One of the diseases that occurs in women in labor (more often in primiparas) during breastfeeding against the background of infections is lactation mastitis. The disease is an inflammation of the breast tissue. Mastitis can be acute or chronic, manifesting itself in varying intensities.
Inflammation of the mammary glands can have different symptoms, including the intensity of symptoms. In some cases, mastitis can be confused with lactostasis. In order to avoid unpleasant consequences, it is necessary to contact a specialist in a timely manner.
Medical offers its services for the diagnosis and treatment of mastitis from highly qualified specialists. We use modern high-quality equipment for diagnostic examinations.
Causes of serous mastitis
In the serous form of mastitis, the parenchyma and milk ducts of the gland become inflamed. The infiltrate does not consist of pus, but of lymph and intercellular fluid.
Causes of the disease:
- Incorrect hygienic breast care during breastfeeding - rubbing the nipple, infrequent or too frequent wiping or washing of the breast.
- Installation of an artificial implant, compression with synthetic material, disruption of lymph outflow.
- Incorrect grip of the nipple during feeding: the baby pulls it without covering part of the areola with his mouth.
- Stagnation of milk and disruption of its normal outflow.
Stagnation of milk, or lactostasis, leads to impaired absorption and secretion of lactic acids. As soon as the serous fluid penetrates the breast tissue, the outflow of lymph becomes difficult and an infiltrate forms. The appearance of a serous infiltrate leads to inflammation of the gland tissue. If infectious microorganisms penetrate into the breast through damage in the form of cracked nipples, serous mastitis transitions into a purulent form.
Detoxification therapy
Infusion-transfusion therapy for mild metroendometritis is carried out in a volume of 1-1.5 liters per day for 5-7 days, for severe forms - in a volume of at least 2-2.5 liters per day for 7-10 days with the introduction solutions 2 times a day.
For mild cases
diseases are introduced:
- isotonic sodium chloride solution (0.9% 400 ml);
- glucose solution (5% 500 ml);
- ascorbic acid (5% 5 ml);
- vitamin B1 (5% 1 ml);
- calcium chloride solution (1% 200 ml);
- Trisol solution (400 ml).
In severe cases
metroendometritis is administered:
- isotonic solution (0.9% 400 ml);
- glucose solution (5% 500 ml);
- Acesol solution (400 ml);
- hemodez (400 ml);
- calcium chloride solution (1% 200 ml)
- ascorbic acid (5% 5 ml);
- vitamin B1 (5% 1 ml);
- aminophylline (2.4% 10 ml).
According to indications, blood plasma (200 ml), albumin (10% 100 ml) and blood transfusion are used.
Classification and symptoms of the disease
Types of serous mastitis according to the location of the infiltrate:
- Localized;
- Diffuse when it is distributed throughout the tissues of the entire gland.
Stages of development of the inflammatory process:
- Local stage - a small area of the chest is inflamed;
- Common stage - infiltrate occupies the entire gland.
The fact that serous inflammation has begun can be assumed by the child’s reaction during feeding. He is hungry because he does not eat enough due to the weak outflow of milk from the milk ducts compressed by the infiltrate. The baby's efforts to suck milk cause pain - the first sign of pathology.
Other symptoms of serous mastitis:
- Heaviness and engorgement in the chest;
- Pain and discomfort;
- Enlargement of the affected breast;
- Absence of fever, skin redness, and other systemic manifestations;
- Discharge of a few drops of clear liquid from the nipple;
- Difficulty expressing milk from the affected breast.
As the inflammatory process develops, milk stagnation increases and the breasts become even larger. With non-lactation serous mastitis, the first symptom is the discharge of a clear secretion from the nipple. The initial signs of serous mastitis are a reason to immediately consult a doctor.
Postpartum metroendometritis
Metroendometritis is the most common purulent-septic postpartum disease, which often occurs in a mild form, but can also have a severe course with the development of postpartum sepsis. Metroendometritis after cesarean section, as a rule, occurs in severe form, with severe intoxication and intestinal paresis. The disease is diagnosed based on the following data (Table 6):
- assessment of the general condition and severity of intoxication syndrome;
- results of examination of the postpartum mother (thermometry every 3 hours, measuring blood pressure at least 2 times a day, measuring daily or
Table 6
Complications of serous mastitis
The entry of pathogenic bacteria into the infiltrate causes an adequate response of the immune system - the formation of pus.
