The normal course of pregnancy involves its development in the uterine cavity. The sperm fertilizes the egg in the fallopian tube, through which it then moves into the uterus and is fixed in its mucous membrane. This is how conception occurs, giving the beginning of a new life. However, sometimes this natural system goes wrong and the fertilized egg attaches to the wall of the fallopian tube instead of entering the uterine cavity, which is the most common cause of ectopic pregnancy. There are rare cases of pathologies such as the development of pregnancy in one of the ovaries, the cervix and the abdominal cavity. These violations make up the remaining 5%. It should be noted that with any abnormal attachment to any organ other than the uterus, the fertilized egg is deprived of its normal development due to the fact that there is no prepared mucous membrane in the abdominal organs and fallopian tubes.
The main danger of an ectopic pregnancy, which often does not make itself felt at first and develops asymptomatically, is the rupture of the organ to which the egg was attached, which is often accompanied by heavy bleeding, and in some cases, its amputation. As a result of its development, the egg increases in size, stretching the tube or other organ to which it is attached; the villi of the fertilized egg, the so-called chorion, grow through the blood vessels, which causes the above-mentioned irreversible consequences. A particularly dangerous period in which a rupture of the fallopian tube can occur between 3 and 8 weeks of pregnancy.
Diagnosis of ectopic pregnancy
Symptoms of an ectopic pregnancy in the early stages are identical to the symptoms of normal pregnancy: engorgement of the mammary glands, nipples, drowsiness, changes in taste perception, increased irritability, etc. However, there are a number of distinctive signs, the presence of which should alert a pregnant woman. This is bloody discharge from the genitals, called “spotting”, pain in the lower abdomen of varying intensity. Manifestations such as weakness, nausea and vomiting, stool disorders can also be secondary signs of ectopic pregnancy, but at the same time they can also be symptoms of other pathological processes: the threat of miscarriage during a normal pregnancy, inflammatory diseases of the appendages, ovarian dysfunction and a number of other pathologies of the female genital organs.
Sharp pain in the lower abdomen, as well as pain radiating to the shoulder blade, rectum, shoulder, low blood pressure, increased heart rate, pallor of the skin and mucous tissues, the appearance of cold sweat and even loss of consciousness from painful shock can be symptoms of bleeding into the abdominal cavity which occurred as a result of a ruptured fallopian tube. In this case, immediate assistance from a medical specialist is necessary, whose competent actions will help avoid serious consequences.
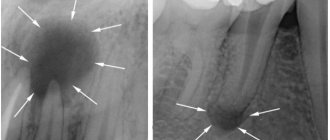
An experienced gynecologist can confirm or rule out an ectopic pregnancy during a routine examination, since severe pain is felt when palpating the patient’s abdomen. To confirm the diagnosis, additional examinations may be prescribed: ultrasound diagnostics, and laboratory testing of a hormone such as the beta subunit of human chorionic gonadotropin, on the presence of which the pregnancy test is based.
Ultrasound diagnosis of the female reproductive system in the early stages of ectopic pregnancy cannot always show a reliable result. There are differences between ultrasound methods: an examination carried out through the abdominal wall (transabdominal ultrasound) is less effective than an ultrasound examination using a probe inserted into the uterine cavity through the vagina, the so-called transvaginal ultrasound, which can detect the presence of a fertilized egg up to four weeks of pregnancy. .
What is it and what happens in a woman’s body?
An ectopic pregnancy is pathological, due to the “incorrectness” of the process, or rather the “failure” of the fertilized egg (fertilized egg) to enter the uterus. For some reason, the egg, after fertilization, is fixed outside the uterus, where it continues its short development.
Depending on the place where the fertilized egg is attached, an ectopic pregnancy occurs:
- tubal (fixed in the fallopian tube);
- ovarian (fixed in the ovary);
- abdominal (attached in the abdominal cavity);
- ectopic pregnancy developing in the rudimentary uterine horn (rare).
The order in this list of types corresponds to the frequency with which deviations occur. In addition, another rare (fortunately) type of ectopic pregnancy occurs in medicine, called heteroscopic pregnancy. In this case we are talking about uterine - normal, and ectopic pregnancies at the same time. That is, a woman ovulated two eggs at once during one menstrual period, and both were fertilized. But one of the fertilized eggs is fixed in the uterus, as it should be, and the second is in a place not intended for it, a tube, an ovary or another.
Causes of ectopic pregnancy
There are a number of reasons that can cause an ectopic pregnancy:
- inflammatory diseases of the uterus and appendages suffered previously;
- ovarian cysts and benign tumors that cause obstruction of the fallopian tube;
- uterine fibroids, localized at the junction of the uterus with the tubes;
- endometriosis in the fallopian tubes;
- adhesions surrounding the fallopian tubes;
- previous surgical interventions on the genital organs;
- previous abortions;
- the presence of intrauterine contraceptives.
