Urogenital chlamydial infection (urogenital chlamydia) is the most common sexually transmitted infection (STI). According to the World Health Organization (WHO), about 90 million new cases of chlamydial infection are registered annually in the world. And, apparently, this is just the “tip of the iceberg.”
The causative agent of urogenital chlamydia is Chlamydia trachomatis , an intracellular parasite close to gram-negative bacteria, but, unlike bacteria, they have lost the ability to produce metabolic energy. This determines their intracellular growth. Belongs to the Chlamydiaceae family.
The source of infection is a person with an acute or chronic form of urogenital chlamydial infection (both with clinical manifestations and asymptomatic).
The main routes of transmission of chlamydial infection:
- Sexual;
- Vertical (infection of the fetus from the mother in utero or during the passage of an infected birth canal).
Susceptibility to urogenital chlamydial infection ranges from 60 to 100%, and is especially high in immunodeficiency of any origin.
Urogenital chlamydial infection predominantly affects the sexually active part of the population (age 17-25 years). Among sexually active, clinically healthy women, chlamydia infection is, according to various sources, 8-40% (on average about 15%), among men - approximately 10%. The number of mixed infections caused by a combination of several microorganisms (gonococci, trichomonas, ureaplasma, mycoplasma, etc.) is also increasing.
Urogenital chlamydia is characterized by a long asymptomatic course, which leads to widespread infection. Since the carrier of the causative agent of chlamydial infection does not suspect anything for a long time and passes it on to sexual partners. The development of pronounced clinical manifestations of chlamydial infection often occurs already at the stage of complications. This leads to late diagnosis and long-term, not always successful treatment.
Possible complications of chlamydia when spreading beyond the urogenital tract include:
- chlamydial conjunctivitis;
- chlamydial pharyngitis;
- chlamydial hepatitis;
- Reiter's disease is the most severe complication of chlamydia. It occurs in people with a genetic predisposition and is manifested by a triad of clinical manifestations - arthritis, urethritis and conjunctivitis. Men get sick 20 times more often than women.
Urogenital chlamydia in women
Uncomplicated urogenital chlamydia in women occurs in the form of mucopurulent cervicitis - inflammation of the cervix.
Symptoms of chlamydia in women: tingling, itching or burning when urinating, pain in the lower abdomen and groin area, slight vaginal discharge between menstruation or during sexual intercourse, slight bleeding from the genital tract, conjunctivitis. The temperature may rise to subfebrile levels. Symptoms are generally nonspecific and laboratory testing (chlamydia testing) is required to make a diagnosis. In addition, up to 75% of cases of chlamydia in women are asymptomatic and manifest themselves already at the stage of complications.
Chlamydia can also affect other organs, spreading upward - “ascending” chlamydia - and leads to pelvic inflammatory diseases (PID): endometritis, salpingitis, salpingo-oophoritis, perihepatitis (Fitz-Hugh-Curtis syndrome), urethritis, cervicitis, proctitis.
In turn, PID often causes serious reproductive dysfunction. Women with a history of PID have a 7-10-fold risk of developing an ectopic pregnancy. In 40% of such women, pregnancy in the future is impossible, and in 60% of women who become pregnant again, an ectopic pregnancy develops again in 12% of cases, and spontaneous abortion in 15-20% of cases.
In approximately 50% of women suffering from infertility, the causative factor is chlamydial infection.
Analysis for chlamydia during pregnancy: with chlamydia in women during early pregnancy, the formation of infectious embryopathies, which are manifested by congenital malformations of the fetus and primary placental insufficiency, is possible. This often ends in a non-developing pregnancy or spontaneous miscarriage.
During pregnancy at a later stage, secondary placental insufficiency, impaired production of amniotic fluid (amniotic fluid), and premature birth may develop.
Culture for Chlamydia trachomatis with determination of sensitivity to antibiotics
This is a microbiological study that allows us to identify the causative agent of chlamydia infection - Chlamydia trachomatis - in the biomaterial being studied and determine its sensitivity to antibiotics.
