Rules for taking painkillers
When using an anesthetic while breastfeeding, you must follow these rules:
- Take the analgesic in the minimum therapeutic effective dosage. You should not reduce the dose in the hope that less of it will pass into breast milk. The painkiller may not show its therapeutic effect, but it will still have an undesirable effect on the child;
- You should not take the medication in a “shock” dose, of course, unless it is prescribed by a doctor. When a large amount of medication is taken, the likelihood of side effects increases;
- It is better to take the medicine immediately after the child has eaten. Then the body will be able to remove it from the body by the next feeding;
- Do not take analgesics with alcoholic drinks, as in this case they enhance the toxic effect of each other;
- Use medications only if other methods do not help cope with pain, such as proper sleep, massage, traditional medicine recipes;
- Take the medication once; in case of chronic pain, it is recommended to consult a doctor to find out the cause of its occurrence;
- Without consulting a specialist, painkillers during breastfeeding should not be taken for more than 3 days in a row;
- The medication should be stopped if the woman or child experiences undesirable reactions.
Requirements for taking painkillers, prohibited drugs
The question of whether a young mother can take painkillers is difficult to answer unequivocally. Experts recommend that women who are breastfeeding should refrain from taking medications if possible. If the pain does not cause the fairer sex any noticeable discomfort, it is advisable to endure it or try to eliminate it using safe traditional medicine. You should resort to medication only when the pain is severe and causes significant suffering to the nursing mother.
Every woman who breastfeeds her child needs to remember the list of drugs that are strictly prohibited during lactation. These medications include:
- Analgin and other drugs based on sodium metamizole (Pentalgin, Sedalgin, Tempalgin, Tetralgin, Revalgin);
- Preparations containing acetylsalicylic acid (Aspirin, Copacil, Askofen, Farmadol, Migralgin, Citramon).
The listed medications are strictly prohibited during lactation, since their active components penetrate into breast milk, provoking allergic reactions in the baby and having a negative effect on its internal organs.

Nursing mothers are strictly prohibited from taking Analgin and Citramon.
Painkillers during breastfeeding should be safe for the baby. When choosing them, preference should be given to those medications that are quickly eliminated from the mother’s body and allow you to obtain the maximum therapeutic effect in a short time. Before using any medication for pain, a woman needs to make sure that she has no contraindications to it. If a representative of the fairer sex took a painkiller approved for lactation before pregnancy, and it caused a hypersensitivity reaction in her, she should refrain from taking it after childbirth, otherwise she risks harming herself and her baby.
Consequences of using painkillers during lactation
Most medications are prohibited for women who are breastfeeding, since their active substances are secreted through the mammary glands and enter the baby’s digestive tract.
They can cause significant harm to his health, cause allergies, dyspeptic disorders, dysfunction of the central nervous system and blood picture, and provoke poisoning.
But even if the medication does not have a negative effect on the child’s development, it can cause a number of other undesirable reactions:
- sleep disorder;
- lethargy;
- moodiness;
- lethargy;
- refusal to eat.

But this does not mean that you need to endure pain, you just need to know what nursing mothers can take.
If you still need to take painkillers - rules
Of course, there are cases when pain relief is needed urgently, but it is impossible to get to a doctor. For example, a nursing mother had a toothache at night. In this case, from the list of approved painkillers, the drug that contains the least amount of toxic substances is selected. Toxins immediately penetrate into breast milk, and the child’s body has not yet learned to eliminate all toxic substances. If the mother is in pain during the day, she needs to see the pediatrician in her area and get advice on what medicine and in what quantity she can take.

