Detection of the corpus luteum on ultrasound is a clear sign of pregnancy. The corpus luteum is a gland in the female body that is formed during ovulation and can remain active for up to 12 weeks. The longer her lifespan, the higher the likelihood of pregnancy. If a woman fails to get pregnant, then perhaps gland pathology is to blame.
Corpus luteum during pregnancy
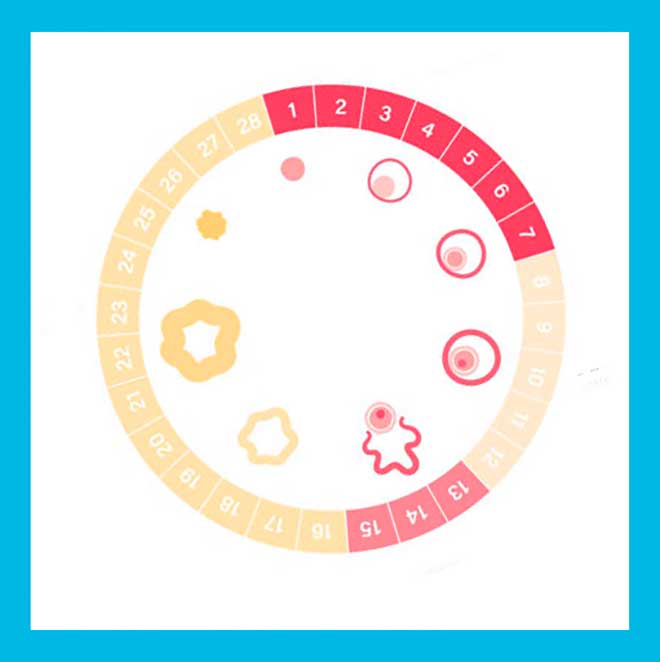
During ovulation, the egg matures and leaves the follicle. If fertilization does not occur during this period, then after a month a new egg matures, and the old one is removed from the body during menstruation. At the end of ovulation, a hormone-producing gland (progesterone and estrogen) is formed, which is called the corpus luteum. If fertilization does not occur, then it decreases, stops producing progesterone, and the menstrual cycle begins. And during pregnancy, the corpus luteum remains active, progesterone prevents the appearance of new eggs and prevents menstruation from developing. The gland disappears during the period when the placenta begins to produce the necessary substances on its own.
If conception has taken place
If, after leaving the follicle, the egg meets the sperm, fertilization occurs. In this case, the “lifespan” of the corpus luteum increases: it functions until 10-12 weeks of pregnancy. The body of the expectant mother needs it: VT actively produces progesterone, promoting the successful development of pregnancy.
By the end of the first trimester, the placenta has developed to the point that it is capable of producing progesterone. The need for a yellow body disappears. Having “transferred” its functions to the formed placenta, the body disappears.
HCG and VT
During pregnancy, the level of the hormone gonadotropin (better known as hCG) begins to increase. It stimulates the development of the “true” corpus luteum. If hCG has increased in the body, this is a kind of signal for VT, a signal for growth.
Blood flow in VT
The blood supply in the corpus luteum is higher than in other organs. It has many capillaries. Thanks to this feature, VT successfully distributes progesterone throughout the body’s circulatory system. Cholesterol and fatty acids come into the VT with blood; it is from them that the corpus luteum produces progesterone.
The better the blood flow in the VT, the more successfully it performs its functions.
Dimensions of VT during pregnancy
The size of the VT indicates the amount of progesterone it produces. And during pregnancy, it is extremely necessary: it allows the fertilized egg to be successfully implanted inside the uterus, and subsequently ensures the development of the fetus.
A VT diameter of 10 to 30 mm is considered normal. Within this normal range, the size of the VT may vary among different women. As a rule, when pregnancy occurs, the VT grows to 27-30 mm. Deviations, both downward (less than 10) and larger (more than 30) are a bad sign.
In the first case, it indicates progesterone deficiency, in the second, a cyst. The doctor will not miss the alarm signal and will prescribe additional tests and studies (ultrasound).
Pathology of the corpus luteum
Diseases of the corpus luteum can cause infertility. When underdeveloped, this gland produces low amounts of progesterone, which is unable to prepare the uterus for pregnancy. As a result, fertilization does not occur.
There are several reasons for this pathology:
- genetic predisposition;
- ovarian diseases;
- postoperative failure;
- post-medication failure;
- kidney disease;
- liver diseases.
Corpus luteum on ultrasound: how and why it is examined
Pelvic ultrasound allows you to determine:
- Dimensions of the yellow body.
- Its localization.
- The phase of development of the temporary gland (the possibility of pregnancy is determined by the phase).
- The presence of a fertilized egg in the internal genital organs.
- Endometrial thickness (measured to check whether the VT is doing its job).