Synonyms Russian
Culture for chlamydia with determination of titer and sensitivity to antibiotics.
English synonyms
Chlamydia trachomatis culture, bacteria identification and susceptibility.
Research method
Microbiological method.
What biomaterial can be used for research?
Conjunctival smear, urogenital smear, prostate secretion, synovial fluid, ejaculate.
How to properly prepare for research?
- For women, the examination (the procedure for taking a urogenital smear) is recommended to be carried out before menstruation or 2-3 days after its end.
- Men should not urinate for 3 hours before taking a urogenital smear.
General information about the study
Chlamydia trachomatis are intracellular parasites primarily affecting the genitourinary system. The source of infection is a patient with chlamydia or an asymptomatic carrier. It is mainly transmitted sexually, but a vertical route is also possible - from a sick mother to a child during childbirth. Chlamydia trachomatis primarily affects the mucous membranes and is the cause of trachoma, lymphogranuloma inguinal, and many other diseases. In men, Chlamydia trachomatis causes non-gonorrheal urethritis, epididymitis, prostatitis, conjunctivitis, atypical pneumonia, reactive arthritis and infertility, in women - urethritis, cervicitis, salpingitis, endometritis, conjunctivitis, atypical pneumonia, reactive arthritis, infertility, ectopic pregnancy, as well as obstetric pathologies. – premature rupture of amniotic fluid and premature birth. In newborns, Chlamydia trachomatis leads to the development of conjunctivitis and atypical pneumonia.
Chronic asymptomatic infection and reinfection are common and may play an important role in the immunopathological reactions that cause trachoma blindness and fibrosis of the upper urinary tract, and such infections contribute to pelvic inflammatory disease, infertility, ectopic pregnancy and pneumonia in children.
One of the methods for identifying Chlamydia trachomatis and the only method for determining their sensitivity to antibiotics is cultivation on nutrient media (seeding). In addition, this is the most reliable way to confirm the diagnosis of inguinal lymphogranuloma.
What is the research used for?
- To establish the cause of inflammatory diseases of the genitourinary system.
- To determine the cause of keratoconjunctivitis.
- To select rational antibacterial therapy and evaluate its effectiveness.
- For differential diagnosis (along with other studies) of diseases that occur with similar symptoms, such as gonorrhea, mycoplasma, ureaplasma infection.
When is the study scheduled?
- If a chlamydial infection is suspected, including inguinal lymphogranuloma, trachoma.
- For infertility or ectopic pregnancy.
- If the results of a serological test for Chlamydia trachomatis are positive.
- After completion of antibacterial therapy (not earlier than 14 days after discontinuation of the drug).
What do the results mean?
Reference values: negative.
Reasons for a positive result
- Chlamydial infection.
Reasons for a negative result
- No chlamydial infection.
What can influence the result?
Previous antibacterial therapy.
Also recommended
- Chlamydia trachomatis, DNA [real-time PCR]
- Chlamydia trachomatis, IgA
- Chlamydia trachomatis, IgG
- Chlamydia trachomatis, IgM
- Mycoplasma genitalium, DNA [real-time PCR]
- Mycoplasma hominis, DNA [real-time PCR]
- Ureaplasma species, DNA quantitative [real-time PCR]
- Neisseria gonorrhoeae, DNA [real-time PCR]
- Trichomonas vaginalis, DNA [real-time PCR]
- Spermogram
Who orders the study?
Gynecologist, urologist, venereologist, ophthalmologist, pediatrician, rheumatologist.
Literature
- Lifshits V.M. Laboratory tests for human diseases: a reference book for doctors / V.M. Lifshits, V.Ya. Sidelnikova. – M.: “Triad-X”, 2003. – 352 p.
- Encyclopedia of clinical laboratory tests / translation from English. edited by V.V. Menshikov. – M.: Publishing house “Labinform”, 1997. – 960 p.