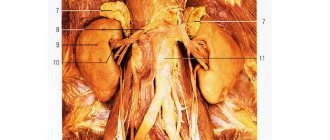
Laparoscopy for adhesions in the pelvis
The presence of adhesions between the pelvic organs interferes with their normal functioning: the normal movement of the egg, sperm or embryo is disrupted, which means infertility develops. The adhesive process develops after surgery, due to inflammatory processes or endometriosis. Laparoscopic adhesiolysis is effectively used to restore the patient's fertility. During the operation, the doctor divides and removes sections of connective tissue between the ovaries, uterus, and fallopian tubes. In particular, peritubar adhesions are removed - adhesions around the fallopian tubes that prevent them from functioning normally.
Treatment methods for ectopic pregnancy
The only way to treat an ectopic pregnancy is to remove the fertilized egg, most often along with the organ where it was located - the fallopian tube. Today, there are two methods of surgical intervention: transection and laparoscopy.
An incision in the abdominal wall, transection, for many years was the only surgical method for removing the fertilized egg. This method is quite effective, but its disadvantages include high traumatism and a long postoperative period.
Modern medicine today has a less traumatic method, in which a video camera, a so-called laparoscope, which expands the capabilities of the surgeon, and the surgical instruments necessary for the operation are inserted through small punctures in the abdominal wall: trocars, which are channels through which scissors and clamps are inserted into the cavity , coagulators and other medical instruments.
Treatment
An obstetrician-gynecologist is involved in the treatment of ectopic pregnancy; if necessary, a surgeon and resuscitator are involved. When determining treatment tactics (performing laparoscopy or laparotomy), the following are used:
- the patient’s desire to preserve reproductive function;
- type of tubal pregnancy termination;
- the degree of blood loss and the severity of the woman’s condition;
- presence of ectopic pregnancies in the past;
- the severity of the adhesive process in the pelvis.
Waiting tactics
The term watchful waiting is usually defined as watchful waiting or close monitoring by health care providers rather than immediate treatment.
Studies have shown that in patients with ectopic pregnancies who are properly evaluated and whose hCG levels decrease, up to 50% of these pregnancies will end naturally, and there will be no need for surgical or drug treatment.
When deciding on the advisability of watchful waiting, doctors first study the results of blood tests, ultrasound, and assess the general state of health. Indications for wait-and-see tactics:
- general health condition is stable;
- the level of pain is considered acceptable;
- Ultrasound shows a small ectopic pregnancy without bleeding into the abdominal cavity.
With expectant management, hCG levels should be assessed every 3-7 days until the level drops to approximately 5000 mIU/ml.
For most women, hCG levels reach non-pregnant levels within about four weeks.
The main risk associated with expectant management is that the ectopic pregnancy may continue to progress and cause the tube to rupture. About 25% of women who are initially under medical supervision nevertheless seek surgical help.
Conservative treatment (methotrexate)
Methotrexate is a drug that suppresses cell growth and is actively used by oncologists.
Intramuscular injection of methotrexate causes the death of the fertilized egg and its organization in the female body. Such treatment is carried out under the following conditions:
- the size of the fertilized egg is no more than 3.5 cm;
- no signs of internal bleeding;
- hCG level is less than 5000 mIU/ml, higher levels are a relative contraindication;
- no evidence of pipe rupture – evidence of pipe rupture is an absolute contraindication
After the injection, the patient can go home immediately, but the doctor will prescribe regular blood tests to assess the effectiveness of the drug.
A woman must use reliable contraception for at least 3 months after treatment. This is because methotrexate can be harmful to the fetus if an intrauterine pregnancy occurs during this time.
Surgical intervention
The only 100% effective way to remove an ectopic pregnancy is surgery.
Laparoscopy is the most gentle method for removing ectopic pregnancy with a low risk of postoperative complications.
Laparotomy with revision of the pelvic organs, removal of blood and clots, and dissection of adhesions is performed in the presence of extensive internal bleeding, severe adhesions, and the patient’s serious condition. The scope of surgery for tubal pregnancy is determined by its location, gestational age, and age of the patient.
In order to preserve the fallopian tube, salpingotomy is performed - dissection of the oviduct, squeezing out the fertilized egg and subsequent suturing of the tube. During fimbrial pregnancy, the fertilized egg is sucked out or squeezed out of the fimbriae of the tube.
If the oviduct is ruptured and there is massive internal bleeding, a salpingectomy is performed - removal of the tube.
