/About children/Breastfeeding and artificial feeding. Complementary feeding/HB problems
Breast problems, unfortunately, are familiar to many nursing mothers.
And, probably, each of them, encountering this for the first time, felt confused: what to do? Run to the doctor? Make a compress? Should I breastfeed my baby or not? We will try to help you understand exactly what ailments occur during breastfeeding and how to act in these cases.
Very often, nursing mothers call mastitis lactostasis .
Associated symptoms

The appearance of burning and redness around the areola indicates serious pathologies
An unpleasant feeling in the chest occurs equally during the night and daytime hours of breastfeeding. In addition to burning and tingling, other signs may appear:
- soreness and lumps on the side of the mammary glands;
- hyperthermia is sometimes possible;
- itching and redness appear around the areola;
- Possible scanty discharge that does not resemble milk.
Such manifestations occur if women have serious problems with women's health. If the burning sensation is physiological in nature, it is short-lived. It is associated with an active rush of blood to the nipples along with the arrival of milk and an increase in the milk ducts.
True mastitis
Mastitis is an infected inflammation of the breast tissue . Most often it develops against the background of engorgement or lactostasis. If milk is not removed in a timely manner during lactostasis, inflammatory changes in the breast tissue begin, occurring against the background of swelling and changes in blood circulation in the lobe of the gland with lactostasis. This condition is often called uninfected mastitis.
If a woman has abrasions or cracks in her nipples, the inflammatory focus quickly becomes infected. It should be noted that the infection can get there not only from cracks, but also from any other source of chronic infection in a woman’s body (for example: a carious tooth, chronic tonsillitis, pyelonephritis, etc.) There are often cases when, with a common sore throat, a cold, , with the flu, a woman suddenly develops pain on the 2-3rd day, sharp tingling pains, even redness on the chest without prior formation of lumps in this place. These are all signs of infected mastitis.
With any mastitis, your health worsens, your overall body temperature rises, part of the breast becomes red and hot, painful when touched.

Treatment of mastitis is carried out according to the same principles as the treatment of lactostasis. It is necessary to free the lobe from milk by pumping, massage and latching on the baby.
“With mastitis, feeding a child is not prohibited, but necessary, since no one better than a baby can empty the lobes of the mammary gland.
The infection that caused the inflammation reached the child several days before the mother showed the first visible signs of this infection. Now he already receives with milk not only pathogenic organisms, but also active immune protection against this infection. As a rule, when such a child is weaned from the breast, he gets sick 2 times more often than when breastfeeding continues.
To speed up the process in this case, expressing with a suitable breast pump and using warming and absorbable compresses are used. Any compresses prescribed by your doctor will do, except alcohol or vodka. Alcohol is an antagonist of oxytocin, a hormone that stimulates milk flow. When using alcohol-containing compresses on the breast, it is well absorbed and disrupts the outflow of milk from the affected lobule. Regular use of alcohol compresses can easily “curtail” lactation completely.
For infected mastitis, antibiotic therapy is necessary. There are a large number of modern antibiotics that are compatible with breastfeeding.
» If a doctor prescribes antibiotics, you must inform him about this, because very often doctors do not consider it necessary to continue breastfeeding during antibiotic therapy and do not bother choosing a treatment that is compatible with breastfeeding.
As a rule, you need to regularly take the medications prescribed by your doctor for at least 5 days and take care to “save” your intestinal flora during the period of antibiotic treatment. Now there are many combination drugs that are prescribed simultaneously with antibiotics. If your doctor has not prescribed anything similar, consult your pharmacist.
Causes of burning in the chest during feeding

