- What is breast MRI?
- In what areas is breast MRI used?
- How should you prepare for research?
- What does the diagnostic equipment look like?
- What is the basis for the research?
- How is the research conducted?
- What should you expect during and after the procedure?
- Who reviews the research results and where can they be obtained?
- Benefits and risks of breast MRI
- Limitations of breast MRI
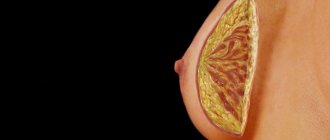
What is breast MRI?
Magnetic resonance imaging (MRI) is a non-invasive test that helps doctors diagnose and treat diseases.
MRI involves the use of powerful magnetic fields, high-frequency pulses and a computer system that allows you to obtain a detailed image of organs: soft tissues, bones and almost all structures inside the human body. The resulting images can be studied on a computer monitor, transmitted electronically, printed or copied to storage media. Ionizing (X-ray) radiation is not used in MRI.
Detailed images allow doctors to accurately assess the condition of various organs and systems and identify certain diseases that may be indistinguishable when using other examination methods, for example, X-ray, ultrasound or computed tomography. Breast MRI provides information about many diseases that is not available with other imaging techniques, such as mammography or ultrasound.
Up
Ultrasound or mammography - which is better?
To examine the mammary glands, methods such as mammography (classical and digital), breast examination using ultrasound (ultrasound) and MRI are currently used. How does breast ultrasound differ from mammography? What are the advantages and disadvantages of these techniques? What is better to do - a regular mammogram, digital or ultrasound of the mammary glands? Let's look at the advantages and disadvantages of each examination?
Conventional mammography or digital mammography – which is better?
Mammography is an examination of the mammary glands using x-rays. In modern medicine, two types of mammographs are used - classical and digital. The classic version of mammography is an X-ray of the mammary glands without the use of a contrast agent; the image of the mammary gland remains on film. This test is cheaper than digital mammography, which is becoming increasingly popular.
In Germany, mammography is performed only using a digital method, which has a number of advantages over film.
Digital mammography
An improved development of traditional X-ray mammography is digital mammography, which shows the image directly on a monitor. In this case, digital X-ray machines are used. The breast is not imaged on ordinary X-ray film, but on electronic phosphor screens or flat panel detectors. They transmit visual data directly to the computer. The computer then displays the images on a high-resolution screen.
Advantages of digital mammography compared to ultrasound
- The doctor can adjust the brightness and contrast on the screen, thereby improving image quality and presenting high-quality images.
- You can make multiple copies of an image.
- In addition, automated image analysis programs (called computer-assisted diagnostic systems) assist radiologists in evaluating images.
- Digital mammography has a lower radiation level.
- Digital materials can be archived electronically, processed and transferred to different medical institutions.
But this method also has disadvantages. Digital mammography is an expensive procedure, on the one hand, but on the other hand, it is less effective when examining young women with dense breasts, in the presence of implants, fibroadenomas, diffuse mastopathy and post-mastitis conditions. In this case, an ultrasound of the mammary glands is prescribed.
Mammography or ultrasound of the mammary glands - which is better and more accurate?
Ultrasound examination (sonography) of the breast does not cause any pain and does not involve radiation exposure. This is its big advantage. But most doctors consider ultrasound to be insufficient as the only test for early recognition of the disease, since ultrasound does not allow one to see small formations in the breast and it turns out that in some cases it is less informative compared to X-ray mammography.
When do doctors recommend breast ultrasound?
- Breast ultrasound is usually used as an adjunct to breast examination, for example in women with very dense breast tissue that cannot be assessed well with conventional mammography.
- When a mammogram reveals a suspicious result, the doctor may use ultrasound to check the accuracy.
- Under ultrasound guidance, a targeted biopsy of the breast or lymph nodes is performed. Ultrasound examination helps to navigate and accurately guide the needle to the right place.
- When a young woman under the age of 40 has symptoms indicating breast pathology, ultrasound is the method of choice.
