Staphylococci are a group of bacteria consisting of 27 species, half of which have adapted to living on human skin and mucous membranes. But the ability to provoke the development of infection is inherent in only a few species that reproduce on tissues under certain conditions.
During breastfeeding, cracks in the nipples are a place for staphylococcus to enter the bloodstream. At the same time, milk infection in half of the cases is safe for the baby, but the situation requires mandatory therapy. The threat is determined by the type and concentration of the bacterium.
Signs of staphylococcal infection in mother and child
While the bacterium lives on the skin, it does not manifest itself in any way. Symptoms develop after staphylococcus enters the blood. Moreover, from the moment of infection until the appearance of characteristic signs of mastitis, 2-4 weeks pass. The taste of breast milk does not change, so the baby maintains a normal appetite during this period.
Symptoms of purulent mastitis in mother
- "Stone chest" effect.
- Elevated temperature: in the first stages – 37.0-37.5°C, upon transition to the purulent stage – 38.0-39.0°C.
- Weakness.
- Chills.
- Drawing pain in the chest, worsens with feeding.
- In 70% of cases, the lymph nodes in the armpits are enlarged.
Since breastfeeding continues, bacteria may enter the baby’s gastrointestinal tract, but the concentration of pathogenic microbes in the baby’s body in 83% of cases is insufficient for the development of the disease.
Symptoms appear at an advanced stage if the mother ignores purulent mastitis for a long time. The multiplication of pathogens in breast milk (from 1 thousand units/ml) at the peak of the disease causes damage to the baby’s organs.
Symptoms in a child
- Swelling of the eyelids.
- Purulent accumulations in the corners of the eyes.
- Crying 20-30 minutes after feeding.
- Peeling and inflammation of the skin.
- Rashes.
- Blistering formations - most often in the lower abdomen, on the back, in the folds of the neck.
These signs are characteristic of diseases caused by staphylococcus - conjunctivitis, phlegmon, pemphigus. The last, extremely dangerous manifestation, with delayed treatment, can be complicated by sepsis and the development of abscesses.
If the infection affects the infant's gastrointestinal tract, enterocolitis develops. Symptoms of the disease are vomiting, fever, loose stools with mucus. Mothers often confuse this condition with ordinary poisoning, prescribing medications (sorbents, antidiarrheals) to their child on their own. In this case, time is lost and the symptoms worsen.
Timely initiation of treatment for mastitis will eliminate the likelihood of complications in the baby. In the initial stages of the disease, the number of microbes in milk is 30-50 units/ml. Such concentrations are quickly destroyed by antibacterial therapy without the need to stop breastfeeding.
How the pathogen is transmitted from women to children
Staphylococcus can be found in mother's milk in different ways. It takes root in a cracked nipple or damaged areas of the skin, and enters a clogged milk canal. As a result, the baby and mother suffer, who may develop mastitis if Chlorophyllipt is not applied in time. Therefore, a woman must take care of her health.
The most common routes of infection to the mother are airborne and contact. The first is most likely while in the antenatal or postnatal ward. If the institution does not regularly treat wards with quartz and wet cleaning with a chloramine solution, pathogenic bacteria, including staphylococcus, multiply very quickly. You can become infected through contact during communication with infected people or through the use of shared hygiene items and things.
At the same time, the likelihood of a baby contracting staphylococcus increases if:
- premature baby;
- with low weight;
- there are congenital diseases;
- switched to additional nutrition when the mother’s milk supply was insufficient.

Staphylococcus can also be transmitted if the mother did not receive Chlorophyllipt in time and, as a carrier of the infection, infected the fetus in utero.
Where does staphylococcus come from in breast milk: reasons for its appearance

