What is immune status?
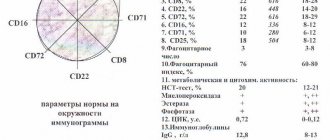
Immune status determines the number of different cells of the immune system. For people with HIV, the number of CD4 cells, or T-lymphocytes, is important - white blood cells responsible for “recognizing” various pathogenic bacteria, viruses and fungi that must be destroyed by the immune system. CD4 cell count is measured as the number of CD4 cells per milliliter of blood (not the whole body). It is usually written as cells/ml. The CD4 cell count in an HIV-negative adult typically ranges between 500 and 1200 cells/mL. HIV can infect CD4s and make copies of itself in them, causing the cells to die. Although cells are killed by HIV every day, millions of CD4 cells are produced to replace them. However, after some time, the CD4 count may decrease and even drop to dangerous levels.
What is HIV infection
HIV infection is a dangerous viral disease of the human immune system, the causative agents of which are HIV-1 and HIV-2 (human immunodeficiency viruses of the retrovirus family), which are able to penetrate (and remain active there for quite a long time) in lymphocytes, macrophages, and also nerve cells. As a result, there is a progressive (albeit slowly developing) damage to such organic systems as the immune and nervous, which is manifested by the development of multiple secondary infections and neoplasms in the patient.
These pathogens contain RNA and the enzyme reverse transcriptase in their genome, with the help of which DNA is synthesized on the RNA matrix of the virus for subsequent integration into the genetic apparatus of the cell of the future host. Most often in the human body, HIV seeks to infect the genome of T-lymphocytes, which have a large number of CD receptors on their surface, as well as B-lymphocytes, macrophages and some other cells (for example, the intestinal mucosa), where the embedded DNA of the virus remains for life.
Due to polyclonal activation of B lymphocytes, the synthesis of immunoglobulins sharply increases, which (accompanied by the constantly occurring replication of HIV) leads to dysfunctional depletion of the immune system. As a result, the cells designed to protect the human body themselves become a source of infection, as they begin to work as virus producers. Further, immunity gradually (over many years, during which a person feels practically healthy) decreases to a critical point, when the body is no longer able to fight any infection, even the simplest and safest for healthy people.
Does the CD4 count tell you about it?
For most people with HIV, their CD4 count usually declines after a few years. A CD4 count between 200 and 500 indicates a suppressed immune system. If the CD4 count falls below 350 or begins to decline rapidly, this is a reason to talk to your doctor about prescribing antiretroviral therapy (ART), since with such an immune status there is a risk of AIDS-related diseases. The main thing that the CD4 count tells us is the state of the immune system.
Changes in CD4 count. The CD4 count can increase and decrease again as a result of infections, stress, smoking, exercise, the menstrual cycle, taking birth control pills, depending on the time of day and even the time of year. Moreover, different test systems may give different CD4 count results.
That is why it is very important to regularly get tested for your immune status and look at changes in the results. It is impossible to assess the health status of an HIV-positive person with one single test. It is also best to measure your CD4 count in the same clinic, around the same time of day. If you have an infection, such as a cold or herpes, it is best to delay getting tested until your symptoms have gone away.
If you have a relatively high CD4 count, no symptoms, and are not taking antiretroviral therapy, getting your immune status tested every 3 to 6 months is sufficient. However, if your immune status is rapidly declining or you start taking medications, your doctor should suggest you get tested more often.
If your CD4 cell count varies greatly from time to time, your total white blood cell count may be changing, for example due to an infection. In this case, the doctor will pay attention to other indicators of immune status. For example, the CD4/CD8 ratio.
CD8 are other cells of the immune system that are not affected by HIV. On the contrary, as HIV infection develops, their number increases: this is how the body reacts to the infection. However, if a person has a normal CD4 cell count, the CD8 count does not matter much. The CD4 percentage also indicates the true state of the immune system.
CD4 percentage. Instead of counting the number of CD4 per milliliter, your doctor can estimate the percentage that CD4 make up of the total number of white cells. This is the percentage of CD4 cells. Normally it is about 40%. A CD4 percentage of less than 20% is about the same as a CD4 count of less than 200 cells/mL.
About where it all started
In 2006, I started having problems with my skin, I had terrible eczema, I went to the doctor in Bendery.
They took my blood for analysis and prescribed treatment for scabies. It took me a month to treat her. I only got worse, and I came to them again. They took my blood again. For this reason, a car even came to the house, they explained that the previous analysis had failed. And again they didn’t say why and what the result was. I began to suspect, took a referral to Chisinau, went for a skin examination, I was treated all summer, but to no avail. It was 2006, I was covered in fungus and eczema and no one suspected anything.
And then, tired of all this, in search of adequate doctors, I ended up at the department of dermatology. I remember how after the examination the doctor told me: “You know what, you probably have AIDS.” And I: “How?!” After that I returned to Bendery. And finally they called me and told me that I had HIV. I spent almost six months in such ordeals.
What is viral load?
A viral load test determines the number of virus particles in a fluid, or more precisely, in the blood plasma. This test only detects HIV genes, that is, the RNA of the virus. The viral load result is measured in the number of copies of HIV RNA per milliliter. Viral load is a "predictive" test. It shows how quickly a person's immune status can decrease in the near future. If we compare the development of HIV infection with a train that goes to its destination (AIDS-associated diseases), then the immune status is the distance that remains, and the viral load is the speed at which the train is moving.
