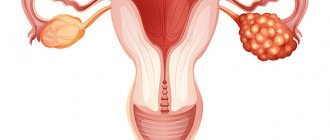
Premature ovarian failure is a form of primary ovarian failure. The pathological condition is characterized by menstrual irregularities (cessation of menstruation) and is very often diagnosed as premature menopause.
Premature ovarian failure is a reversible process and can be effectively treated. Symptoms of declining ovarian function most often appear in women aged 40 years. The most common symptoms include hot flashes, night sweats and headaches.
What is premature ovarian failure
The content of the article
Back in the first half of the 20th century, it was noticed that some young women around the age of 40 stopped menstruating. This condition was defined as premature menopause. In the course of research over the years, it was noticed that in the urine of women with early menopause there is an increased level of gonadotropins (hormones responsible for the proper functioning of the reproductive system).
Currently, this disease is defined as premature ovarian failure .
– POF).
It manifests itself as delayed menstruation in women under forty years of age. It is one of the types of primary ovarian failure. Delayed menstruation
The development of premature ovarian failure may be suggested by the appearance of early hot flashes before the onset of menstrual irregularities. Premature ovarian failure occurs in women in the fourth decade of life. This disease affects 1 in 100 women in the age range from 30 to 39 years.
A much lower incidence of 1 in 1000 occurs in women under 30 years of age. Hormonal disorders are confirmed by laboratory data. An increased level of gonadotropins in the urine and a decrease in the concentration of estradiol are determined. Premature ovarian failure, unlike menopause, is a reversible condition.
It is necessary to undergo a course of treatment. The effectiveness of therapy is confirmed by cases of resumption of ovarian function in women after a course of medications.
What is ovarian reserve
The content of the article
Ovarian reserve is the reproductive potential of the ovaries - the number of follicles that are able to grow and develop into a mature egg.
A girl is born with a certain ovarian reserve, which is about 1-2 million primary cells, which ultimately form oocytes. Every day, and then with every monthly cycle, the number of oocytes only decreases.
So, during puberty, a girl already has 300-500 thousand of them. Then most of the remaining oocytes are resorbed and in the end only 400-500 remain.
The remaining oocytes mature under the influence of hormonal balance. In each menstrual cycle, one of them ovulates. Therefore, the older a woman is, the less likely she is to conceive.
Not so long ago, 30-40 years ago, most women gave birth to children when they were only eighteen or twenty years old. Today things are different. After graduation, a woman goes to work, then focuses on career growth. Having children becomes a secondary problem: “I still have time for this,” “I’m not ready yet, I’ll think about the baby later,” say modern businesswomen.
For many, it has become the norm to start a family at the age of thirty, and only after a few years do thoughts about pregnancy arise. For many couples, this may be too late - the biological clock is ticking, and time does not spare anyone...
Reasons for the development of pathology - premature ovarian failure
Disruption of the normal functioning of the ovaries can occur as a result of the action of various factors on the woman’s body. Some cause accelerated atrophy of ovarian follicles. Another mechanism of action is to reduce the number of follicles containing eggs.
The most common causes of premature ovarian failure include the following:
- Genetic factors associated with damage to the X chromosome (an example would be Shereshevsky-Turner syndrome, which is characterized by X chromosome monosomy (XO), that is, the presence of only one X chromosome);
- Autoimmune diseases such as type 1 diabetes mellitus, hypofunction of the adrenal glands and/or thyroid gland, in addition, systemic lupus erythematosus, rheumatoid arthritis, vitiligo and Crohn's ulcer disease;
- Infectious diseases such as malaria, smallpox, inflammation of the appendages after mumps;
- Bacterial and viral infections;
- Inflammation of the ovaries (oophoritis),
- The effect of radiation therapy and chemotherapy.
What causes changes in ovarian volume?
The reasons why one ovary becomes larger may be the following:
- Appendicitis, while the right appendage increases, but the left ovary remains the same in diameter.
- Inflammation of the ovary, uterus or fallopian tubes.
- Ovulation, which is often accompanied by unilateral nagging pain, increased body temperature, and weakness.
- A single cyst (more than 3-5 cm in diameter) or multiple ovarian formations.
- PCOS.
- Cervical erosion. In this case, the microorganisms that provoked the development of pathology invade the ovarian tissue, resulting in the development of an inflammatory process.
- Malignant tumor of a paired organ.
Risk factors for developing the disease
The reason for the development of pathology in a large number of women has not been established. Stopping long-term use of oral contraceptives may lead to premature ovarian failure. In some cases, the disease may develop immediately after pregnancy.
As a result of the studies, the presence of risk factors for the development of this disease has been proven:
- high blood glucose levels;
- age;
- smoking.