Before taking medications, you should consult your doctor
After taking painkillers and feeding the baby, the mother should constantly monitor the condition of the baby. If he develops increased drowsiness, lethargy, apathy, lack of appetite, and especially nausea with vomiting, he should immediately call an ambulance.
In the case when the drug is taken as a course, it is necessary to exclude breastfeeding at the very peak of activity of the active substances. If a nursing mother is prescribed a medicine that is incompatible with lactation, she should stop breastfeeding and resume it after treatment. Under no circumstances should you reduce the dose of the drug in order to continue feeding your baby milk. This is dangerous for his health, development, and sometimes life.
Pediatricians strongly recommend that when taking painkillers for a long time, you constantly express milk so that the active substances do not enter the baby’s body.
If the pain is temporary and does not occur often, it is quite acceptable for a woman to take an approved painkiller while breastfeeding. When the pain does not stop, occurs regularly, and causes severe discomfort, this signals that the woman needs to undergo an examination to identify the true causes of the pain.
How to choose a medicine
When choosing a medication, you must follow the following recommendations:
- Give preference to single-drug medications, since the more active components (substances) a medicine contains, the more contraindications it has and the higher the likelihood of developing unwanted reactions. This is why do not take several medications at the same time;
- You should not use long-acting medications, as they take a long time to be eliminated from the body. It is better to use products with a short half-life;
- Choose dosage forms that release the active substance more quickly, such as rectal suppositories or dissolvable tablets;
- If it is possible to relieve pain with ointments and other means for external use, then give preference to them;
- Pay attention to contraindications and unwanted reactions that it may provoke.

Contraindications and possible side effects
Before using any medicine, it is recommended to carefully study the prohibitions on use. Most products have one general contraindication - the individual sensitivity of the body to the active components. In such cases, the use of tablets or suppositories is strictly prohibited. In case of chronic severe diseases at the peak of exacerbations, it is also better to stop using painkillers.
If you neglect the prohibitions, the following complications are possible:
- nausea;
- vomit;
- stool disorders;
- dizziness;
- prolonged headaches;
- discomfort in the digestive organs;
- irritation of the dermis.
If even one signal appears, it is recommended to immediately stop treatment with painkillers and consult a specialist.
Methods of using painkillers
Painkillers can be taken orally, applied topically or rectally.
Pills
Painkiller tablets are effervescent and coated. If possible, it is better to give preference to soluble drugs, as they begin to act faster.
Women who support breastfeeding are allowed Ibuprofen, Panadol and Efferalgan, which are available in effervescent tablets.
Pain relieving ointments
Ointments and other external dosage forms are practically not absorbed into the bloodstream, and, therefore, do not cause systemic adverse reactions. In this case, excretion through the mammary glands occurs in a minimal amount.
But, unfortunately, the range of applications of these drugs is narrower compared to tablets. They help only with pain arising from pathologies of the musculoskeletal system and soft tissue injuries. You also need to know what pain-relieving ointments can be used, because many of them are still prohibited for breastfeeding women.
It is acceptable to use Voltaren Emulgel, Nurofen Express gel.
Candles
Analgesic suppositories have the same spectrum of action as analgesic medications in tablets. Moreover, they can be used when oral administration is contraindicated or ineffective, for example due to vomiting.
Another advantage of suppositories is the rapid onset of therapeutic action.
The downside is that they are absorbed into the bloodstream and cause systemic side effects.
There are pain-relieving suppositories on sale for the treatment of hemorrhoids: Relief Advance, Procto-Glivenol.

What will help with stomach pain
No-Spa will help relieve stomach pain; this drug is also effective in cases of renal, hepatic and intestinal colic, inflammation of the bladder (cystitis), and bloating after surgery. The tablets relieve headaches caused by vasospasm. During lactation, you can take one or two at a time, but only 4 pieces are allowed per day. The duration of use should not exceed 7 days.
For abdominal pain due to intestinal discomfort (flatulence, bloating, rumbling), in addition to No-shpa, you can use an infusion of dill seeds in the form of tea (a teaspoon per 300 ml of boiling water), it simultaneously stimulates the secretion of breast milk, relieves colic in baby. It is beneficial to drink herbal tea with chamomile and mint.
Watch the video about dill seed recipes:
Allowed means
Paracetamol
Medicines based on paracetamol are drugs for relieving pain during lactation, which is observed in the following pathologies:
- Neuralgia;
- Dysmenorrhea;
- Joint, muscle, toothache;
- Cephalgia.
They are produced under different trade names:
- Paracetamol;
- Panadol;
- Efferalgan.
Preparations containing paracetamol should not be used if you are intolerant to their composition!

