Humanity realized the danger posed by the human immunodeficiency virus (HIV) too late.
The disease it causes is acquired immunodeficiency syndrome (AIDS).
True, at the beginning of the 21st century, doctors have learned to effectively fight this infection.
No one will deny that the leading role in this direction was played by the improvement of laboratory methods for detecting infection.
As well as studies of blood parameters of already infected people.
Types of analyzes
According to its characteristics, HIV belongs to the category of blood-borne infections.
Infection of a healthy person occurs when the pathogen enters the bloodstream.
There, the virus binds to lymphocytes and other targets and begins active replication.
Infected cells do not immediately become exhausted and die.
Due to this, immunodeficiency occurs.
Thanks to the compensatory abilities of the human body, the infection remains asymptomatic for a very long time (up to several years).
This is the main danger of infection.
The only thing that can be informative in the initial stages of the disease is blood tests.
In clinical practice they are used in different areas:
- primary diagnosis is research that directly indicates the presence or absence of HIV infection in the body of the person being examined
- immunogram - aimed at assessing indicators of the immune system, such as the number of CD4 lymphocytes, which are the main target for viruses
- viral load – helps to assess the degree of infection activity and the effectiveness of antiretroviral therapy
- a complete blood test (CBC), which is performed on infected people for a general assessment of the body's damage to the virus
- biochemical studies allow us to assess the function of the main vital organs - liver, kidneys, hematopoietic system, and so on
The difficulty is that the indicators of the last two points change mainly in the advanced stages of the disease.
But if a person is diagnosed on time and finds out about his status, he can now keep the disease under complete control.
You just need to register with a specialized center and take the necessary tests on time.
We propose to consider a typical algorithm for examining a patient in the form of the following table:
| Blood for HIV | Express method and ELISA in situations where there is a risk of infection or with characteristic symptoms (fever, swollen lymph nodes, frequent colds, diarrhea, weight loss, etc.) |
| Reanalysis | Positive response from the first study. |
| Clinical blood test | Establishing a diagnosis of HIV infection, in the future - according to indications |
| Blood chemistry | Establishing a diagnosis of HIV infection, in the future - according to indications |
| Blood for CD-4 cells | Establishing a diagnosis of HIV infection, first twice with a period of 7 days, then every 6-12 months, if health deteriorates - immediately |
| Viral load | Establishing a diagnosis of HIV infection before starting ART and then - after 3 months until negative results are obtained, then every 6 months |
Like any pathology, HIV infection has individual characteristics for each infected person.
Therefore, the proposed table is only a guide.
The exact timing and list of necessary tests are prescribed by the doctor who is caring for the patient.
The timing of monitoring examinations is also changing after a patient begins taking antiretroviral therapy (ART).
Decoding HIV test results
Given that viral load can rise and fall naturally, viral load is not assessed separately from CD4 count. In other words, if the CD4 count is normal, but the viral load has increased, then this is not a cause for concern. Conversely, if the viral load increases against the background of a decrease in CD4 levels, then “it’s time to sound the alarm.”
The results obtained during the viral load study are interpreted as follows.
- Up to 10,000 copies of the virus – low viral load.
- Over 100,000 copies – high viral load.
- 0 copies – there is no virus in the body, which is considered the norm for a healthy person and indicates the need for repeated testing for HIV-infected patients.
Undetectable viral load is the minimum number of copies, the presence of which cannot be detected using the selected research method.
Thus, an undetectable viral load is the goal that all HIV-infected patients strive for. This result indicates that there is a virus in the body, but its amount is negligible and at the moment the person is not in danger. In this case, it is imperative to assess the general condition of the immune system. To do this, you need to determine the number of CD4+ antigens of T-lymphocytes. Cell norms and possible deviations are shown in the table below.
| CD4 count | Possible patient actions |
| 1500 – 500 cells/ml | norm |
| 500 – 350 cells/ml | need to start HAART |
| 200 cells/ml and below | administer HAART |
| Less than 100 cells/ml | carry out HAART and symptomatic therapy |
By assessing viral load and CD4 levels, a reliable conclusion can be made about the patient’s health status. If the viral load is low, for example, 4000 copies and CD4 counts are normal, then HAART is effective. And vice versa - a high viral load with a decrease in CD4 counts indicates low effectiveness of treatment.
General blood test indicators for HIV
In the early stages of infection, the indicators of a general blood test change little or even remain within the normal range.

An attentive physician can associate some marginal fluctuations in leukocytes (white blood count) with episodes of repeated recurrent colds and respiratory infections.