Symptoms
| Occurrence (how often a symptom occurs in a given disease) | |
| Absence of pregnancy in a woman of childbearing age within one year of regular sexual activity without the use of contraceptives | 100% |
| Lack of hair or mild hair growth in the pubic area | 90% |
| Lack of hair growth or mild hair growth in the armpit area | 90% |
| Underdevelopment of breasts in women | 80% |
| Stopping menstruation | 80% |
| Pain during sexual intercourse in women | 5% |
Symptoms of premature ovarian aging
Stopping the ovaries leads to estrogen deficiency and the development of hormonal imbalance. This affects the functioning of all body systems. The development of the disease is characterized by the following symptoms:
- night sweats;
- tides;
- frequent mood changes;
- headaches and dizziness;
- increased predisposition to the development of diseases of the cardiovascular system and type 2 diabetes mellitus;
- weight gain;
- withering, aging of the skin;
- atrophic changes in the organs of the genitourinary system.
Tides
Weight gain
The above symptoms are very similar to the signs of menopause; it is important not to confuse these conditions and make the correct diagnosis.
Diagnosis of ovarian wasting syndrome
Initially, the doctor examines the patient, collects information about the beginning and course of her menstrual cycles, the time at which the first signs of ovarian dysfunction were noticed. As a rule, women suffering from SIS do not have noticeable organic damage, their physique is normal, without pathological features. However, they look older than their years, they show signs of early aging of the body - gray hair, wrinkles, dull skin color, etc. In the primary diagnosis of SSI, cases of exposure to negative external factors (toxic substances, radiation, etc.) are of great importance. ), as well as the presence of reproductive problems among the patient’s relatives.
To identify this pathological condition, a woman undergoes a comprehensive medical examination, including the following tests:
- A gynecological examination reveals an abnormally low secretion of vaginal lubrication and the “pupil” effect (the presence of mucus from the cervical canal on the vaginal part of the cervix), and bimanual palpation reveals underdevelopment of the uterus relative to the age norm;
- Ultrasound of the ovaries and other pelvic organs allows us to determine genital infantilism, reduction in the size of the uterus, homogeneous structure of the myometrium, hypotrophy of the endometrium and gonads;
- Metrosalpingography - contrast X-ray examination of the uterine cavity and tubes with contrast reveals thinning of the endometrium, fibrous atrophy of the glandular tissue of the ovaries and the absence of follicles;
- Using diagnostic laparoscopy, the doctor determines the presence of changes in the gonads and takes samples of their tissue for histological examination;
- A blood test for hormones reveals an increased concentration of gonadotropins, a sharp decrease in female sex hormones (estrogens and progesterone);
- Densitometric testing is aimed at assessing bone density and the effectiveness of osteoporosis therapy;
- Electroencephalography detects functional disorders in the hypothalamic-pituitary system that are amenable to drug therapy.
- Computed tomography and magnetic resonance imaging are used to identify organic pathologies of the brain that can trigger ovarian wasting syndrome.
If other pathologies are detected in a woman (endocrine disorders, metabolic disorders, anomalies and injuries of the genital organs), the doctor may prescribe additional examinations and consultations with specialized specialists - a reproductive specialist, an endocrinologist, etc.
Take the first step
make an appointment with a doctor!
Consequences of premature ovarian failure
First of all, a deficiency of estrogen in the body leads to osteopenia. Osteopenia is a decrease in bone mineral density. Subsequently, osteoporosis develops, a progressive systemic metabolic disease that affects connective tissues. A predisposition to brittle bones and fractures is associated not only with the disease, but also with taking medications, a sedentary lifestyle, and smoking.
Osteoporosis
Malfunction of the ovaries leads to a lack of ovulation, which jeopardizes a woman’s reproductive function. Since recently there has been a trend towards late childbirth, many people decide to have a child after 35 years. Ovarian dysfunction is not a death sentence. With the correct diagnosis and treatment of the disease, the possibility of a normal pregnancy and childbirth remains possible.
Treatment of congenital absence of ovaries
- Hormone replacement therapy.
- ECO.
Treatment is prescribed only after confirmation of the diagnosis by a medical specialist.
Essential drugs
There are contraindications. Specialist consultation is required.
- Somatropin (anabolic, growth-stimulating drug). Dosage regimen: subcutaneously, at a dose of 0.07–0.1 IU/kg or 2–3 IU/m2 per day, once daily at night.
- Conjugated estrogens (estrogenic agent). Dosage regimen: orally, at a dose of 0.3 mg/day. for 1 appointment. The course of treatment is 3–6 months.
- Dydrogesterone (progestin agent). Dosage regimen: orally, at a dose of 10–20 mg/day. for 1-2 doses.