The bacterium lives and multiplies in the external environment. Due to the low sensitivity to external influences and the high rate of division, it is difficult to get rid of staphylococci in an infected room. Even with quartzization, the probability of survival of the “superbacterium” is 40-50%. But, if an infected object (tool, person) enters the treated room again, within 4-6 hours the concentration of staphylococcus becomes the same.
The No. 1 place of infection for a woman after childbirth is a medical hospital. This institution is considered the most dangerous in terms of the risk of infection with Staphylococcus aureus. Moreover, the hospital “superbug” has the strongest resistance to antibiotics and external influences.
Stages of infection
- Skin contact – household, airborne.
- Penetration into the wound surface and further into the blood.
- Infection of the gland.
- Penetration into milk.
- Development of infectious mastitis.
The bacteria enters the surface of the skin through tools, dust, household items, cutlery in common areas (treatment room, dining room, restroom). On the skin, microbes “wait” for the right moment to penetrate the body.
In the case of breastfeeding, staphylococcus enters the gland through the nipple fissures. The infection covers glandular tissue, milk ducts, and the bacterium is found in milk. As the pathogen multiplies, infectious mastitis develops.
To prevent infection, it is necessary to follow the rules for attaching the baby to the breast and skin hygiene.
Where does staphylococcus come from?
Staphylococci are bacteria that cause a wide variety of diseases. In small quantities they usually have no effect on the body. But under favorable conditions their concentration increases. As a result, consequences such as abdominal pain, digestive disorders, sore throat, otitis media, pneumonia and other diseases are possible.
Staphylococcus aureus is especially dangerous. The bacterium has a golden color, for which it was given its name. It is in a microcapsule, thanks to which it easily penetrates into tissues. In a certain environment, it produces toxic substances and enzymes that have a destructive effect on cells. Immunity to staphylococcus is not developed, so repeated infections cannot be ruled out in the future.
If staphylococcus is found in breast milk, this means that the woman is a carrier of the bacteria. She could have become infected in one of the following ways.
- Airborne. Often such infection occurs in hospitals, including maternity hospitals. It is quite difficult to fight bacteria brought from medical institutions, as they become resistant to antibiotics. To prevent their spread, these establishments must be properly sanitized.
- Contact. The pathogen can be found on common objects, on stair railings, on handrails in vehicles and in other places. Therefore, you should wash your hands with soap on time.

Breast milk tests for staphylococcus: delivery and interpretation
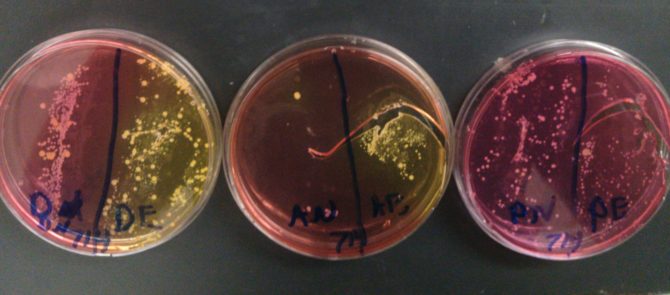
The presence of staphylococcus in breast milk is determined by laboratory analysis. The procedure for submitting milk for analysis requires proper preparation: a sterile, disposable container is used (sold in pharmacies), you will need 2 test tubes - one for each breast.
Preparation
- Breast treatment - wash with laundry soap and dry with a towel.
- Wipe the nipple with an alcohol wipe or hydrogen peroxide.
- Express 5-10 drops of milk into a separate bowl (the first portion is not suitable for analysis).
- The next 10-15 ml are collected in pharmacy tubes.
- Expression time is no more than 3 hours before the study.
- Label the test tubes “1” and “2” (or “left” and “right”).
The result takes 5-7 days to prepare.
The form with the analysis result has two columns - the norm and the result, which should have minimal differences. But the presence of pathogenic flora in milk is not a reason to panic, since the threat is determined by the growth rate of colonies.
Decoding indicators
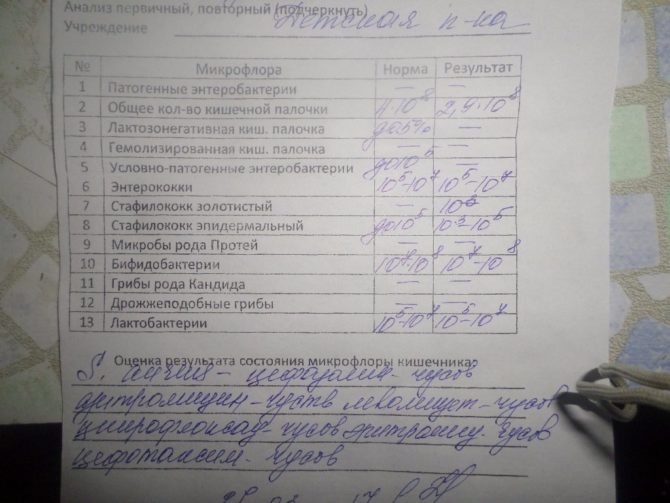
The result of the state of the intestinal microflora
- Grade 1 – weak growth of staphylococcus colonies.
- Grade 2 – growth of up to 10 colonies.
- Grade 3 – 10-100 colonies.
- Stage 4 – multiplies >100 colonies.
The higher the degree, the more actively the infection process develops. First, second degree - there is a bacteria, but there is no disease; third - pathology develops; the fourth is a disease at a dangerous stage of complications.
The decision to continue breastfeeding is made based on the result of the milk analysis.
For whom is staphylococcus dangerous?
Microorganisms present in breast milk first enter the baby’s mouth and then into his gastrointestinal tract, but pathological conditions do not always arise. Mother's milk, being a rich source of vitamins, among other things, supplies the child with important antibodies that successfully fight microbes, including staphylococcus. Therefore, most children's bodies do not react in any way to the presence of these microbes. They can cause disease in the following children:
- premature;
- born with pathologies;
- very weak, low weight;
- receiving complementary foods from the first days of life.