On the 3-5th day of delay to detect pregnancy. Sometimes the blood flow in the VT is measured: as mentioned above, the better it is, the better the VT functions. If blood flow is poor, VT failure may be diagnosed. It is necessary to check the level of the hormone progesterone to maintain pregnancy.
Based on the results of the study, the doctor judges the woman’s reproductive ability and the possibility of carrying a child normally. An ultrasound scan is necessary if you are planning a pregnancy, want to confirm it, carry a child, or solve the problem of infertility. It is recommended for those who have had miscarriages or a “frozen” pregnancy.
In the ultrasound results, a woman may not find the inscription “corpus luteum”; ultrasound specialists may use the words “anechoic formation” instead. Don’t be scared by the word with the prefix “ano” (which means the opposite, the absence of any sign or condition): the corpus luteum cannot pulsate (cannot be echogenic) because it contains fluid. Therefore, the formation is called anechoic. The corpus luteum may not appear on ultrasound.

In order not to worry once again, you should not try to decipher the ultrasound results yourself. Go to the doctor and ask questions: he will explain everything.
Treatment of hormonal deficiency
Treatment of corpus luteum pathology during pregnancy is symptomatic. If a woman’s body does not produce enough progesterone, it must be taken additionally. There are oral, vaginal or rectal preparations, as well as skin creams with progesterone as an active ingredient. Urozhestan and Duphaston are most often prescribed. Hospitals may prescribe progesterone in ampoules. Each medicine should be taken on certain days. But before prescribing hormonal drugs, it will be necessary to undergo a full examination.
During drug treatment, constant monitoring is carried out - the patient undergoes ovulation tests, progesterone levels are checked, and the corpus luteum is observed on ultrasound.
The Medicenter clinic network employs professional endocrinologists who have extensive experience in treating hormonal deficiency of the corpus luteum during pregnancy.
Complications
We have already mentioned three possible complications associated with the development and functioning of VT:
- failure;
- cyst;
- weak blood flow.
Let's look at each in a little more detail.
Failure
If VT is too small or not visualized at all during ultrasound, they talk about risks and possible complications. Let’s be clear right away that complications are only possible. To find out if everything is okay with the child, you need to check the level of progesterone in the blood using a laboratory test.
Perhaps the ultrasound specialist simply did not see the VT on the monitor screen (this is not always possible). Thus, the absence of VT or its insufficient size is only a signal to undergo additional analysis and recheck the results at the next ultrasound. And the doctor will draw conclusions based on the results of observations.
Consequences
Insufficiency (or failure) of VT is a common problem; many women encounter it during pregnancy. Due to its small size, VT does not produce enough progesterone, so the pregnancy is at risk of termination.

Failure of VT is associated with infertility (becomes the cause of female infertility) and chronic miscarriage.
Causes
Sometimes the small size of the temporary gland is associated with a shortened second phase of the cycle (not 14 days, but 10 or less). If there is a genetic predisposition, VT insufficiency is associated with chromosomal abnormalities in embryo development. A test to identify such genes is needed.
Insufficiency of VT can also be caused by oncological diseases, disturbances in the functioning of the pituitary gland, in the functioning of the gonads, kidneys, liver, endocrine diseases, and hormonal imbalance. Additional diagnostics will help determine the cause and eliminate the risks.
Manifestations of deficiency
How is VT failure manifested? Failure of the menstrual cycle, thinning of the inner layer of the uterus (endometrium), which in turn affects the implantation of the fertilized egg (cannot take hold). Due to a lack of progesterone, the uterus contracts, as during menstruation, which prevents pregnancy from developing.
How to fix
The deficiency can and should be replenished (especially during pregnancy). They are replenished with drugs containing progesterone - Utrozhestan, Duphaston; in the hospital they use an oil solution of this hormone. But the doctor prescribes the treatment.
Cyst
Large sizes of the corpus luteum on ultrasound (if the VT is more than 30 mm, i.e. 50 or even 80) indicate pathology - the presence of a cyst. A cyst can form during pregnancy or without it.
Causes
The reasons for its appearance are not clear (not known to medicine). It may be due to impaired blood flow in the ovaries or stimulation of ovulation with hormonal drugs before IVF.

A cyst is formed at the site of VT, which for some reason did not disappear in due time. This occurs rarely - in 5% of women of childbearing age.
Doctors say the reason for the formation of cysts is frequent mono-diets (eating only one type of food - fruits, or only cereals, or only dairy), with which women overload their bodies. Sometimes work is blamed if it involves heavy physical activity or hazardous work. Women who have had abortions several times are also reproached. Apparently, doctors' debate about the reasons will continue for a long time.
Symptoms
The pathology occurs asymptomatically. Only for some women the cyst makes itself felt by nagging pain in the lower abdomen or cycle disorders. It is not dangerous to health (unless rupture or inflammation occurs). When diagnosing, doctors (even experienced ones) may confuse a cyst with a malignant tumor.
Consequences: rupture, inflammation
Typically, the cyst lives for 2-4 months and resolves on its own, without causing harm to health, without interfering with conception and the development of pregnancy. During pregnancy, as a rule, they disappear by 20 weeks. But sometimes it ruptures with internal bleeding. In this case, surgery cannot be avoided. If the cyst does not resolve, surgery is also recommended.