Complications:
- Formation of an abscess - an encapsulated collection of pus;
- The formation of phlegmon - diffuse inflammation of the glandular tissue of the breast,
- Dilation of the milk ducts, which subsequently prevents normal lactation and threatens suppuration.
Complications and consequences
One of the most insidious complications is the formation of a purulent infiltrate. In this case, not only ordinary mastitis, but also an abscess can develop. If there is no timely and effective treatment, the inflammation can develop into phlegmon of the chest, which is accompanied by the rapid destruction of the structural elements of the glandular tissue. In this case, only surgery will help.
An equally dangerous consequence of improper treatment can be the formation of multiple or single cysts, as well as galactoceles. Cysts quickly form and expand significantly due to the large accumulation of fluid in them. They can fester and interfere with breastfeeding of the baby.
Diagnostics
When visiting a doctor (surgeon, mammologist, gynecologist), a visual examination of the breast is performed. When pressing on the nipple, the doctor may detect clear discharge from it. The specialist collects anamnesis, finds out what complaints the patient has, and gets acquainted with the feeding habits.
General clinical tests to exclude other pathologies:
- General blood analysis;
- Analysis of urine;
- Blood sugar test.
An exceptionally informative diagnostic method is breast ultrasound. Ultrasound penetrates through all breast tissue, helps determine the location of the infiltrate, its features, size, and monitor the effectiveness of treatment.
It is important to differentiate serous mastitis from the purulent form of this disease. The purulent form of mastitis is characterized by increased temperature, general deterioration of the condition, and discharge of pus from the nipple. Manifestations of abscess mastitis can be detected by palpation, when fluctuation and softening of the middle of the infiltrate are noted.
Clinical and laboratory criteria for assessing the severity of metroendometritis
| Criteria for evaluation degree of severity | Severity | |
| light | heavy | |
| Risk factors for the development of purulent-septic diseases | May occur | The disease often develops against the background of complicated pregnancy and childbirth. |
| Emergence of clinical signs of disease | 5-12 days after birth | On the 2-3rd day after birth |
| The patient's condition | Satisfactory | Moderate or severe |
| Symptoms of general intoxication | Absent or weak expressed | Expressed |
| Body temperature | Low-grade fever, possible increase to 38.5 °C, without chills | 39 °C and above, with chills |
| Skin, visible mucous membranes | Regular color | Hyperemic or pale |
| Language | Clean, wet | Dry, with a white coating |
| Tachycardia | Within 90 beats/min | Severe, bradycardia may be observed |
| Tachypnea | No shortness of breath | Dyspnea |
| Stomach | Mild, usually painless | Soft, painful in the lower regions |
| Intestinal paresis | Absent | May occur after caesarean section |
| Uterus | An enlarged, painful uterus with unclear contours, soft or heterogeneous consistency is palpated, the size does not correspond to the day of the postpartum period (subinvolution) | |
| Lochia | Bloody or bloody, mixed with pus | Purulent, with an ichorous odor |
| Inspection using mirrors | Purulent discharge from the cervical canal; purulent plaque on the sutures of the vagina and cervix | |
| Vaginal examination | The cervical canal is passable for the finger beyond the area of the internal os. The uterus is enlarged, soft or heterogeneous in consistency, does not correspond to the rate of its involution after childbirth, is slightly painful on palpation; appendages are not defined, the arches are free | We pass the cervical canal for the finger beyond the area of the internal pharynx. The uterus is enlarged, soft or heterogeneous in consistency, does not correspond to the rate of its involution after childbirth, is sharply painful on palpation, the parametria are infiltrated, the uterine appendages may be enlarged and painful |
| Ultrasound data | The uterus has a heterogeneous echostructure, is usually enlarged, its cavity is expanded and contains hyperechoic inclusions throughout and fluid | |
| Dynamics of the disease during treatment | The mother's condition improves on the 2-3rd day | Symptoms disappear gradually over 5-7 days |
| Anemia | Mild degree | Severe degree |
| Leukocytosis | Up to 9.0-12.0-109/l | 14.0-30.0 109/l |
| Shift of the leukocyte formula to the left | Minor | Expressed |
| Toxic granularity of neutrophils | Absent | Occurs |
| ESR | Promoted | Sharply increased |
| Proteinogram | Total protein content is within normal limits or slightly reduced | Hypoproteinemia and dysproteinemia |
| Coagulogram | Tendency to hypercoagulability | Hypercoagulability, possibly decreased fibrinogen levels |
hourly diuresis, clinical and biochemical blood test, general urine test, bacteriological cultures of blood, urine, breast milk, contents of the cervical canal and nasopharynx, coagulogram, ultrasound of the abdominal organs, chest X-ray, ECG).