- Stamm WE, Jones RB, Batteiger BE Introduction to chlamydial diseases; Stamm WE, Jones RB, Batteiger BE Chlamydia trachomatis (trachoma, perinatal infections, lymphogranuloma venereum, and other genital infections). In: Principles and practice of infectious disease / GL Mandell, Bennett JE, Dolin R (Eds) ; 6th ed. – Churchill Livingstone, Philadelphia, PA 2005. – 2701 p.
- Chlamydia trachomatis infection. In: Oxford handbook of genitourinary medicine, HIV, and Aids / R. Pattman (Eds) ; 1st edition. – USA: Oxford University Press, 2005. – 580 p.
Urogenital chlamydia in men
In 25-30% of cases, chlamydia in men occurs with unexpressed clinical manifestations and remains unrecognized for a long time.
Uncomplicated chlamydial infection occurs in men most often in the form of urethritis - inflammation of the urethra.
Symptoms of chlamydia in men: itching or burning during urination, pain in the scrotum, redness around the external opening of the urethra, slight bleeding during ejaculation or at the end of urination, conjunctivitis. The temperature may rise to subfebrile levels. Symptoms are generally nonspecific and laboratory testing (test for chlamydia) is necessary to make a diagnosis.
The most common complication of urogenital chlamydia in men is epididymitis (inflammation of the epididymis). Epididymitis can lead to the development of infertility due to damage to the tissue of the spermatic cord or suppression of normal testicular secretion due to autoimmune processes.
What is the importance of performing a PCR test?
If the causative agents of the disease are not detected in time, bacteria and protozoa that have entered the body can cause a chronic inflammatory response. It involves the urogenital tract and organs of the genitourinary system. As a result, the patient suffers from discomfort in the intimate area, painful urination, and discomfort during sexual intercourse.
As the disease progresses, the organs of the reproductive system (uterus, ovaries and tubes in women, prostate gland, testicles and their appendages in men) may be involved in the inflammatory process, which can further lead to chronic inflammation, the formation of adhesions and possible problems with conception and pregnancy . To avoid this, once a year or more often, it is advisable for men and women of reproductive age to take a smear test for gonorrhea, chlamydia and other infections.
Laboratory diagnosis of chlamydial infection
Early detection of chlamydial infection makes it possible not only to prevent its further spread and transmission to offspring, but also to significantly reduce the risk of complications leading to reproductive dysfunction.
Indications for testing for chlamydia:
- preventive examination;
- presence of characteristic complaints;
- pregnancy planning;
- examination of pregnant women;
- complicated obstetric and gynecological history;
- suspicion of urogenital chlamydia;
- before surgical interventions on the genitals and pelvic organs;
- suspected conjunctivitis or arthritis of chlamydial etiology.
Appointment with a urologist
[/su_posts]
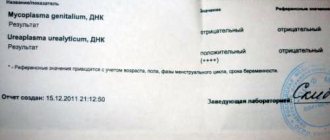
Explanation of PCR analysis.
When performing a PCR test for chlamydia, two results are possible: negative and positive.
- A negative PCR result indicates that no traces of chlamydia were found in the biological material. Therefore, there is no infection in the body.
- A positive PCR test result indicates that chlamydia is present in the patient’s biological material.
The PCR method as a means of detecting chlamydia is characterized by higher accuracy and reliability than the ELISA blood test. Therefore, you can trust the decoding of its results; it is mandatory to submit it if you suspect the presence of chlamydia in the body.
ELISA blood test results
The main advantage of the ELISA blood test is the ability not only to determine or refute the presence of chlamydia in the human body, but also to monitor the dynamics of the development of the infection. Deciphering the ELISA analysis can give one of the results below.
Absence of IgM, IgG antibodies.
If, as a result of the ELISA test for chlamydia, antibodies to them were not diagnosed, we can come to the conclusion that this infection is not familiar to the patient’s body.
Absence of IgM antibodies, presence of IgG antibodies.
If, as a result of ELISA, only IgG immunoglobulins to chlamydia are detected in the patient’s blood, this indicates that he suffered from the disease in the past, but is now inactive.