They should be used with caution if a woman has the following pathologies:
- Impaired kidney and liver function;
- Alcohol addiction;
- Glucose-6-Phosphate Dehydrogenase (G6PD) deficiency;
- Damage to baking with ethyl alcohol;
- Viral hepatitis;
- Increased levels of bilirubin in the blood due to pigmentary hepatosis.
Medicines in this group can cause the following adverse reactions:
- Nausea, vomiting, abdominal pain;
- Allergy, manifested by rash, itching, urticaria, angioedema;
- Decrease in the level of all blood elements.
You should not take several paracetamol-containing medications at the same time, as this may cause paracetamol poisoning.
If paracetamol drugs are taken for more than 5 days, then it is necessary to monitor the peripheral blood picture and liver function.
Ibuprofen
Ibuprofen (Mig, Nurofen) belongs to the group of non-steroidal anti-inflammatory drugs. The medicine is sold in the form of tablets, including effervescent tablets, capsules and gel. The drug is excreted in small quantities in breast milk, but it can be taken once during lactation.

When taking a daily dosage of more than 800 mg or for a long time, the baby must be switched to formula.
The analgesic can be taken orally to relieve moderate pain of various origins:
- Pain after injury or surgery;
- Dysmenorrhea;
- Cephalgia and migraine;
- Neuralgia;
- Muscle and toothache.
Ibuprofen-based gels can be used for pain arising from pathologies of the locomotor system:
- Rheumatism;
- Attack of gout;
- Muscle pain;
- Ankylosing spondylitis;
- Inflammation of the tendon-ligamentous apparatus;
- Injuries to soft tissues, without compromising the integrity of the skin;
- Lumbodynia;
- Pinched sciatic nerve;
- Radiculopathy;
- Osteochondrosis;
- Periarthritis;
- Arthrosis.
Regardless of the form of release, an anesthetic should not be used if a woman has an intolerance to the composition of the medication and other NSAIDs, which include aspirin.
You should not take an analgesic orally if you have the following pathologies:
- Exacerbation of erosive and ulcerative diseases of the gastrointestinal tract;
- Colitis;
- Problems with blood clotting;
- Brain hemorrhage;
- Bleeding from the digestive tract;
- Severe dysfunction of the liver and kidneys;
- Previous coronary artery bypass surgery.
It should be taken with caution if you have the following diseases:
- Heart failure;
- High pressure;
- IHD;
- Cerebrovascular accident;
- Increased levels of lipids and bilirubin in the body;
- Diabetes;
- Pathologies of the arteries of the extremities;
- Nicotine and alcohol addiction;
- Cirrhosis;
- History of gastrointestinal ulcer;
- Blood pathologies of unknown origin;
- Disease of the liver and kidneys, in which the glomerular filtration rate is less than 60 ml per minute.
The gel should not be used if the integrity of the skin is damaged, eczema, or weeping dermatitis.
It should be used with caution in the presence of the following pathologies:
- Exacerbation of hepatic porphyria;
- Gastrointestinal ulcer;
- Severe pathologies of the liver and kidneys.
The following side effects may occur when taking Ibuprofen orally:
- Abdominal pain, nausea, vomiting, heartburn, lack of appetite, loose stools or retention, bloating, ulcerations of the digestive tract mucosa, which can cause organ rupture and bleeding;
- Irritation, pain and dry mouth, stomatitis, inflammation of the pancreas and liver;
- Dyspnea, bronchospasm;
- Hearing loss, ringing in the ears;