In more advanced stages of the disease, when the body’s compensatory capabilities weaken, the following changes occur in the CBC:
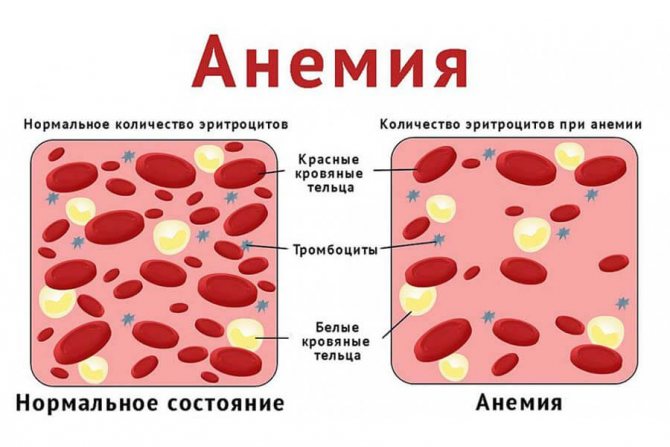
- Anemia. A decrease in the number of red blood cells below the age and gender norm is associated with HIV damage to bone marrow cells and general exhaustion of the body. The degree of anemia correlates with the activity of HIV infection: anemia increases with the progression of the disease and, conversely, recedes during ART therapy.
- Leukopenia and lymphopenia are typical phenomena for HIV. A general blood test can detect a persistent decrease in the number of leukocytes (below 4*10 to the 9th degree) and lymphocytes (below 13%), the indicators of these cells help doctors make a preliminary prognosis and develop measures to protect a person from other infections (for example, prescribe biseptol prophylaxis ).
- Thrombocytopenia. A drop in platelet levels below normal (180*10 to the 9th power) is very typical for HIV infection; within 10 years, this phenomenon occurs in 45% of infected people. Thrombocytopenia is caused by two mechanisms: autoimmune damage to thrombocytopenia and a decrease in the number of their precursors (megakaryocytes).
It is very important for the patient to comply with the deadlines when the doctor recommends taking the OAC.
This will help you notice dangerous complications of HIV infection in time and prevent them.
In addition, we must not forget about the risk of developing adverse reactions in response to pre-drug ART therapy.
What is HIV infection

This is an infectious disease caused by the human immunodeficiency virus (HIV). The disease is characterized by latent and slow progression. The virus primarily affects immune blood cell structures (lymphocytes, macrophages, microglia). Getting inside immune cells, it destroys their ability to recognize foreign agents. Then the multiplied virus “releases” into the biological fluid. The host cell dies and the virus colonizes healthy cells.
At first, the body copes with the infection by producing a large number of new cells to replace the massive death of the affected ones. As the disease progresses, compensation becomes insufficient. As a result, the number of immune cells decreases sharply, which leads to decreased immunity. The body is left without reliable protection against negative external and internal factors.
Attention! The rapid ability to mutate is one of the characteristics of HIV. Therefore, not a single medicine has yet been created that can eliminate the infection.
The virus enters the body from a human carrier. Infection occurs through contact with infected blood, saliva, breast milk, semen, vaginal secretions, and lymph. It should be borne in mind that infection will occur when the listed biomaterial enters the systemic bloodstream. Therefore, the infection enters the blood through wounds, abrasions, microtraumas of the oral mucosa, genital organs, etc.
The disease lasts from several months to several years. But throughout the entire period, it purposefully destroys the immune system. The infection manifests itself with various symptoms. Acquired immunodeficiency syndrome greatly reduces the body's defenses. As a result, a secondary infection often joins the main disease, and neoplasms of a malignant nature appear.
ESR indicator
A very important data from the CBC is the erythrocyte sedimentation rate, or ESR for short.
The norm is 4-10 mm per hour.
When the ESR accelerates, this indicates an imbalance in the protein balance of the blood.

Unfortunately, the indicator is completely nonspecific: ESR increases with any infection, injury, or oncology.
Patients are characterized by such a combination when the erythrocyte sedimentation rate is increased to 30-40-50 mm per hour.
And the person feels more or less normal.
This picture is associated with a decrease in the number of white blood cells.
In particular, those lymphocytes that synthesize immunoglobulin proteins.
A decrease in the amount of these immune proteins entails a relative increase in albumin proteins, which is reflected in the increase in ESR.
Symptoms that require testing a patient for HIV:
- the patient has an enlargement of two or more lymph nodes;
- constant night sweats;
- diarrhea that lasts a long time;
- sudden weight loss;
- fever of unknown origin;
- pregnancy planning;
- preparation for surgery;
- the following infections: toxoplasmosis, persistent herpes virus infection, pneumonia, frequent casual sexual intercourse, candidiasis, etc.