There are different types of viral load tests currently in use. Each test system is a separate technique for detecting viral particles, so the sensitivity of the test system will determine whether the result is considered low, medium or high. Nowadays, viral load tests are reliable for any subtype of the virus.
Natural variations. Viral load levels may rise or fall, but this does not affect a person's health. Research shows that for people not on antiretroviral therapy, the results of two viral load tests from the same blood sample can differ by up to three times. In other words, there is no need to worry if the viral load rises from 5,000 to 15,000 copies/ml without treatment. Even a twofold increase may turn out to be a simple error in the test system.
Ideally, you should take a viral load test when you are healthy. If you have had an infection or recently been vaccinated, your viral load may temporarily increase.
Significant changes. There is cause for concern only when the viral load remains elevated for several months or if the viral load has more than tripled. For example, if the viral load rose from 5,000 to 25,000 copies/ml, this is a significant change, since the result has increased fivefold. Still, it is better to retest to confirm the upward trend.
The effect of vaccinations and infections. If you have recently had an infection or been vaccinated, you may experience a temporary increase in your viral load. In these cases, it is recommended to postpone the test for at least a month after vaccination or illness.
Minimizing deviations. Information about changes in viral load will be more reliable if the tests are done in the same clinic using the same method. If this is your first time taking this test, try to remember the method that was used for it. In the future, when you take a viral load test (especially if you take it at another hospital), make sure that the same method is used to determine your load previously.
If you are not on antiretroviral therapy. If you are not on antiretroviral therapy, your viral load may be predictive of developing HIV infection without this therapy. Findings from a study examining changes in viral load in people not on antiretroviral therapy suggest that, when combined with CD4 cell count, viral load may predict the risk of developing symptoms in the future. By testing people with the same CD4 cell counts, the researchers found that symptoms developed more quickly in those with higher viral loads. In a group of people with the same viral load, symptoms developed more often in those with a lower immune status.
Taken together, CD4 cell count and viral load provide a basis for predicting the development of HIV infection in the short and medium term.
The decision to initiate antiretroviral therapy. The first thing that will help you make this decision is your CD4 cell count and your viral load.
Doctors recommend starting therapy before the immune status drops to 200 cells. In people with higher immune status, the decision to prescribe therapy may depend on the level of viral load, the rate of decline in immune status, the likelihood of strict adherence to therapy, the presence of symptoms, and the wishes of the patients themselves.
If you have been advised to start antiretroviral therapy but decide to wait, keep a close eye on your immune status and viral load.
Viral load in women. If we compare the same indicators of immune status in women and men, then in women, on average, it begins to decline with a lower viral load. However, this does not in any way affect how the body will respond to antiretroviral therapy.
What does an undetectable viral load mean? All viral load tests have a sensitivity threshold below which they cannot detect HIV. It may be different in different test systems. However, the fact that the viral load is not detectable does not mean that the virus has completely disappeared from the body. It's still there, but in such small quantities that the test has a hard time detecting it. In addition, viral load tests only measure the amount of virus in the blood. Even if you have an undetectable viral load, this does not mean that it is not, for example, in the semen.
What is the sensitivity threshold of modern tests? In most hospitals in Russia, test systems determine the amount of virus up to 400-500 copies/ml. Some modern hospitals use more sensitive tests that detect up to 50 copies/ml. A test system has already been developed that determines the level of virus in the blood up to 2 copies/ml.
About accepting a diagnosis
I was 46 years old at that time, and when I received the results of all the tests, I only had 8 immune cells.
When they told me about the diagnosis, I felt so bad that I didn’t even try to look for the reason, I decided to survive by any means necessary. I was admitted to the hospital for a month and a half, then I posted encouraging affirmations about HIV throughout the ward, read Louise Hay, convinced myself and other patients that this was not the end. Every morning I made everyone do exercises, we put on makeup before going around, we always put ourselves in order.
I spent a month and a half in the department. I was discharged with 10 immune cells. I felt very bad for 10 days, then there was a crisis night, then I clearly felt that something would happen that night - either I would remain alive, or it would be the end. Then some kind of vacuum formed, someone talked to me, they told me that I would live, I would help people, that I would open my own store. They say that this was a guardian angel.
Keeping Sexual Partners Safe
Regardless of viral load, people living with HIV can benefit from taking steps to protect themselves and their sexual partners. These steps may include the following:
- Take your antiretroviral drugs regularly and as directed . When used correctly, antiretroviral drugs lower the viral load, thereby reducing the risk of transmitting HIV to others. Once the viral load becomes undetectable, the risk of transmission through sexual contact is virtually zero.
- Get tested for STIs . Given the potential impact of STIs on the risk of HIV transmission in people receiving treatment, people with HIV and their partners should be tested and treated for STIs.
- Use condoms during sex . Using condoms and sexual activity that does not involve the exchange of body fluids reduces the risk of transmission.
- Consider pre-exposure prophylaxis . Partners should talk to their doctor about pre-exposure prophylaxis, or PrEP. This medicine is designed to prevent people from becoming infected with HIV. When taken as prescribed, it reduces the risk of contracting HIV through sexual contact by more than 90 percent.
- Consider post-exposure prophylaxis . Partners who suspect they have already been infected with HIV should talk to their doctor about post-exposure prophylaxis (PEP). This medicine reduces the risk of infection when taken within three days of possible exposure to HIV and continued for four weeks.
- Get tested regularly . Sexual partners infected with HIV should be tested for the virus at least once a year.