- After the introduction of implants or reconstructive operations, ultrasound is used to monitor the intervention.
MRI mammography or X-ray mammography – which is better?
Imaging the breast in slice-by-slice images using MRI mammography (magnetic resonance imaging mammography) is now considered to be at least as informative as X-ray mammography.
Although MRI does not detect microcalcinosis, it very well shows the formation of new vessels around the cancer site. Thus, MRI, according to studies, detects as many or even more early-stage cancers than conventional mammography. The advantage of MRI mammography is that there is no radiation exposure and there is no compression of the breast during the examination. However, the examination lasts several minutes, during which the patient must lie on her stomach in the tube (this can be difficult if she is claustrophobic). Another disadvantage of MRI mammography: inexperienced researchers are more likely to see suspicious changes that lead to further research, but ultimately turn out to be a false alarm. In addition, MRI mammography is an expensive test.
So which is better – mammography, ultrasound or MRI of the mammary glands?
It is difficult to unequivocally answer the question of which is better, ultrasound or mammography, since each examination has its own pros and cons. Classic mammography allows you to see microcalcinosis, MRI mammography detects cancer in the initial stages, but mammography has contraindications associated with X-ray radiation, plus it is an expensive procedure. Ultrasound of the mammary glands may not show pathology of the milk ducts, but is more effective in identifying malignant tumors in young women and can be used at all stages of pregnancy, as well as during lactation. That is, all these studies complement each other, but do not replace each other.
Therefore, if you choose which method is better, it is advisable to listen to the opinion of the doctor who will prescribe the examination, taking into account your age and the purpose of the examination.
In what areas is breast MRI used?
Breast MRI is not a replacement for mammography or ultrasound, but rather complements these techniques in some important areas of medicine, such as:
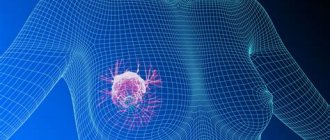
- Screening, that is, active examination, of women at high risk of developing breast cancer. MRI is a suitable diagnostic tool for evaluating women at high risk of breast cancer, especially those with a strong family history. A family history implies the development of breast cancer in the patient's mother or sister before the age of 50 years. They could also be cousins or aunts, including relatives with ovarian cancer. The family history is carefully reviewed by the radiologist or attending physician, who decides whether MRI should be used for screening purposes.
- Determining the stage of breast cancer after diagnosis. After a diagnosis of cancer, MRI of the mammary glands is performed for the following purposes: Determining the size of the tumor and its spread to the underlying muscles.
- Identification of other foci of cancer in the same mammary gland or previously undetected foci in the opposite gland.
- Detection of enlarged lymph nodes in the axillary region, which may be a sign of the spread of a malignant tumor to them.
Up
Alternative to mammography: a more accurate and gentle way!
Alternative to mammography: a more accurate and gentle way!
February 19, 2021
Despite advances in treatment and improved quality of diagnosis of breast cancer , this disease requires the scientific world to constantly move forward to improve treatment and diagnostic methods. Today, an alternative to the “gold standard” of screening has emerged – mammography. The new, gentle method makes it possible to precisely determine the presence and size of a tumor, after which it becomes possible to prescribe the most effective course of treatment. presents a modern diagnostic method and offers a German clinic where oncological examinations are already carried out at the highest level.
According to the American Cancer Society, mortality from breast cancer (BC) ranks first among cancer diseases in women. This is primarily due to late diagnosis and untimely referral of patients.
Currently, radiation diagnostic methods are mainly used breast cancer At the same time, the “gold standard” for breast cancer screening is mammography. However, this method is not informative enough and when used, about 10-15% of all cases of breast cancer .
MRI procedure is also uninformative because When imaging dense breasts, for example when undergoing screening on a specific day of the menstrual cycle or during treatment with hormonal drugs, it may not recognize cancer or give a false result of a multifocal lesion.