- Weakened vision, diplopia, scotoma, swelling of the mucous membrane of the eyes and eyelids;
- Headache, vertigo, sleep and consciousness disturbances, depressed mood, hallucinations, inflammation of the meninges, anxiety, irritability;
- Hypertension, heart failure, increased heart rate;
- Impaired kidney function, increased daily diuresis, inflammation of the bladder;
- Allergy;
- Decrease in hemoglobin, leukocytes and platelets;
- Increased sweating;
- Increased bleeding time;
- Hypoglycemia;
- Increased creatinine levels and liver enzyme activity.
Ibuprofen-based gel can cause allergies, dyspepsia, abdominal pain, and bronchial asthma.
If used for a long time, it can provoke systemic adverse reactions.
What painkillers are used in the maternity hospital after cesarean section: which ones to take and which ones to inject?
In the first 2-3 days in the maternity hospital after a cesarean section, fairly strong drugs are injected, but with a low risk for nursing mothers; they can then be taken in tablets or administered in suppositories: Ketoprofen, Ketorolac, Diclofenac.
Ketoprofen
Preparations with ketoprofen in injections (Ketonal, Flamadex, Ketoprofen, Artrosilene) are administered intravenously or intramuscularly, 1-2 ampoules per day; instead of the second injection, you can put a suppository at night. Relieves pain for 6-8 hours and also has an anti-inflammatory effect. Contraindicated for peptic ulcers, heavy bleeding, severe liver and kidney diseases.
Artrosilene Ketonal Flamadex Ketoprofen
Ketorolac
Injections of drugs with ketorolac (Ketorol, Ketanov, Dolak) are stronger than Ketonal, but their anti-inflammatory effect is less pronounced. Intramuscular injection is carried out slowly, as deep as possible into the muscle. Relieves pain in 15-25 minutes, the maximum effect appears at the end of the first hour and lasts for at least 6 hours.
Ketorol Ketanov Dolak Ketorolac
Ketorolac is used only for unbearable pain, as it can depress the nervous system of the mother and child. Contraindicated in diseases of the digestive system (exacerbation of ulcers, gastritis), renal, liver failure, severe heart disease, hypertension.
Diclofenac
When Diclofenac is administered (synonyms: Voltaren, Diclonate), the analgesic effect occurs quickly (after 8-15 minutes). It is prescribed for moderate to severe postoperative pain and lasts 6-8 hours. You can make 2 injections per day or use one injection and one suppository.
Diclonate Voltaren
You cannot inject the drug for more than 3 days; if necessary, the woman in labor is switched to tablets or suppositories. The use of the drug for gastrointestinal bleeding, peptic ulcers, and circulatory disorders is prohibited.
How many days do you take pain relief?
Usually, after a caesarean section, pain relief is required in the first 3 days with injections, then you can switch to suppositories, and tablets for oral administration are less commonly prescribed. As soon as the pain becomes tolerable, the dose is reduced. Most often, by the end of the first week (before discharge), the need for pain relief medications is minimal or not required at all.
If necessary, in the first 1-2 weeks it is best to use suppositories (Ketonal, Diclofenac), they are easy to administer independently, they are less harmful to the gastric mucosa.
Diclofenac suppositories
The main condition is to use the minimum effective dose and the shortest course, then they do not have a harmful effect on the mother and child. All medications are prescribed only by a gynecologist.
Prohibited means