Presence of IgM antibodies, absence of IgG antibodies.
If the ELISA test for chlamydia shows exclusively IgM immunoglobulins, the infection appeared in the patient’s body relatively recently. Antibodies to chlamydia IgM can appear in the blood within 4-7 days after infection; after a few weeks (on average 8-10) they disappear.
Presence of IgM and IgG antibodies.
If the ELISA transcript indicates that immunoglobulins of both groups are present in the patient’s blood, two assumptions can be made. The first option is that chlamydia was introduced into the patient’s body several months ago. The second option is that the infection has reactivated in the human body.
The accuracy of the chlamydia ELISA test is approximately 60%. Therefore, it should be used only in conjunction with other studies, and not as an independent means of detecting chlamydia.
CLICK TO MAKE AN APPOINTMENT, TEST OR ULTRASOUND
If you find an error, please select a piece of text and press Ctrl+Enter
PCR analysis for chlamydia
In diagnosing chlamydia, of all existing methods, the polymerase chain reaction (PCR) method is recognized as the most reliable.*
Advantages of PCR diagnostics for chlamydia:
- Direct determination of chlamydia in biomaterial . PCR is a molecular biological method that is aimed at identifying DNA fragments specific to chlamydia and directly indicating the presence of infection
- High specificity . In the biomaterial subjected to analysis, the genetic material of chlamydia is detected - a DNA fragment. It is specific and not the same among DNA-containing organisms.
- High sensitivity. To perform PCR analysis, the presence of single chlamydia cells in the biomaterial is sufficient. The sensitivity of PCR analysis is 10-100 cells in a biomaterial, when other tests have 103-105 cells (microscopic, bacteriological methods). These methods do not allow identifying the pathogen in 20-40% of infected individuals, while the PCR method allows identifying chlamydia in 98-100% of patients.
- The versatility of the PCR method. Along with the detection of chlamydia DNA in the biomaterial under study, the PCR method allows the simultaneous detection of several pathogens, for example, Trichomonas, gonococci, etc.
- Speed of obtaining results. PCR analysis is fully automated, which allows you to obtain results in a short time, from 1 to 3 calendar days.
- Diagnosis of latent and sluggish forms of chlamydia. The PCR method can detect chlamydia, even if it is asymptomatic.
To test for urogenital chlamydia using the PCR method, you can submit: scrapings from the urethra, urine, prostate secretions in men, scrapings from the cervical canal, vagina in women.
For diagnostic activities, we use reagent kits from the Federal Budgetary Institution Central Research Institute of Epidemiology of Rospotrebnadzor, which have an EU certificate of conformity and are used not only in our country, but also abroad.
Preparation:
- in women, a smear to determine chlamydia, gonorrhea and other infections is taken outside the menstrual period;
- 7-14 days before the study, stop taking antibiotics;
- a week before collecting biomaterial, avoid douching, insertion of vaginal suppositories, and application of local antiseptic preparations;
- do not have intimacy one day before the test;
- on the evening before the diagnosis, take a shower, and then do not wash yourself again;
- To get reliable results, a smear for gonorrhea and other STIs should be taken in women and men 2-3 hours after urination.
Diagnosis of chlamydial infection in CMD
- Chlamydia, qualitative DNA determination, PCR
- Chlamydia, DNA quantification, PCR
- Chlamydia, qualitative determination of ribosomal RNA using the NASBA method
- Chlamydia, semi-quantitative determination of IgG antibodies, ELISA
- Chlamydia, semi-quantitative determination of IgA antibodies, ELISA
- Chlamydia, qualitative determination of IgM class antibodies, ELISA
Considering the high frequency of mixed infections, in addition to testing for chlamydia, it is advisable to use a wider range of studies, and in women, a mandatory determination of the quantitative ratio of vaginal microflora:
- Comprehensive STI research, DNA quantification, PCR
- Urogenital infections in men, DNA quantification, PCR
- Urogenital infections in women, DNA quantification, PCR
- Florocenosis
- Florocenosis and Microscopy
- Florocenosis and NCMT
- Florocenosis and NCMT and Microscopy
For the best choice of tests, consult your doctor.