Scintimammography has been proposed to reduce the chance of error . A recent study of small breast tumors in 100 patients conducted in 2007 revealed the following sensitivity: tumor size <5 mm can be detected in 29% of cases, tumor size 6-10 mm - 86%, >11 mm in diameter - 97% .
Thus, scintimammmography is not effective enough in the early stages of the process.
often used to diagnose breast cancer , the main purpose of which is to predict the activity of the tumor, diagnose metastases, evaluate the effectiveness of treatment and identify local relapses. The sensitivity of PET in diagnosing multifocal lesions was twice as high as with the combined use of mammography and ultrasound (63% and 32%, respectively). The sensitivity and specificity of PET diagnostics for axillary lymph node metastases have also been reported to be 79% and 92%, respectively.
However, PET has limited sensitivity and is not suitable for detecting small tumors and well-differentiated breast cancer.
These problems can be solved by a specialized PET system – positron emission mammography ( PEM ). Unlike large PET systems that can scan the entire human body, a TEM system is small and is used to image a single breast. Externally, TEM resembles a mammograph. Just like with X-ray mammography, with TEM the mammary gland is fixed between two bars and slightly compressed for 10 minutes. The entire procedure takes about two hours, including administration of the radiopharmaceutical and rest. TEM produces sharp and detailed images of breast tumors ranging in size from 1.5-2 mm.
And this is not the only hybrid method that has emerged from PET. Currently, there are machines that combine PET with CT and/or MRI (PET/CT, PET/MRI, and PET/CT and MRI).
I found out which European clinic offers the most modern examination for suspected breast cancer . The University Hospital of Freiburg (Germany) has an Antitumor (Oncology) Center, where the most accurate methods for diagnosing this disease have been developed. It is also here that they use a gentle and effective technology for the treatment of breast cancer : doctors, using a special apparatus and special attachments, “burn out” the tumor during surgery.
You can find out all the details and get additional information about the new diagnostic method, as well as the German clinic and the possibility of organizing consultations and trips abroad, from our managers by contacting us in any convenient way or by calling our toll-free line: 8
Did you like the article? Share:
How should you prepare for research?
The nurse may ask the patient to wear a hospital gown during the examination. If the patient’s own clothes are loose, comfortable and do not have metal elements, then they are allowed to wear them.
Recommendations regarding food and fluid intake before a breast MRI depend on the characteristics of the examination itself, as well as on the preferences of the doctor. As a rule, the patient is allowed to maintain her usual daily routine and take food and medications in the prescribed order, unless the doctor says otherwise.
Because MRI may require contrast material to be injected into the bloodstream, the radiologist or nurse always asks the patient about any allergies, including to iodine or X-ray contrast materials, medications, food or environmental factors, and about the presence of bronchial asthma. However, MRIs typically use a contrast material such as gadolinium, which does not contain iodine and is less likely to cause any adverse or allergic reactions.
In addition, the radiologist needs to know about any diseases that the patient suffers from, as well as about recent operations. Some medical conditions, such as severe kidney disease, preclude the use of contrast in MRI. If you have renal pathology, before an MRI examination, you must take a blood test, which will allow you to evaluate your kidney function.
A woman should always warn the radiologist about the possibility of pregnancy. MRI has been used to evaluate patients since the 1980s. twentieth century, and there are no reports of negative effects on the body of pregnant women or their children. However, during the study, the woman's body, along with the fetus, is placed inside a strong magnet. Therefore, MRI should be performed in pregnant women only in cases where the possible benefits of the study outweigh the possible risks. In addition, the administration of contrast material is contraindicated for pregnant women.
If you have claustrophobia (fear of closed spaces) or severe anxiety, the patient may ask the doctor for a mild sedative before the test.
It is advisable to leave all jewelry and other decorations at home or remove them before the examination. Metallic and electronic objects are not allowed in the treatment room as they may affect the operation of the magnet. Such objects include:
- Jewelry, watches, credit cards and hearing aids that may be damaged during the examination.