Cyst rupture can occur spontaneously. It can be triggered by injuries, violent sexual intercourse, or excessive physical activity. Accompanied by severe pain, weakness, and a drop in blood pressure.
The solution is constant monitoring
In addition to rupture, inflammation may begin. Therefore, constant monitoring is necessary: rechecking with professional modern ultrasound machines. Sometimes it is recommended to take a blood test to check for cancer markers.
Weak blood flow
Impaired blood flow during pregnancy must be corrected with the help of therapy (the doctor prescribes Utrozhestan and other similar drugs). This increases the chances of saving the child.
If blood flow remains insufficient, less progesterone will be produced. This can lead to various consequences: you won’t be able to get pregnant, or the egg won’t be able to implant in the uterus, and the pregnancy may stop developing. Lack of progesterone can also cause miscarriage. This (from the presence of risks) implies the need for constant monitoring by a gynecologist.
How long does it function?
How long does a VT live? The corpus luteum has a limited lifespan, but it is formed every month during the menstrual cycle. The functioning of the formation depends on whether the fusion of gametes has occurred or ovulation has been wasted and menstruation should begin.

If the fusion of gametes does not occur, the function of the corpus luteum gland begins to fade from the 12th day after ovulation. In a 28-day cycle, this is day 26. It dries out, gradually degenerating into scar tissue, producing less and less progesterone, which is why the endometrium of the uterus begins to shed. Menstruation, as a result of endometrial rejection, accompanied by bleeding, is a consequence of the extinction of VT function.
How long does it live after ovulation?
Each woman has her own length of the menstrual cycle. For some, the break between bleeding is 3 weeks, while for others it is 5. The time of ovulation depends on the duration of the cycle.
The period of existence of the corpus luteum in the ovary is in no way related to the length of the cycle. For women of all ages and nationalities, a single normal duration of existence of the temporary gland has been established. The corpus luteum is formed during the ovulatory period of the menstrual cycle and remains active for 12 to 14 days. If the period of operation of the gland is less than 10 days, then this is a deviation from the norm. In this case, gynecologists talk about the insufficiency of the second phase and take measures to correct this condition.
What happens to the corpus luteum after ovulation can be clearly seen on an ultrasound. Over the course of several days, it increases in size to produce the required amount of progesterone, and reaches its peak before the start of a new cycle. With the onset of menstruation, the temporary gland dissolves. In some cycles, it does not disappear with the onset of menstruation, but continues to function over the next month. As a rule, this period turns out to be anovulatory.
If conception has occurred, the corpus luteum increases the secretion of progesterone. This ensures the continuation of pregnancy. Regression of the temporary gland occurs in the second or third trimester, but only after the placenta has formed.
Formation process
The formation of the corpus luteum is divided into several stages:
- Proliferation is the appearance of a gland after the rupture of the follicle and the release of the egg. During this process, cell division begins and the formation of lutein, which has a yellowish tint. The corpus luteum acquires uneven edges and a heterogeneous structure.
- Vascularization is the stage of gland growth, during which it wraps around blood vessels and becomes embedded in the epithelial layer. This happens on days 13-17 of the cycle and is a small tumor with normal blood flow.
- Blooming - the corpus luteum reaches its maximum size, acquires brighter outlines and increases blood flow, on days 19-25 of the menstrual cycle.
- Regression - this stage will only occur if fertilization has not occurred and the egg dies. The corpus luteum decreases in size and disappears by the beginning of menstruation. Afterwards, scars or so-called hylian formations remain on the ovary.

Deviations
There are situations in medical practice when the presence of a gland does not correspond to its average values. This is preceded by some conditions and factors. Deviations are possible in the presence of a cyst or insufficiency of the corpus luteum.
If an ultrasound shows an increase in the diameter of the gland, then the doctor will suspect neoplasms. Their nature is a cyst. This pathology occurs due to hormonal imbalance and disappears without any help after several menstrual cycles.
A cyst larger than 40 millimeters requires treatment or surgery such as laparoscopy.
If the formation is more than 60 mm, then there is no way to do without surgical methods, since it can rupture.
If the corpus luteum is small in size by day of the cycle, hormonal therapy and long-term treatment are required due to the fact that most often these indicators are the cause of infertility.

What are the disorders in the development of the corpus luteum?
The main deviations in the normal formation of the corpus luteum are:
- functional failure; - cyst.
Both diagnoses are made after comprehensive examinations, which include ultrasound, blood tests for progesterone and hCG levels, gynecological examination, and study of the basal temperature chart. A woman is not at risk of harm from ultrasound during pregnancy; at the moment, ultrasound is the most informative and absolutely safe method of studying the condition of the fetus. It can be performed as many times as needed and at any stage of pregnancy.
Corpus luteum cyst is considered a harmless disease and rarely requires treatment. But it is better to detect the insufficiency or absence of the corpus luteum as early as possible, since this pathology threatens the termination of pregnancy in the early stages or the further development of placental insufficiency.