Is it possible to breastfeed if you have staphylococcus?

In half of the cases, breastfeeding does not stop. At minimal concentrations in milk, staphylococcus is safe for the baby. Stopping breastfeeding is recommended if a diagnosis of purulent mastitis is made or if pathogens are detected in the child’s stool. In this case, antibiotic therapy is prescribed, which is often incompatible with hepatitis B.
If the results are higher than the third degree (the probability of developing a purulent process is 80%), the risk of infection of the child increases, so switching to artificial nutrition is preferable.
If the infection does not cause purulent inflammation in the mother, then it is better to continue breastfeeding. The explanation is the immunomodulatory effect of milk on the child’s body, protection against the penetration of pathogens.
Arguments for"
- Possibility of using herbal antimicrobial drugs compatible with hepatitis B.
- Production of safe antibacterial drugs.
To eliminate the risk of infection of a child, precautions must be taken. Prevention of transmission of bacteria to the baby will allow combining therapy with breastfeeding.
Precautionary measures
- Treatment of nipple cracks with hydrogen peroxide (morning, evening).
- Using nipple shields.
- To wash the glands, use moisturizing soap (to avoid drying and cracking of the skin).
- Correctly position the baby when feeding (the baby's mouth is open wide, the lower lip is turned out, the chin is pressed to the chest).
Prevention of complications and treatment of infection will prevent infection of the child and restore the normal composition of milk in 7-14 days. In 70% of cases, treatment is accomplished without antibacterial drugs.
Rules for collecting analysis for bacteriological culture
If the baby is capricious, sleeps poorly, regurgitates frequently, and the stool differs from what it should be, then it is necessary to have your breast milk tested for staphylococcus. This will require some care, but overall the procedure is not too complicated.
- Prepare 2 sterile test tubes or jars with lids; you can purchase them at a pharmacy or use containers available at home.

- Wash 2 small jars, boil them for at least 15 minutes, wipe the tight lids with moistened soda, rinse and immerse in boiling water for 1 minute.
- Wash your hands, breasts, nipples and areolas with baby soap, wipe everything with sterile wipes, you can use Chlorophyllipt for lubrication.
- Label the dishes, since the milk from each breast is expressed into a separate jar.
- The first 10 ml of milk should be expressed into the sink to prevent the entry of bacteria that could remain after rinsing the nipples.
- The second portion of 10-20 ml is expressed into jars, which must be closed immediately.
- After this, the tests are submitted to the laboratory for bacteriological culture within 3 hours.
The results of the test for staphylococcus, obtained after 5–7 days, are transferred from the laboratory to the pediatrician. Only he can decide on the need for treatment and which drugs are best to use.
How to get rid of staphylococcus in breast milk

It is difficult to destroy staphylococcus, since the microbe is extremely resistant to antibiotics. For example, Penicillin was initially an effective antimicrobial drug. But today's staphylococcus is no longer sensitive to the product.
The most dangerous bacteria, difficult to respond to antibiotics, live in hospitals. Pathogens adapt to survive under conditions of strict sanitary control, and therefore are resistant even to modern drugs. To determine treatment tactics, resistance studies are carried out, on the basis of which the doctor prescribes certain drugs.