- Pins, hair clips, metal lighters and similar metal objects that cause deformation of the MR image.
- Removable dentures.
- Pens, folding knives and glasses.
- Piercing.
In most cases, MRI is safe for patients who have metal implants in their bodies, with the exception of certain types. Persons with the following devices are prohibited from undergoing an MRI or being in the examination area, unless specifically authorized by a radiologist or technologist knowledgeable about the presence of the implant:
- Built-in pacemaker
- Cochlear implant
- Some types of clips that are used for cerebral aneurysms
- Some types of metal devices (stents) that are placed inside blood vessels
The presence of medical or electronic devices in the body must be reported to the radiologist, since these devices can interfere with the examination and carry a risk that depends on their type and the strength of the magnet. Examples of such devices include, but are not limited to:
- Artificial heart valves
- Installed ports for drug administration
- Installed electronic devices, including heart pacemaker
- Limb prostheses or metal joint prostheses
- Installed neurostimulator
- Metal plates, screws, pins, stents, or surgical staples
In general, metal objects used in orthopedic surgery do not pose any risk during MRI. However, recent joint replacement may require a different study. If the doctor doubts the presence of metal objects in the patient's body, then diagnostic radiography may be performed.
X-ray examination before MRI is also required for all patients with metal objects in certain parts of the body or organs. It is important to notify the radiologist or technologist if there are any bullets, shrapnel, or other metal that may have entered the body as a result of the accident. The inks used in tattoos may contain iron and become hot during an MRI. However, this rarely poses a serious difficulty. Fillings and braces are usually not affected by the magnetic field, but these elements can distort images during MRI of the head and face, so they should always be reported to the radiologist.
Up
How thermography works
Thermographic cameras capture heat radiating from the body. The result of the procedure is called a thermogram. Infrared thermography is a technology that converts infrared energy (radiated heat) into an image. Any substance in the Universe one way or another gives off heat in the form of radiation, the amount of this radiation increases with increasing temperature.
In other words, the infrared energy coming from an object is directly proportional to its temperature. Thermography analyzes changes in the patient's body surface temperature. However, it is worth understanding that the thermal radiation coming from the body is in no way related to the radiation during radiation therapy.
Thermography capabilities are applicable not only in diagnosing breast cancer, but also in examining the entire body. In addition to cancer, thermal imaging can help monitor changes in women with fibrocystic disease, infections, allergies and even cardiovascular disease that affect the health of the arteries. Thermographic cameras are used at airports to detect people who are sick or carrying weapons, by firefighters to detect smoke or civilians in distress, and by the military for surveillance.
One of the main advantages of thermography is its reliability (compared to other methods), as well as the possibility of early diagnosis of abnormal cellular activity and the development of tumors.
Thermographic images are precise and sensitive, and they detect even subtle changes in the body that may conceal illness. This is not an expensive procedure, it does not require surgery or exposure to radiation, which have a number of contraindications.
Here are some interesting facts about thermography:
- Thermal imaging is capable of identifying rapidly growing active tumors. The machine shows areas of heat that may indicate abnormalities, including breast cancer. The procedure may also be useful in assessing sensory nerve irritation, significant soft tissue damage, and locating the source of pain.
- Thermographic imaging records changes in body temperature due to blood flow and abnormalities caused by tumor development. During the diagnosis, both warmer and colder areas become visible, which may change over time. Since cancer cells grow and multiply very quickly, blood flow and metabolism, and therefore body temperature, are higher in these areas.
- Thermography is a non-invasive and inexpensive diagnostic method that does not involve radiation.
- Thermography may be particularly useful as a complementary diagnostic test along with other screening methods, such as mammography (which is generally not prescribed to women under 50 years of age). About 15% of breast cancer cases occur in women under 45, which means assessing the risk of the disease during this period is very important. Breast cancer in young women can be very aggressive.