Analgin
Analgin and its analogues, such as Baralgin, Bral, Spazmalgon, Maksigan cannot be used for breastfeeding, since their constituent metamizole sodium is excreted in the form of metabolites in breast milk.
Read more about taking Analgin during breastfeeding here
Nimesulide
Nimesulide belongs to the group of NSAIDs (non-steroidal anti-inflammatory drugs). The medication relieves pain and inflammation, lowers body temperature, but it is contraindicated for nursing mothers. The following drugs are complete analogues of Nimesulide:
- Nimulid;
- Nise;
- Nimesil.
Ketanov
Ketanov contains ketorolac as an active component. It is contraindicated during pregnancy, childbirth and lactation, as well as in patients under 16 years of age. The drug is available in injections and tablets.
The drug passes into breast milk. After oral administration, the maximum concentration in the blood is observed after 2 hours. The following drugs are complete analogues of Ketanov:
- Ketorol;
- Dolak;
- Ketorolac;
- Ketalgin.
Diclofenac
Diclofenac belongs to the group of NSAIDs. The drug has an antipyretic and analgesic effect, stops the inflammatory process. The medicine is produced by several domestic and foreign companies in tablets, injections, gel, ointment, rectal suppositories, eye drops. When taking the medication orally, or injected into a muscle or anus, Diclofenac passes into breast milk. Therefore, it is contraindicated in tablets, suppositories and injections.
There is no data on whether it is secreted through the mammary glands when used in the form of a gel or ointment, so it is not advisable for them to be used by a nursing mother without a doctor’s recommendation.
When it is necessary to use a painkiller, the gel or ointment should not be applied to the mammary glands, to an open wound, or used for a long time.
Diclofenac gel and ointment should not be applied if you are intolerant to their composition and other NSAIDs. They should be used with caution if a woman has the following pathologies:
- Exacerbation of hepatic porphyria;
- Gastrointestinal ulcer;
- Bronchial asthma;
- Severe liver and kidney diseases;
- Problems with blood clotting;
- Chronic heart failure.
Diclofenac in the form of gel and ointment is allowed to be used during feeding, but consultation with the attending physician is required, since the drug can cause the following adverse reactions:
- Urticaria, Quincke's edema, rash;
- Bronchial asthma;
- Eczema, dermatitis, erythema, photosensitivity;
- Dry skin, burning.
They can be used for pain that occurs in the following pathologies:
- Neuralgia;
- Tendon inflammation;
- Osteochondrosis;
- Deforming arthrosis;
- Myalgia;
- Injuries of the musculoskeletal system, bruises and sprains.
Complete analogues of Diclofenac are available for sale:
- Ortofen;
- Voltaren;
- Diclovit.
Elimination of pain in muscles and after cesarean section
Muscle pain is not uncommon for nursing mothers. During the postpartum period, they are often felt in the lower back, back, neck, legs and other parts of the body. Such pain in young mothers develops as a result of excessive muscle tension during childbirth and does not require drug treatment. But if the pain is severe and prevents a woman from enjoying motherhood, local painkillers for lactation in the form of gels and creams for external application will help her. These drugs include Finais, Nurofen-gel, Menovazin, Biopin, Traumeel-S. Despite the fact that these products are intended for application to the surface of the skin, their active components in small quantities can penetrate into breast milk and harm the health of the newborn baby. To prevent possible undesirable consequences for the baby’s health, nursing mothers should use external painkillers only in case of severe muscle pain.
Many women who become mothers as a result of cesarean section experience pain in the area of surgical sutures after childbirth. To alleviate the condition of such patients, experts prescribe a pain reliever during lactation in the form of No-shpa. For nursing mothers, this antispasmodic is prescribed in the form of tablets and solution for injection. The number of drugs approved for relieving pain in nursing mothers after cesarean section also includes Ultracaine solution. It is widely used in gynecological practice and is considered safe even for newborns.
When taking painkillers while breastfeeding, women need to understand that all medications, without exception, can negatively affect their young children. To minimize the negative impact of the anesthetic on the baby's body, a nursing mother should use it immediately after feeding. In this case, the drug will have time to be absorbed and partially eliminated from her body before she starts her next feeding.
How to pacify pain faster
Depending on the type of pain, approved medications may differ.
Headache

To relieve headaches, you can use medications based on ibuprofen and paracetamol.
If you have cephalalgia, you should not use medications containing acetylsalicylic acid and caffeine, such as:
- Citramon P;
- Coficil;
- Askofen-P.
Acetylsalicylic acid can cause allergies, bleeding, digestive and central nervous system disorders in a child. Caffeine can cause overexcitation and increased heart rate in a baby.
Therefore, any pain reliever for a nursing mother that contains caffeine and acetylsalicylic acid is contraindicated.
Toothache
If a toothache occurs, it is better to immediately consult a dentist, especially since Ultracaine is allowed for local anesthesia for nursing mothers.
When you can’t get an appointment to cope with the pain, medications based on paracetamol or ibuprofen will help.
Groin pain
If you experience pain in the groin, you should not take any analgesics without a doctor’s recommendation, as they can blur the clinical picture and the diagnosis will be made incorrectly.