Both laparoscopy and laparotomy are performed under general anesthesia. The duration of the operation depends on the technique, the presence of complications, the amount of blood loss, the skill of the surgeon and is 30-90 minutes.
Restoring the menstrual cycle after surgery
The hormonal balance of each woman is individual and after undergoing a pathological process and surgery to remove the fertilized egg, it is therefore difficult to answer unambiguously when the next period will come after an ectopic pregnancy operation. In the absence of significant complications, on average they recover within a period of 28 to 40 days from the day of the operation. Bloody discharge after an ectopic pregnancy operation that appears earlier than this period may be evidence of uterine bleeding rather than restoration of the menstrual cycle, which requires immediate medical intervention. The opposite cases are also known, which can also become a cause for concern - when menstruation after an ectopic pregnancy operation is delayed and does not occur earlier than two months later. The reason for this phenomenon may be late diagnosis of ectopic pregnancy, which increases the recovery period, as well as the stress experienced by the patient before surgery.
How is the operation performed?
Most operations in modern gynecology are performed using laparoscopic access, which has a number of undeniable advantages for both the doctor and the patient. Laparoscopic operations are less traumatic, have a lower risk of complications, less pronounced postoperative pain syndrome, allow for quick rehabilitation and leave a minor cosmetic defect.
However, if there are contraindications, laparotomy is resorted to. The Pfannenstiel incision is chosen - this is a transverse incision in the lower third of the anterior abdominal wall of the abdomen. The surgeon resorts to choosing a more traumatic approach if there are contraindications to laparoscopic surgery, such as severe adhesions, suspicion of malignant neoplasm of the ovaries and fallopian tubes, or grade 3-4 purity of the vaginal smear.
The operation is performed under general anesthesia. The patient falls asleep and wakes up in her room. Laparoscopic access is carried out using three trocars, which are inserted through small holes with a diameter of up to 1.5 cm. The first, with a video camera, is located in the umbilical region, and the other two with manipulators in the right and left iliac regions.
The assisting surgeon fills the abdominal cavity with gas in a volume of 2-3 liters. This stage is called pneumoperitoneum and is necessary to create conditions for the operation of optics, with the help of which the surgeon navigates inside the abdominal cavity. In most cases, carbon dioxide is used as the safest. In addition, by acting on the respiratory center, it increases the vital capacity of the lungs and, as a result, reduces the risk of secondary complications from the respiratory system.
At the beginning of the operation, the surgeon examines the pelvic cavity, finds the affected part of the organ and immobilizes it. Clamps are applied to the fallopian tube and blood vessels. Then the affected part of the uterus is excised, and a hemostatic suture is placed on the vessels, which will stop the bleeding. Since the fallopian tube is directly connected to the uterine cavity, the resulting hole is closed with a sheet of peritoneum. This process is called peritonization. In case of purulent inflammation of the fallopian tube, the abdominal cavity is thoroughly washed. Drainage is installed through the posterior vaginal fornix. At the end of the surgical intervention, the surgeon inspects the pelvic cavity, removes the trocars and sutures the small incisions that remain from them.
Possibility of getting pregnant after an ectopic pregnancy
The possibility of becoming pregnant after surgery to remove the fallopian tube with the fertilized egg is quite high, but still half as much as before it. Therefore, it is worth making every effort to thoroughly prepare for future conception, which will be most favorable if it occurs no earlier than two years after the ectopic pregnancy; during this period, the woman’s reproductive system is completely restored.
Following all the recommendations of your doctor and a healthy lifestyle will help you achieve the desired result!
ectopic pregnancy
With pipe removal
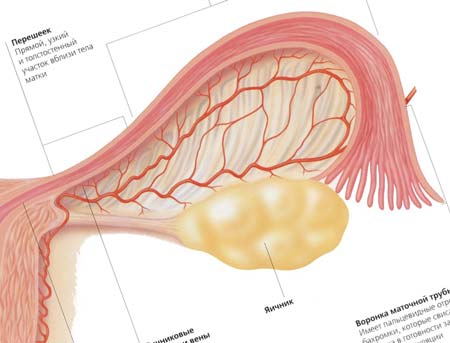
This is what the oviduct looks like
If there are significant changes in the oviduct, it is impossible to perform organ-preserving surgery. Factors that serve as indications for laparoscopy with elimination of the fallopian tube during ectopic pregnancy.
- Rupture of the wall of the oviduct, when damage to a large area is observed.
- Hyperemia and cyanosis of the tube during ectopic pregnancy with damage to almost all layers of the membrane.
- There is a danger of bleeding when performing coagulation of the attachment site of a fertilized zygote.
- Previous surgery on this tube with a similar diagnosis.