- The result of the thermogram is different for each patient, so the “master” image is saved and used for comparison with other results of the procedure. Some experts compare a thermogram to a “thermal fingerprint”, since it is unique to each person and changes only if pathology occurs.
- Doctors compare the results of the thermogram to make sure that the image remains unchanged for several years, which means that no inflammatory processes occur in the patient’s body.
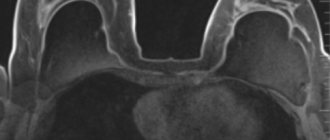
What does the diagnostic equipment look like?
A standard MRI machine is a large cylindrical tube surrounded by a magnet. The patient sits on a movable examination table that slides inside a magnet.
Some CT scanners (called short-tunnel systems) are designed so that the magnet does not completely surround the patient's table. Some devices are open on the sides. Such tomographs are especially suitable for examining obese patients and people who suffer from a fear of closed spaces. Modern open MRI scanners make it possible to obtain very high-quality images for various examinations. However, if an open type machine uses an old magnet, the image quality may be reduced. Some studies cannot be performed on an open tomograph. For more information, consult a specialist.
The computer working system that processes the images is located in the room next to the scanner.
Up
conclusions
The FDA said it is taking action to stop false advertising about thermography. Last week, it issued a warning letter to one company, Total Thermal Imaging, Inc., California, for marketing and promoting thermography devices that had not received marketing clearance or approval.
The Food and Drug Administration also ordered five other agencies to stop making inappropriate claims about thermography devices.
The authors of another study compared mammography and thermography.
What is the basis for the research?
Unlike traditional X-rays and computed tomography (CT), MRI does not require the use of ionizing radiation. Instead, the radio waves generated by the magnet change the direction of rotation in a powerful magnetic field of protons, which are the nuclei of hydrogen atoms.
In most MRI machines, a magnetic field is generated when an electric current passes through coils. Other wires located in the machine, and in some cases placed on the area of the patient's body that needs to be examined, send and receive radio waves. This generates signals that are picked up by sensors.
The signals are processed by a computer program, resulting in a series of images, each showing a thin section of tissue. The resulting images can be examined from a variety of angles by a radiologist. Often, MRI is the best way to distinguish pathologically altered, diseased tissue from healthy tissue than other imaging techniques, such as radiography, CT or ultrasound.
Up
Alternative research methods
Carrying out MRI of the mammary glands in the complex diagnosis of various diseases is advisable and desirable, since:
- MRI perfectly visualizes the soft tissues of an organ, much better than CT, radiography and ultrasound;
- MRI does not contain ionizing radiation, which is used in radiography and computed tomography;
- MRI scanning allows you to get the most complete and clear picture, unlike mammography, which is less informative;
- MRI makes it possible to study an organ both from the outside and from the inside (in ultrasound diagnostics it is only possible to assess the condition of the outer shell);
- MRI allows you to determine the presence of even small formations (unlike mammography).
The possibility of repeated repetition and the absence of negative effects on the woman’s body makes this type of research the most popular in modern diagnostics.
How is the research conducted?
MRI can be performed either on an outpatient basis or during the patient’s hospitalization. The radiologist's assistant places the patient on a moving table. The body position is secured using belts and special bolsters that help the patient lie still.
When performing an MRI of the mammary glands, the patient lies on her stomach, face down, on a platform specially designed for this procedure. The platform is equipped with holes for the mammary glands, which allows you to take pictures without squeezing them.
All electronic equipment required for image acquisition is already built into the platform. It is extremely important to remain still throughout the examination. The easiest way to achieve this is to sit on the treatment table as comfortably as possible and relax. Active muscle tension in order to maintain body position can only cause harm. It is important to notify the technologist or radiologist of any discomfort as any discomfort increases the likelihood of movement during the examination.
If an MRI is performed for the sole purpose of verifying the integrity or rupture of a breast implant, then the administration of contrast material is not required. In any other cases, intravenous administration of contrast is necessary. Breast MRI without contrast material cannot diagnose cancer.