In addition, discomfort can be caused by a dangerous pathology, including ectopic pregnancy, rupture of an ovarian cyst, appendicitis, which without emergency assistance can lead to death.
Muscle pain
In case of myalgia, it is better to give preference to external medications. Drugs based on diclofenac and ibuprofen, such as Dolgit, Diclovit, Naklofen, can relieve pain.
Haemorrhoids
Often during lactation a woman develops hemorrhoids. If pain occurs due to this pathology, suppositories and Procto-Glivenol cream can be used. They are used for external and internal hemorrhoids. The drug contains lidocaine and tribenoside as active ingredients.
An antihemorrhoidal drug is prohibited in case of intolerance to its composition and liver failure. It can cause allergies, itching and burning in the anus.
You can also relieve pain during breastfeeding with suppositories and Relief Advance cream. The therapeutic effect of them is explained by benzocaine.

The drug is used to relieve pain from hemorrhoids, anal fissures, after operations on the rectum and during diagnostic procedures.
Relief Advance should not be used in case of hypersensitivity to its composition, thromboembolism, or low granulocyte levels.
During drug treatment, allergies, itching and redness of the anorectal area may occur.
Pain after cesarean
For pain relief after a caesarean section, as after any other operation, drugs based on paracetamol and ibuprofen are allowed.
Pain during menstruation
For painful menstruation during lactation, you can take medications containing ibuprofen and paracetamol: Advil Liquid-Jels, Faspik.
Recommended pain relievers for breastfeeding
For toothache
During the period of breastfeeding, the mother's body suffers from a lack of calcium. Therefore, she may develop dental diseases. You can endure the onset of pain and use folk remedies. But if the pain becomes unbearable, and a visit to the dentist is impossible for one reason or another, a nursing mother can use the drug Ketanov: the pill will temporarily relieve severe pain. It will not eliminate the cause of the pain; the action is aimed at reducing pain. Use no more than twice a day, no longer than three days.
Ointments can be used as pain relievers for toothache. These methods of alleviating pain are allowed for a baby when teething, which means that a mother can also use them for toothache:
- Kalgel (based on lidocaine).
- Traumeel.
- Kamistat Baby in the form of a gel: in addition to lidocaine, it contains chamomile extract.
- Dentol Baby - has a cooling, analgesic effect, relieves inflammation.
It is worth considering that all of these drugs have a short-term effect and eliminate pain temporarily. If possible, you should visit your dentist immediately.
To relieve pain during medical procedures, dentists use injections of Lidocaine or similar Ultracaine.
For headaches
Headache is a common symptom. Fatigue, lack of sleep, worry about the baby, etc. are the main reasons. It often goes away without taking medications; it is enough to use folk remedies or a head massage.
A nursing mother is prescribed the following painkillers to relieve headaches:
- Paracetamol preparations (Strimol, Efferalgan, Panadol);
- Nurofen, Avil, Ibufen with Ibuprofen in the composition.
Taking painkillers while breastfeeding is a necessary measure. First you need to try to relieve pain without medication: relax, walk in the fresh air, take a bath.
After caesarean section
Pain in the groin area is a companion during the first months of a woman who gives birth by cesarean section. The following drugs are prescribed:
- No-spa: as tablets or injections, non-systemically;
- Ultracaine is effectively used by gynecologists and is not dangerous for nursing mothers;
- Ketoprofen, Ibuprofen.
In case of prolonged pain, if there is discharge and the suture does not heal well, you need to visit a doctor.
For menstruation during lactation
During breastfeeding, pain during menstruation is practically absent. This is due to the production of a hormone that prevents blood from stagnating in the uterine cavity and thereby reduces pain. If they still exist and cannot be tolerated, gynecologists prescribe No-shpu during menstruation. The effect occurs a quarter of an hour after taking the medicine (2 tablets of 40 mg each). A one-time dose will not affect the quality of milk and the condition of the child. Do not take for a long time.
Pain syndrome is also effectively relieved by drugs: Ketanov, Ketorol, Paracetamol. It is recommended that if you experience severe pain during menstruation, consult a specialist.
What to do if you need to take a potent drug
It happens that a nursing woman needs to take a prohibited drug or has contraindications to approved drugs, then for the period of therapy she is recommended to transfer the baby to artificial feeding.