Diagnosis and treatment of premature ovarian failure
The diagnosis of ovarian insufficiency (hypofunction of the ovaries) is made on the basis of the clinical picture of the disease, the results of studies on hormone levels, gynecological and general medical examination of the patient. An ultrasound examination is performed to determine the size of the ovaries, the presence or absence of follicles, and the general condition of the genital organs.
The treatment regimen is determined individually, taking into account the symptoms of the disease, test results and the presence of concomitant pathologies. The basis of treatment for premature ovarian failure is the use of hormonal medications as part of the so-called HRT - hormone replacement therapy. HRT involves the introduction into the body of hormones that are produced as a result of the work of the ovaries. Treatment should be carried out strictly under the supervision of a doctor.
Hormonal drugs
Recommendations for the treatment of concomitant diseases, which may also cause ovarian dysfunction, should be strictly followed. Especially such as: hypothyroidism, hypofunction of the adrenal cortex, systemic lupus erythematosus, Crohn's ulcer disease, type 1 diabetes mellitus. Complex therapy of the disease is necessary.
Experts recommend taking a complex of vitamins and minerals, as well as medications containing melatonin. Melatonin improves the functioning of the immune system, slows down the aging process, regulates the functions of the endocrine system, blood pressure, and sleep frequency. In addition, it is assumed. that melatonin prevents depression, restores fertility and the menstrual cycle.
You should pay attention to the woman’s mental state. Decreased mood may be associated both with fears for one’s health and with the desire of young women to have children. If necessary, appropriate treatment should be prescribed.
After adequate treatment of the disease, the work and secretory functions of the ovaries are restored. Young women have every chance of having a healthy child using in vitro fertilization.
After treatment, regular monitoring by a personal gynecologist is necessary. A woman is recommended to give up bad habits, switch to a proper sleep-wake schedule, and engage in moderate physical activity. By changing your lifestyle in favor of proper nutrition and avoiding stimulants, you can significantly improve the functioning of the endocrine and reproductive systems.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
If you find an error, please select a piece of text and press Ctrl+Enter
How to determine ovarian reserve
Women planning a child can assess the likelihood of conception by doing several tests:
- FSH analysis;
- AMS analysis;
- Ultrasound of the ovaries;
- Hormone tests: estradiol, progesterone, inhibin B.
FSH (follicular stimulating hormone) analysis
A test that measures the levels of follicle-stimulating hormone (also called follicle-stimulating hormone) produced by the pituitary gland. It is thanks to FSH that follicles mature.
FSH test
This hormone is found not only in the body of women, but also in men, so FSH analysis to diagnose infertility is carried out in both sexes. The FSH test in women involves drawing blood on day 3 of the cycle.
FSH level results are interpreted as follows:
- less than 3 mIU/ml – pituitary insufficiency;
- 3-9 mIU/ml – satisfactory ovarian reserve;
- 9-12 mIU/ml – low ovarian reserve;
- 12-18 mIU/ml – the supply is significantly reduced – the ovaries are practically depleted;
- above 18 mIU/ml – depleted ovarian reserve.
In women, in addition to diagnosing infertility, FSH can also help diagnose ovarian diseases such as polycystic ovary syndrome or other hormonal disorders, and determine whether a woman has entered menopause.
AMN analysis (concentration of anti-Mullerian hormones in serum)
AMH - analysis of the concentration of anti-Mullerian hormones in blood serum. This hormone is produced by the follicles surrounding the egg, and the fewer eggs there are, the lower its concentration. The test is carried out at any stage of the cycle.
Interpretation of AMH level results:
- above 3.0 ng/ml – high hormone levels, which may indicate polycystic ovary syndrome;
- above 1.0 ng/ml – normal level;
- less than 1.0 ng/ml is a low level that may indicate low ovarian reserve, including menopause.
Ultrasound of the ovaries with antral follicle counting
An ultrasound examination that determines the number of antral follicles that are ready to grow under the influence of natural gonadotropins produced by the pituitary gland or hormones administered during treatment. If there are less than 4 such bubbles, there is a small chance that you will become pregnant.
Ultrasound of the ovaries
Hormone tests: estradiol, progesterone, inhibin B
- Estradiol.
If the estradiol concentration test on cycle day 3 shows an E2 concentration of <75 pg/ml, this indicates low ovarian reserve or the presence of cysts. - Progesterone
. If the progesterone concentration test in the second phase of the cycle is ≤3 ng/ml, this means no ovulation. - Inhibin
B. This is a hormone produced by granular cells located in the follicle. A result below 45 pg/m (ng/L) on day 3 of the menstrual cycle indicates low ovarian reserve or menopause. In postmenopausal women, the result will be <10 pg/ml (ng/l).
Hormone tests