If contrast is needed during the test, the nurse will insert a catheter into a vein in your arm. A bottle of saline solution may be connected to the catheter. The solution provides continuous flushing of the system, which prevents it from clogging before contrast material is injected.
After all preparations, the patient’s table moves inside the magnet, and the radiologist and nursing staff leave the treatment room for the period of the study.
If contrast material is needed, it is administered intravenously after the initial series of images. During or after the injection, the doctor receives an additional series of images.
After the examination is completed, the doctor asks the patient to wait until the analysis of the resulting images is completed, since an additional series of images may be required.
The intravenous catheter is removed.
A body MRI procedure typically consists of many sequences (series) of images, each taking several minutes.
The process of obtaining images of breast tissue generally takes from 30 minutes to an hour, and the entire procedure is completed within about an hour and a half.
During MRI, it is also possible to conduct magnetic resonance spectroscopy, which allows you to evaluate the biochemical processes inside cells. This study takes an additional 15 minutes.
Up
What should you expect during and after the study?
In most cases, an MRI is completely painless. However, some patients experience discomfort due to the need to lie still during the examination. Other patients may experience an attack of claustrophobia (fear of closed spaces). That is why the doctor offers sedatives for anxious patients, but in reality only 1 in 20 people need them.
During the study, a local increase in the temperature of the body area being examined is possible, and this is normal. However, if this phenomenon greatly bothers the patient, it is important to inform the doctor about it. It is extremely important that the patient lie absolutely still while the images are being taken (from several seconds to several minutes at a time). During some tests, the doctor asks the patient to hold her breath. The tapping or clicking sounds that the magnet makes as it produces high-frequency pulses help you know when image capture has begun. You can relax a little between series of shots, but you should still try to maintain your body position, without moving if possible.
As a rule, during the study the patient is alone in the treatment room. However, the radiologist can see, hear and talk to the patient at all times via a two-way communication system. The staff at many diagnostic centers allow relatives or friends of the patient to stay in the room until the test begins. However, they then need to go out to avoid exposure to the magnetic field.
The patient may be given headphones or earplugs to help suppress the loud knocking and humming of the scanner while images are taken. The patient has the right to ask for headphones herself. Children must be provided with headphones or earplugs of the appropriate size. The MRI scanner is air conditioned and well lit. Some centers play soft music during the examination.
When a contrast material is injected, there is normally a feeling of coolness or a rush of blood that lasts a couple of minutes. The patient experiences some discomfort when inserting and removing an intravenous catheter, which can leave hemorrhage under the skin. It is extremely rare that irritation occurs on the skin at the site of needle insertion. Some patients are bothered by a metallic taste in the mouth after injection of contrast material.
If the procedure was not accompanied by the use of sedatives, then a recovery period after it is not required. A return to normal activities and normal nutrition is possible immediately after the study. Some patients experience side effects when contrast is administered, such as nausea and local pain. It is extremely rare for an allergic reaction to the contrast material to occur, resulting in hives, itchy eyes, or other allergy symptoms. If you experience symptoms of an allergic reaction, you should inform your doctor. A radiologist or nurse will immediately provide the necessary assistance.
Manufacturers of contrast materials do not recommend breastfeeding for 24-48 hours after intravenous administration of contrast to the mother. However, experts from the American College of Radiology and the European Society of Urogenital Radiology report that research suggests that it is safe to continue breastfeeding after the use of intravenous contrast materials.
The American College of Radiology guidelines on the use of contrast materials state: “A review of the published literature indicates that oral administration by infants of small amounts of gadolinium-based contrast material that is excreted in breast milk does not cause any toxic effects. Therefore, we believe that after the introduction of such materials, continued breastfeeding is safe for both mother and baby. If the mother is concerned about the development of any unwanted effects, she should be given the opportunity to either continue breastfeeding after administration of gadolinium contrast or temporarily discontinue it. If the mother decides to stop breastfeeding for 24 hours after administration of the drug, then active expression of milk from both breasts is recommended during this period. Alternatively, a breast pump may be used before an examination using a contrast agent, which allows for enough milk to be fed to the baby for 24 hours after the procedure.”