How long after you can start breastfeeding again depends on the specific medication, since the time it takes for drugs to be eliminated from the body varies.
To prevent the milk from running out and the baby to take the breast again, the following rules must be followed:
- Express during treatment;
- Do not bottle-feed your baby, as it is easier to suck on and it is possible that he will not breastfeed afterwards;
- You can feed your baby using a syringe without a needle.
The effect of painkillers on the baby
The well-known children's doctor of the highest category, E. Komarovsky, believes that it is advisable for a nursing woman to abstain from any medications, including painkillers. During lactation, the painkiller is directly transported into the milk, and then immediately into the baby’s body, which is not yet fully formed. But no one is immune from situations when the pain becomes unbearable. In this case, you should discuss taking pain medications with your doctor.
Any medications, even conditionally approved for breastfeeding, have an impact on the health of the baby. The small body does not yet know how to remove toxic substances, which means that any drug can poison the baby.
In addition, even an approved painkiller in the wrong doses can cause milk loss. This happens when a large dose of the drug was taken, or the medicine was chosen incorrectly. Before taking a painkiller, think about how necessary it is? After all, many mothers, even with the slightest headache, immediately resort to pills, although you can get by with warm tea and a half-hour rest.
Other ways to relieve discomfort
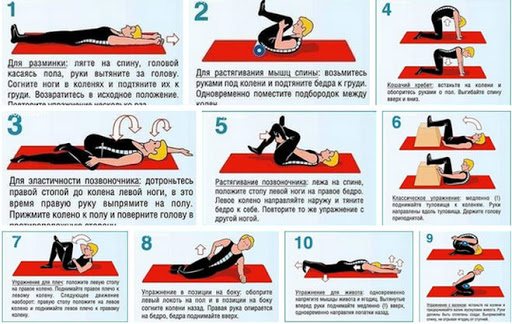
You can tidy up your back muscles with exercise therapy
If a nursing mother’s back hurts, for example, due to a lumbago as a result of a pinched nerve, you can do without medications.
Back treatment methods during breastfeeding:
- Massage. The usual kneading and rubbing of the painful area gives a good effect. However, you should not overuse it: every movement should be soft, smooth, without jerking. It is recommended to massage until slight redness appears on the skin.
- Physical activity. Therapeutic exercises can help relieve discomfort caused by muscle spasms. You can bend to the sides, forward and backward, and make circular movements with your body.
- Applying a cold compress. The method is effective for muscle pain in the back. Take any item from the refrigerator and wrap it in linen to prevent frostbite. You can also use a heating pad, into which water is poured at room temperature.
- Cold and hot shower. Alternately douse with hot and cool water (it is forbidden to turn on cold water). This helps to dilate blood vessels and relieve pain.
- Breathing exercises. The method is effective for the body as a whole. The functioning of internal organs and systems returns to normal, psychological disorders go away.
- Meditation. You need to take a relaxing position, close your eyes and focus on thoughts and sensations that are not associated with pain.

Horseradish leaves as a compress for the back
You can treat lumbago while breastfeeding at home using folk remedies that are easy to do with your own hands:
- from a cabbage leaf: beat it a little (you can use a rolling pin) to obtain juice, apply to the sore spot under a compress for 15-20 minutes;
- from lemon pulp, which has an analgesic effect: apply the lemon with a cut to the skin, leave for 30-40 minutes;
- from beet juice: a cotton pad or gauze swab is soaked in it and applied under a compress to the skin for 30-40 minutes.
A solution of vinegar, prepared in a 1:1 ratio with water, is used for inhalation (the product has a calming and relaxing effect on the body).