*Federal clinical guidelines. Skin diseases. Sexually transmitted infections. 2021
Where in St. Petersburg can you get tested for STIs at an affordable price?
To undergo diagnostics at one of the most affordable prices in St. Petersburg, we invite you to the medical office. Here you can get tested for other sexually transmitted infections 7 days a week, at a time that suits you. Current prices for PCR analysis for gonorrhea, trichomoniasis, mycoplasma, ureaplasma and chlamydia are listed on the website. If you still have any questions about the preparation and cost of the study, you can contact our managers at the phone numbers given in the “Contacts” section.
Who is the examination indicated for?
Absolutely all people who have had sexual intercourse at least once without personal protective equipment. A polymerase chain reaction study should be performed. In addition, it is advisable to conduct the examination among a large contingent of citizens.
PCR for chlamydia is most appropriate in the following situations:
- any symptoms of problems in the genitourinary area
- low-grade fever without a clear reason
- decreased ability to work
- frequent change of sexual partners
- infertility
- prostatitis
- decreased sensations from sexual intimacy
- low libido or erectile dysfunction
- pregnancy
In the latter case, PCR must be carried out. Since microorganisms can cause problems during pregnancy.
It is better to carry out the study before conception, and if the result is positive, carry out treatment. However, even during pregnancy, adequate therapy will help avoid miscarriage.
STANDARDS AND DECODING
The essence of the analysis is that the DNA of the bacterium that needs to be detected is copied many times using specific enzymes. As a rule, many cycles are carried out, with each of which the desired DNA is doubled, which ultimately makes it possible to accurately identify it.
The result of the study can be obtained within a few hours, since PCR diagnostics do not require isolation and long-term cultivation of a pathogen culture, as with bacteriological culture.
When testing blood for chlamydia trachomatis, the norm is a negative result, which confirms the absence of chlamydial infection. The analysis should only be deciphered by a qualified specialist who will analyze all the indicators and make the correct diagnosis.
Detection of chlamydia in cell culture (on McCoy medium)
This method is unique in that it allows one to evaluate not only the quality of the therapy performed, but also to determine the sensitivity of chlamydia to various groups of antibacterial drugs.
The essence of the method is to infect the treated cell culture with the collected material, followed by inoculation on a nutrient medium and incubation for two days. The presence of chlamydia in the resulting cells is determined by PCR.
To determine sensitivity to antibiotics, growth medium containing a specific antibacterial agent is added to the treated cell culture and incubated for 5 days.
The effectiveness of the drug is determined by the absence or slowing of growth in certain groups. The presence of growth indicates resistance to the antibiotic added to the nutrient medium.
The disadvantages of this diagnostic method are its duration (7 days) and high cost, so it is used extremely rarely in clinical practice. Typically, the indication for its use is long-term, ineffective antibacterial therapy.
Analysis steps
How many days the analysis is done depends a lot on the sequence and speed of collecting the material and delivering it to the laboratory. Even the time factor will be important, since the substrate obtained in the morning will be analyzed on the same day.
The complete sequence of stages of PCR analysis for chlamydia is as follows:
- examination by a specialist
- taking biomaterial
- packaging in a physiological environment for chlamydia
- delivery to the laboratory
- conducting a test
- medical verification
- issuing the result
The immediate duration of testing does not exceed 4 hours. However, due to delays in transportation or late collection of material, the analysis is ready only the next day.
A prerequisite for the reliability of the study is medical verification. This means that a laboratory technician personally examines the test and checks for the presence of chlamydial DNA.
There are two options for carrying out polymerase chain reaction - quantitative and qualitative.
In the second case, the result will be obtained faster, since the calculation of genomic equivalents of the microorganism is not required. This also determines how much the research costs. If a quantitative result is obtained, the price will be higher.
However, in practical medicine the price range for PCR is not too high. Since many people need to undergo examination.