Painful sensations may occur as a result of damage to the nipple
First of all, a burning sensation in the chest during lactation occurs under the influence of physiological factors. Such conditions are often favorable and do not require special treatment if they are not associated with an inflammatory process.
- Large quantities of milk. In the first days after the birth of a child, a woman begins to produce the hormone prolactin. As a result, milk arrives in the breast. It swells, burning and tingling appears. In this condition, it is necessary to carry out regular pumping to avoid stagnation. The production process will improve at the moment when the child can eat normally. For this purpose, you need to observe regular application.
- Damage to the nipples. Soreness appears if there are injured areas on the skin around the nipples. These could be child bites or cracks. Small ulcers often appear due to improper attachment of the baby to the breast. Usually, pain syndrome appears immediately at the time of feeding, when the baby begins to bite painful places with his gums.
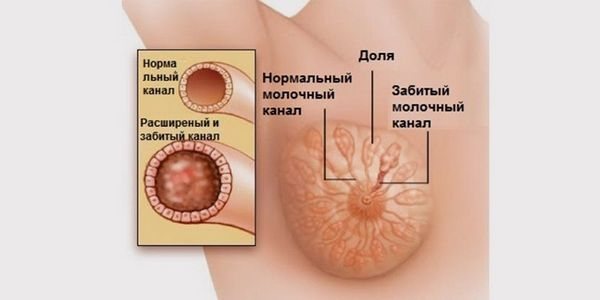
Lactostasis causes blockage of the milk ducts - Lactostasis. This condition is accompanied by inflammation in the mammary tubules of the mammary glands. Along with the burning sensation, redness may appear. The cause of this problem is improper attachment and incomplete emptying of the breast by the child.
- Mastitis. Accompanied by elevated temperature. Greenish or yellow discharge from the nipples may appear. This indicates the presence of pus in the mammary glands. It is caused by improper breastfeeding and the penetration of Staphylococcus aureus into the breast through wounds and cracks in the nipples.
If the condition is pathological, the pain does not go away for a long time even after finishing feeding. In this case, one may suspect the progression of a fungal infection that penetrates the open milk ducts. Also, with such symptoms, malignant neoplasms are often diagnosed.
If a deep burning sensation appears in the chest of a nursing mother, it is necessary to urgently seek advice from a mammologist. Perhaps the process is benign, and the disease can still be cured.
What other factors may influence

A tight bra can cause discomfort and pain.
There are several more banal factors that can affect the appearance of discomfort in the chest area.
- Wearing a tight synthetic bra. When the glands filled with milk are compressed, the milk ducts narrow. This causes tingling. In the future, poor milk yield during feeding is possible.
- Eating hot food. If you eat this way constantly, you will produce an increased amount of milk. This causes a feeling of warmth and burning in the chest.
- Menstruation after childbirth. They usually appear after 9-10 months of established lactation. Accompanied by a burning sensation in the areola and lateral parts of the mammary glands.
Similar sensations may occur at the time of weaning from breastfeeding. Especially if there is a pronounced lack of milk, the baby tries to actively suckle at the breast, as a result of which the mother experiences pain and irritation.
What is lactostasis?
This is a painful lumpiness of the breast, and often redness of the skin over the lump. The occurrence of such lumpiness or compaction is associated with blockage of one of the ducts, presumably a fat droplet, and a violation of the outflow of milk from the gland lobe.
If lactostasis is accompanied by an increase in body temperature, chills, and deterioration in general health, then American authors prefer to call it uninfected mastitis
(as opposed to
infected
or
serous
mastitis, the signs of which are described below). Therefore, there is confusion both in the literature and among nursing mothers - you can say “mastitis” and mean completely different things.
» The main cause of lactostasis is poor drainage of the entire breast or part of it.
Poor drainage is most often associated with the baby feeding in the same position. For example, in a standard “sitting” position, the axillary lobe, the largest and with convoluted ducts, is emptied the worst of all (the areas closest to the child’s lower jaw are emptied best - in this case, the infero-central ones, and the superolateral ones - the worst).
The simplest action to prevent stagnation of milk in the axillary lobes is to sometimes put the baby “from under the arm” - the mother, for example, sits (you can also lie down), the baby lies on a pillow with his head at the chest, and the bottom and legs are behind the mother’s back, The baby lies on his side, under his arm. Very often, when congestion occurs under the arm, it is enough to place the child in this position several times in a row and he will suck everything out perfectly.
The location of lactostasis on top “in the center” is typical for those cases when the mother holds the breast with “scissors” during feeding.
– nipple between the index and middle fingers, the index finger pressed into the chest.
This way, the breasts cannot be supported or fed - but in most maternity hospitals this is how they advise giving breasts; in some courses on preparation for childbirth they literally advise the following: “Hold your breasts like a cigarette.”
“The chest must be supported with the whole hand – the thumb on top, the rest under the chest. In the vast majority of cases, the breast does not need to be supported throughout the entire feeding - it must be held by the child himself.
Very often there are recommendations to constantly wear a bra so that it supports the breasts higher, and then they would fill evenly both above and below, they even suggest sleeping in a bra. All this is called the prevention of lactostasis. But by nature, a woman’s breasts are designed in such a way that more milk accumulates in the lower lobes, and from any position it is the lower lobes of the gland that are best emptied. So why do we need to achieve uniform accumulation of milk in all lobes of the gland? Probably, so that it would be more convenient for lactostasis to form up there... If a bra is worn, it should be loose. It is convenient when milk leaks and you need to use pads...
“If a woman has large and heavy breasts, one of the reasons for the formation of lactostasis is sleeping at night in an uncomfortable position.
Try to sleep more often on your stomach with a comfortable pillow - then during strong hot flashes, the milk will simply flow out and not stagnate.
Lactostasis is much less common with properly organized breastfeeding, when there is no accumulation of large portions of milk for feeding, and the mother knows how to feed the baby from different positions.
However, lactostasis is a mysterious thing, sometimes it occurs out of nowhere and with active sucking on the affected breast it goes away within 1-2 days without special measures. (And the mother begins to say that it was the cabbage leaf that helped her. If you come across a mother who does not understand at all what is happening to her, and when she begins to develop lactostasis, she stops putting the baby to the sore breast and stops touching it altogether, she no cabbage leaf helps. Then disaster usually happens.)
“The tendency to form lactostasis in women is usually the same and does not go away with age and the birth of other children.
If a woman with her first child did not have lactostasis, and at the same time she followed all the rules of feeding - she fed for a long time, without restrictions at the request of the child, without supplements and supplements, and lactation persisted for at least a year - this means that the likelihood of

