the endometrium is compared with the day of the patient’s cycle: if there are discrepancies with the norm, inflammatory process.
Cervix and endocervix . What matters is the structure of the cervix and its size, which normally should correspond to 40 x 30 mm. The cervical canal should have a diameter of less than 3 mm and be filled with mucus.
Sizes and contours of the ovaries
Transvaginal ultrasound perfectly shows the size of the right and left ovaries. At the same time, they may differ slightly, but their total volume should not exceed 10 cubic cm. If this indicator is exceeded, polycystic syndrome or an inflammatory process may be suspected. Their contours can be either smooth or irregular due to the formation of follicles.
Presence of free fluid in the pelvis
A small amount of it can normally be seen in this area, but only immediately after ovulation, which is associated with rupture of the follicle. Otherwise, the fluid may be a sign of ovarian inflammation resulting from an infectious lesion.
Fallopian tubes
They are usually visualized in the presence of an ectopic pregnancy or an inflammatory process in them. To diagnose tubal patency, a contrast agent is used. Already at the stage of ultrasound diagnostics - transvaginal ultrasound, the doctor can determine the following pathological conditions:
- inflammation of the fallopian tubes, ovaries or endometrium of the uterus;
- polycystic ovary syndrome;
- ovarian cyst;
- endometriosis of the uterus and nearby organs;
- polyps or uterine fibroids;
- cancer of the ovary, uterus or cervix.
Normal indicators during the study
The conclusion of a transvaginal ultrasound indicates the ultrasound signs of the identified pathology, and the final diagnosis is established by an obstetrician-gynecologist. Normal results are usually designated as follows: “No ultrasound signs of pathology of the pelvic organs were identified.”
Pregnancy is a separate issue. During a normal pregnancy, the uterus is in normal tone, enlarged in accordance with the term, and there are no signs of chorionic detachment. At 5–6 weeks, the heartbeat of the embryo becomes audible.
A decrease in the size of the organs of the reproductive system after the onset of menopause is considered normal. These are natural age-related changes in the body.
Uterus
A healthy uterus has smooth and clear contours, uniform echogenicity, tilted anteriorly (anteflexio) or posteriorly (retroflexio). The second option of uterine inclination creates difficulties in conceiving and carrying a pregnancy. Painful menstruation and a tendency to constipation are possible.
Dimensions of the non-pregnant uterus in women of reproductive age:
- length: 70 mm;
- width: 60 mm;
- anterior-posterior size: 40–42 mm.
The uterine cavity is normally homogeneous with clear, even edges, without pathological neoplasms. The thickness of the endometrium (inner layer of the uterus) depends on the menstrual cycle:
- 3–4 days of the cycle: less than 3 mm;
- on days 5–7: within 3–6 mm;
- on days 11–14: about 8–15 mm;
- on days 15–19: up to 10–16 mm;
- on the eve of menstruation: no more than 10–20 mm;
- decidualization of the endometrium – possible pregnancy.

Cervix
A healthy cervix has a homogeneous echostructure without pathological inclusions. The cervical canal is up to 3 mm in diameter and contains mucus of a homogeneous echostructure. Both pharynx of the cervix (external, internal) are closed.
Dimensions of the cervix during transvaginal examination:
- length: 35–40 mm;
- anterior-posterior size: 2.5–3 mm.
Ovaries
The ovaries are located on the sides of the uterus, slightly behind it, connected to it by the fallopian tubes. The ovaries have a homogeneous echostructure with small areas of fibrosis, clear contours, and a bumpy surface due to the presence of follicles. A slight difference in the size of the right and left ovaries on ultrasound is considered normal.
Dimensions:
- length: 20–37 mm;
- width: 18–30 mm;
- thickness: 16–22 mm;
- volume: 4–10 cu.m. cm
Depending on the day of the cycle, the number and size of follicles vary. In the first half of the cycle, there are up to 10 follicles with a diameter of less than 6 mm and 1 dominant one. The maximum size of the dominant follicle before ovulation is 20 mm.
In the second phase of the cycle, a corpus luteum is detected at the site of the burst follicle, which decreases from 25–27 mm until it completely disappears by the time of menstruation.