Patterns and changes in CBC in HIV-infected patients
The presence of HIV pathogens cannot be determined in a general blood test, but some signs of the development of the disease are visible.
Lymphocytes
The normal content of these cells is 25-40% or 1.2-3×109/l. At the beginning of the development of the disease, an increase in this indicator (lymphocytosis) is observed due to the body’s increased fight against viral infection. As the disease progresses and affects the human immune system, a critical decrease in the level of lymphocytes in the blood (lymphopenia) is detected. In HIV, it is mainly the fraction of T-lymphocytes that decreases.
Neutrophils
This type of leukocyte is activated immediately after infection with the virus. Neutrophils carry out the process of phagocytosis (absorption of viral cells). This subsequently leads to their destruction and a decrease in their number - neutropenia. The normal content of these cells is 45-70% or 1.8-6.5 × 109/l. A decrease in the number of neutrophils in the blood is not specific to HIV infection, since the phenomenon is observed in all infectious and inflammatory diseases.
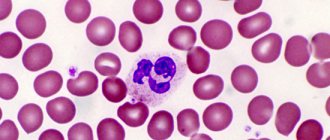
Mononuclear cells
These atypical cells (lymphocytes with one nucleus) are a type of leukocyte. Mononuclear cells appear in a blood test when infectious agents (viruses or bacteria) enter the body. Normally, these immune cells should not be present in the biomaterial.
Platelets
Platelets play an important role in blood clotting processes. Normally, an adult has from 150 to 400 × 109/l blood platelets. When infected with HIV, the platelet count decreases. Clinically, this fact is manifested by the development of various types of bleeding: internal, external; the occurrence of petechiae (pinpoint rash) on the skin and hemorrhages on the mucous membranes.
Red blood cells
This indicator is not so specific for infection with the human immunodeficiency virus. The number of red blood cells often decreases with this pathology. This action occurs due to the influence of the virus on the bone marrow, in which blood formation occurs. The norm is considered to be the content of erythrocytes in biomaterials in the amount of 3.7-5.1 × 1012/l.
However, sometimes an increase in the number of red blood cells is detected in the CBC during immunodeficiency. This occurs in pulmonary diseases accompanying the development of HIV infection. These diseases include pneumonia and tuberculosis.
Hemoglobin
Often with HIV, a decrease in hemoglobin levels is detected, which indicates the development of iron deficiency anemia. Hemoglobin, an iron-containing protein, is located on the surface of red blood cells and is involved in the delivery of oxygen to all cells of the body. When its amount decreases, tissues suffer from hypoxia (oxygen deficiency). Clinically, anemia is manifested by weakness, dizziness, pale skin, and increased heart rate. Normal hemoglobin levels in men are 130-160 g/l, in women – 120-140 g/l.
Erythrocyte sedimentation rate
When infected with HIV, there is a significant increase in this indicator. Normally, in men, ESR ranges from 1 to 10 mm/h, in women – from 2 to 15 mm/h. Acceleration of ESR is not specific for viral damage. A similar sign is characteristic of any infectious and inflammatory processes in the body.
Sometimes, with HIV infection, the ESR may not increase for several years, and then increase sharply.
Thus, a general blood test does not allow 100% detection of the presence and stage of development of HIV infection. However, this research method is important for doctors at the initial stages of diagnosing the disease.
Reasons for the decrease in lymphocytes in the blood
In HIV and other conditions of the body, lymphocytes, which belong to the group of leukocytes, are responsible for cellular immunity, distinguishing between self and foreign proteins. A low level of lymphocytes, the norm of which depends on age, indicates lymphopenia. In the leukocyte formula they must correspond to a certain amount. Acceptable percentage of deviations from the total number of all elements:
- 20 – in adolescents and adults;
- 50 – in children from five to seven years old;
- 30 – in children.

A slight decrease in lymphocytes occurs during infections. In this case, the lesion is rapidly attacked by immune cells, and lymphopenia is temporary. To make a correct diagnosis, it is important to find out as quickly as possible the reason why these cells decreased. A low level of leukocytes is detected in HIV, as well as in:
- miliary tuberculosis;
- severe infections;
- aplastic anemia;
- chronic liver diseases;
- chemotherapy;
- lupus erythematosus;
- destruction of lymphocytes;
- corticosteroid intoxication;
- lymphosarcoma;
- and etc.
Detection of lymphopenia requires immediate treatment of the pathologies that provoked it.