The main place in treatment
postpartum metroendometritis is treated with antibacterial and detoxification therapy; it should also include vitamins, antispasmodics, antihistamines, immunomodulators, antioxidants, drugs for correcting the hemostatic system and physiotherapeutic methods - local hypothermia, electrophoresis of magnesium sulfate or zinc sulfate (7-12 procedures). The duration of therapy depends on the severity of the disease and is 7-10 days for mild forms, and at least 14 days for severe forms.
Treatment of serous mastitis
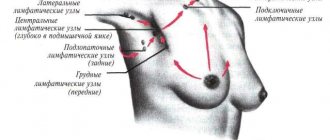
To normalize blood circulation and improve lymph circulation, it is important to restore normal milk flow. After the swelling subsides, the serous fluid will be absorbed spontaneously, and the disease will be cured. To improve your milk flow, it is important to continue breastfeeding or learn proper pumping techniques. To facilitate this process, perform a light and gentle massage from the top of the breast to the nipple. The next massage movement is carried out from the nipple to the armpits along the flow of lymph.
To improve blood circulation and relax the chest muscles, you can place a warm heating pad on the mammary gland.
It is not necessary to use medications to treat serous mastitis.
Medicines for symptomatic treatment:
- No-spa – relieves pain, improves milk flow;
- Malavit is a medicine created on a natural basis, used for compresses that relieve pain and itching, swelling and inflammation;
- Progestogel is a gel with progesterone in its composition, used to relieve swelling and reduce vascular permeability;
- Menovazin is an ointment for topical use, used to restore blood circulation and relieve swelling.
Vitamin complexes are used to restore immunity.
Physiotherapeutic methods are used in the treatment of serous mastitis:
- Electrophoresis with magnesia, Dimexide, Malavit;
- Infrasound;
- Magnetotherapy.
Proven folk methods are used as additional means. Among them are compresses made from honey cakes and cabbage leaves, alcohol compresses with aloe juice. It is important to remember about the dangers of alcohol for an infant and to wash off traces of such a compress from the breast.
Medicinal herbs are used as compresses, ingredients of ointments and healing infusions:
- Arnica – infusion relieves swelling, helps resolve infiltrate, improves blood circulation.
- Yarrow - compresses from brewed herbs or using an infusion internally helps relieve spasm of the milk ducts and normalize lactation.
- St. John's wort – compresses have an antispasmodic effect and improve blood flow from the source of inflammation.
Breastfeeding with mastitis
Mastitis in nursing women is quite common. Even though the pain may be too severe, you should not stop breastfeeding completely. The outflow of milk becomes difficult in the acute form of this disease. Constant stimulation of the nipple directly during feeding will help remove spasms and large amounts of accumulated milk. Without special indications, the child does not need to be transferred to artificial feeding.
If there is a need to administer medications to a woman or the inflammation passes from the serous stage to the purulent stage, then many doctors recommend stopping giving the baby breastfeeding for this time, and simply expressing until the gland is completely empty.
You should feed your baby not by the hour, but on demand. This will stimulate the production of certain hormones that promote good milk flow, and will also help the baby to latch onto the breast well.

Prevention
To prevent serous mastitis, it is enough to properly care for your breasts and rationally feed your child.
Basic preventive measures:
- Feed the baby on demand, without taking breaks of more than 3 hours between feedings;
- Carefully wash your breasts between feedings, do not rub them, and do not use aggressive detergents;
- Eat nutritiously and get enough sleep for adequate milk production.
Risk of disease complications

What complications can serous mastitis lead to and how dangerous is it? Experts emphasize that the first sign of worsening pathology is the formation of an abscess or the presence of pus in the inflamed area of the chest.