Fallopian tubes
Unchanged uterine (fallopian) tubes are not visualized during transvaginal ultrasound.
Free liquid
In the first days after the rupture of the dominant follicle, a small volume of free fluid accumulates in the retrouterine space. This is considered the norm. There should be no free fluid on other days.
Interpretation of transvaginal ultrasound: table of indicators and diseases
| Genitals | Normal indicators | Deviations |
| Uterus | Anteflexio (anterior tilt); The contours of the uterus are smooth and clear; Dimensions of the uterus: length - 7 cm, width - 6 cm, diameter - about 4 cm; Homogeneous echogenicity of the walls; Homogeneous structure; Crisp and smooth edges | Retroflexio is a variant of the norm that prevents conception; Uneven contours indicate inflammation in the uterus and tissues or tumors of various origins; Heterogeneous echogenicity is a sign of a tumor; Hyperechoic formations (polyps, tumors, myomatous nodes); Heterogeneous structure: a sign of endometritis |
| Cervix | Dimensions: anteroposterior size - 2-3 mm, length - 3-4 cm. Diameter of the cervical canal: 2-3 mm. Homogeneous echostructure. Mucus of homogeneous echostructure. | Increased size of the cervix and cervical canal Heterogeneous structure |
| Free liquid | Normally, its amount is several mm. | A large amount of fluid is a sign of infection |
| Ovaries | Dimensions: width - 2.5 cm, length - 3 cm, thickness - 1.5 cm. Normal volume: 2-8 cm³; Fuzzy, lumpy contours. Homogeneous structure, small areas of fibrosis; In the middle of the cycle, follicles 4-6 mm in size and one dominant follicle up to 2 cm in size are formed | Increase in size (inflammation, polycystic disease) Large fibrous foci (inflammatory process). The size of the dominant follicle is greater than 2.5 cm (follicular cyst) |
| The fallopian tubes | Almost invisible | Clearly visualized (a sign of ectopic pregnancy or inflammation) |
Echo signs of uterine pathologies
| Pathology | Features |
| Uterine cancer | Changes in the contours of the uterus, swelling |
| Myoma | Increased size of the uterine body, altered contours, “hyperechoic zone” (nodule in the muscle) |
| Polyps | Fuzzy contours of the uterus, space-occupying formations in the uterus |
| Endometriosis | “Bubbles” on the cervix, in the tubes and in the uterus itself |
| Adnexit | Thickening of the fallopian tubes, enlarged ovaries, unclear and blurry contours |
| Ovarian cancer | Increase in size with deformation of contours |
| Ovarian cyst | Accumulation of fluid with a diameter greater than 25 mm |
| Endometritis | Swelling of the endometrial layer, increased size of the uterus, thickening of the walls |
| Cervical tumor | Deformation and enlargement of the cervix |
Timely diagnosis and identification of pathological processes in the genitourinary system allows, in most cases, to manage only with drug therapy. Only in rare cases are identified problems solved exclusively by surgery. This speaks to the importance of an annual preventive examination by a gynecologist and undergoing a transvaginal ultrasound by a good specialist.
CLICK TO MAKE AN APPOINTMENT, TEST OR ULTRASOUND
If you find an error, please select a piece of text and press Ctrl+Enter
Decoding the results
Decoding the results includes:
- location, structure and size of the cervix;
- ovarian structure;
- places where the fallopian tubes exit;
- size and number of mature and emerging follicles;
- the amount of free fluid in the abdominal cavity.
The generally accepted standards for the main research indicators are as follows:
- Uterus. Length - 65-75 mm, width - 55-65 mm, diameter - 39-43 mm.
- Endometrium. The thickness depends on the phase of the cycle: 1 week - 3-8 mm, 2 - 7-16 mm, 3 - 10-18. Before the onset of menstruation it reaches 20 mm.
- Ovaries. Length - 20-25 mm, width - 12-15 mm, thickness 9-12 mm, volume - 1.5-4 cubic meters.
The fallopian tubes are not visible in normal condition; they are visible only during an ectopic pregnancy or the presence of inflammatory diseases. An enlarged uterus in the absence of pregnancy indicates a hydatidiform mole.
Irregular shape and unclear contours of the uterus indicate the presence of oncological processes. A large number of calcifications with compaction of 2 mm or more indicates inflammation of the appendages. The development of cancer is indicated by thickening of the walls of the cervix and/or fallopian tubes.
A vaginal examination alone does not make an accurate diagnosis. An ultrasound is performed to examine the general condition of the organs. If there are disturbances in their work, additional narrow-profile diagnostics are prescribed.
How to prepare for this ultrasound method
Before coming to the ultrasound examination room, you need to prepare a diaper or towel that is placed on the couch. In paid clinics, a disposable sheet is already included in the cost of an ultrasound scan.
To prepare for an ultrasound, it is ideal to drink a drug that reduces gas formation (Filtrum, Smecta, activated carbon or others) the day before the procedure. Also limit your intake of foods that cause bloating.
One more point: before carrying out this examination method, you must empty your bladder.
Some patients ask whether it is possible to have sex before the procedure. It is usually prohibited when collecting vaginal smears. With a transvaginal ultrasound, sex will not affect the results in any way.
Optimal time for the procedure
Your attending physician will answer this question for you. The timing of the survey depends on the specific objectives of the survey. We will only talk about a few common features:
- If a woman experiences bleeding on any days other than menstrual days, urgent diagnosis is necessary, as this may be a sign of pathologies that require urgent treatment.
- To check for endometriosis, you need to come for an ultrasound in the second half of the cycle.
- To determine the causes of infertility or during preparation for conception, transvaginal ultrasound is performed three times a month: on the 8-9th day of the cycle, on the 15-16th and after the 22nd day.
Planned procedures are carried out immediately after the patient’s period ends.
How is a pelvic ultrasound performed using a transvaginal sensor?
The sensor is inserted into the woman's vagina. Before the examination, the patient is naked from the waist down and takes a comfortable position on the couch. For hygiene purposes, a condom must be placed on the sensor, which is then lubricated with a special gel intended for ultrasound diagnostics.

The size of the transvaginal sensor is small (approximately 12 cm depending on the model), so it is easily inserted, and the woman does not experience any discomfort. If they occur, you should immediately inform your doctor about it. When a biopsy is necessary, it is performed during the examination using a needle attached to the end of the probe.
During the procedure, the doctor will slightly move the sensor inside the vagina, but this, as a rule, does not affect the sensations. Most women who have undergone the procedure note a complete absence of unpleasant moments.