She has little lactostasis when feeding subsequent children. If, under the same conditions, there were lactostases when feeding the first child, then perhaps they will be regularly repeated at the same time when feeding subsequent children, and, as a rule, the mother herself learns to treat them calmly and cope quickly and don't turn it into a problem.
It is impossible to say anything similar about a woman who does not follow the feeding rules, because she does not have the most important weapon in the fight against lactostasis - the self-regulating mother-child system. There are often cases when a mother who fed her first child regularly suffered from lactostasis, and when feeding her second and subsequent children she fed freely and was surprised to note that she did not have any lactostasis.
“If lactostasis appears in the breast, you need to put the baby on it as often as possible.
Sometimes it is necessary to express the breast before feeding and attach a baby who actively wants to suckle to the breast, in which only lactostasis remains. Sometimes it is necessary to preheat and massage the segment with lactostasis and express it. The easiest way to warm up, which a mother can safely use, is to place a hot, wet napkin (towel) on the affected segment 5-10 minutes before pumping (or a warm shower).
The severity of the situation does not depend on the degree of soreness or redness of the breast, but on the woman’s ability to express with such soreness. It is pain that prevents the mother from pumping effectively. Therefore, it is better to seek the help of a specialist who can cope with this complication in 30 minutes. Most mothers are afraid to express and massage this area because they think something might burst there. “Something can burst” only if you carry out massage and pumping as follows: put your breasts on a stone and hit it with a hammer on top.
“Lactostasis in itself is not a dangerous thing; illiterate actions to overcome it are dangerous.
You cannot stop feeding the affected breast, even if you have a very high fever! You can’t leave a painful lump unattended during the night break!
Examination methods
Palpation of the mammary glands is one of the methods for diagnosing the disease
At home, a woman needs to independently determine the condition and size of her breasts. To do this, stand in front of a mirror and evaluate whether there is asymmetry. If the volume of the mammary glands differs, it is necessary to seek an in-person consultation with a doctor. In the future, the following types of diagnostics are prescribed.
- professional palpation;
- MRI (magnetic resonance imaging);
- mammography;
- laboratory tests for female hormones.
Based on the test results, an accurate diagnosis is established and the danger of the pathology to health and life is assessed.