The complication of the disease is explained by:
- Penetration of pathogenic organisms into the structure of the mammary glands.
- Lack of timely therapy or its low effectiveness. In this case, there is a danger of a more serious complication – destruction of the glandular tissue of the breast by the inflammatory process. It is unacceptable to feed a child during such a clinic, as serious problems with his health and development may arise in the future.
- The formation of a galactocele (a typical benign formation) or a cyst in the structure of the mammary glands due to incorrect treatment.
- The development of cystic lumps occurs when the distal parts of the breast begin to enlarge and fill with fluid. This condition is a rather dangerous situation, since there is a risk of suppuration.
Forecast for the development of the disease
If treated in a timely manner, the prognosis for the development of serous mastitis is extremely favorable. A woman has many chances to finally recover. To prevent complications, it is important not to ignore the symptoms of serous mastitis, because complications develop very quickly. Pain, discomfort, and disturbances in the normal feeding of the baby should not be ignored and time should not be wasted for diagnosis and treatment.
Author of the article:
Lapikova Valentina Vladimirovna |
Gynecologist, reproductive specialist Education: Diploma in Obstetrics and Gynecology received from the Russian State Medical University of the Federal Agency for Health and Social Development (2010). In 2013, she completed her postgraduate studies at NIMU named after. N.I. Pirogova. Our authors
Prevention of pathology in young mothers
Following simple rules will allow you to establish physiological breastfeeding without the development of serous mastitis.
The breast and nipple must be prepared already at the stage of gestation. The glands are regularly rubbed with a hard towel, flat nipples are pulled out, and a massage is performed. When feeding, the mammary glands alternate; a long break between feedings of the baby should not be allowed. During hygiene procedures, a nursing mother should not rub the nipple area due to the risk of cracking. The bra should be as comfortable as possible. Often, when milk is secreted, breast size increases by 1-2 sizes. A nursing mother needs to purchase new, preferably special, underwear. For lactostasis, take a warm shower and express the gland until it is completely empty. A young mother should get enough sleep, spend time in the fresh air, eat well, take mineral and vitamin complexes, and protect her breasts from injury and hypothermia.
Read also:
Vitamins and nutrition for nursing mothers
Breastfeeding is a natural physiological process that allows you to provide all the nutritional needs of an infant for growth and development. Treatment of serous mastitis at the first signs will allow you to maintain lactation and protect the mammary gland from surgical intervention.
How to treat the inflammatory process without interrupting feeding
When a nursing mother encounters mastitis for the first time, it is difficult for her not to make mistakes. Some people panic and switch the baby to artificial formulas, some people, in a semi-fainting state, try alternative recipes that are applicable only at the very beginning of the disease, while others come to their senses and address their problem to an intelligent doctor. Yes, it is not easy to find such a specialist, but this is one of the first tasks that should be solved for the sake of your health and the health of your child.

Preventive measures
As you can see, serous mastitis can only be treated comprehensively, which greatly increases the chances of sustainable relief from the pathological condition.
To avoid the development of a painful condition, the following rules must be observed:
- You should not wash your breasts every time before and after feeding your baby. It is enough to wipe the nipples with a couple of drops of milk.
- During manipulation, you should not rub the nipples intensively, which is dangerous due to the appearance of cracks.
- If cracks occur on the nipple and areole, treat them promptly with an antiseptic and healing compounds (Bepanten, Solcoseryl, Purelan, sea buckthorn oil, etc.)
- A daily morning shower is enough to keep the glands clean.
- During feeding, it is important to ensure that the newborn latches onto the nipple and area around the nipple correctly.
- Avoid tight underwear with tight elastic bands.
Following these simple recommendations will help the young mother avoid the appearance of microcracks on the nipple, which can provoke serous mastitis.
Estimated forecast
With timely relief of the disease, the prognosis is always favorable. If the patient carefully follows all medical recommendations, she has a good chance of a full recovery.
An important point in successfully getting rid of serous inflammation is to seek medical help at its first symptoms, since this disease is characterized by rapid onset of complications.
If the process of breastfeeding becomes painful, the breasts become hard, or other symptoms begin to appear, you should immediately contact a gynecologist or mammologist.