Up
Who reviews the research results and where can they be obtained?
The images are analyzed by a radiologist: a doctor who specializes in performing radiological tests and interpreting their results. After examining the images, the radiologist draws up and signs a report, which is sent to the attending physician. In some cases, the report can be collected from the radiologist himself.
A follow-up examination is often required, the exact reason for which will be explained to the patient by the attending physician. In some cases, additional examination is carried out when doubtful results are obtained that require clarification during repeated images or the use of special imaging techniques. Dynamic observation allows timely identification of any pathological abnormalities that arise over time. In some situations, repeated examination allows us to talk about the effectiveness of treatment or stabilization of tissue condition over time.
Up
Benefits and risks of the study
Advantages:
- MRI is a non-invasive imaging technique in which the patient's body is not exposed to ionizing radiation.
- MRI has a proven diagnostic value for a whole range of diseases, including in detecting breast cancer and determining the stage of the tumor, especially when other imaging techniques are ineffective (mammography, ultrasound, etc.).
- MRI can detect pathological lesions hidden by bone formations and therefore invisible to other imaging methods.
- The contrast material used in MRI is much less likely to cause allergic reactions than the iodine-based contrast used in traditional x-rays and CT scans.
- MRI is becoming increasingly popular as a method of early diagnosis of breast cancer, along with traditional X-ray mammography.
- MRI has been shown to effectively detect small pathological lesions in the breast, which are sometimes not visible with mammography.
- MRI is successfully used to examine so-called dense breasts, especially in young women, as well as breast implants, where mammographic examination is often difficult
- MRI, in addition to mammography, has been shown to be successfully used in the evaluation of women at high risk of developing breast cancer.
- If a suspicious lesion is detected only on an MRI, it can be biopsied under MRI control.
Risks:
- If appropriate safety guidelines are followed, MRI carries virtually no risks for the average patient.
- When using sedatives, there is a risk of overdose. This is why the radiologist assistant carefully monitors the patient's vital signs.
- Despite the fact that the powerful magnet in the scanner itself is harmless, problems during MRI can arise if there are devices implanted into the patient's body that contain metals.
- When contrast material is injected, there is a very small risk of developing an allergic reaction. Such reactions are usually very mild and go away quickly when appropriate medications are prescribed. If allergy symptoms occur, a radiologist or nurse will immediately provide the necessary assistance.
- One recently described, but extremely rare, complication of MRI is nephrogenic systemic fibrosis, which develops when large doses of gadolinium-based contrast material are administered to patients with impaired renal function.
Up
Key tool in risk assessment
Early diagnosis of cancer greatly increases the likelihood of successful treatment. In fact, 95% of breast cancer cases are treatable if the disease is detected at an early stage.
Every year, more than 70,000 adult men and women ages 15 to 39 in America are diagnosed with cancer. Moreover, among women in this age group, breast cancer is the most common and most dangerous. Now doctors, as a rule, do not prescribe mammography for women under 50 years of age, so in 75% of women who do not have a family history of this disease, cancer is discovered too late.
Over the past 20 years, infrared thermography has proven its reliability; Doctors use ultra-sensitive, high-definition digital infrared cameras to detect heat spots in patients' bodies. Dr. Alexander Mostovoy from Thermography Clinic Inc. explains that the procedure is a 15-minute non-invasive examination without any pressure, radiation or contact.
Doctors may also perform a full body scan using thermography to look for signs of inflammation or pathology. If the thermogram shows pathology, the doctor will be aware of the changes that have begun in the body, which may subsequently lead to the development of oncology. If breast cancer is detected and then confirmed, the doctor can continue to more carefully monitor the progress of treatment and select the most effective therapy to combat the disease.