In medical terminology, metastases are secondary foci of growth (dropouts) of malignant tumors. Viable cancer cells, breaking away from the “maternal” tumor and penetrating the lumen of a blood or lymph vessel, move and settle in a new place. Then they begin to actively divide, forming a metastatic focus. The most extensive internal organ in terms of blood supply area is considered to be the lungs, which are one of the most common sites of tumor metastasis. In addition, various types of tumors have a tropism (craving) for the development of metastases in certain organs, most often such organs are, in addition to the lungs, the brain, liver, and bones.
Metastatic tumors
Modern oncology has information about a variety of primary malignant neoplasms that can spread, forming metastases in the lungs and other organs. This list includes:
- kidney cancer (16%);
- breast cancer (8.2%);
- colon cancer (rectum and colon) (14.3%);
- lung cancer (7.4%);
- bone sarcomas (24.1%).
In some cases, the primary tumor that triggered the screening of malignant cells remains unknown. Often, the process of metastasis does not make itself felt for a long time and is detected only during a diagnostic examination or at the very last stage of the disease.
Lung cancer and tuberculosis
If pneumonia is excluded, a differential diagnosis between lung cancer and tuberculosis is usually necessary. Similar symptoms are characteristic of infiltrative tuberculosis and peripheral cancer.
With tuberculosis, it is often possible to identify direct contact of a patient with a confirmed carrier of mycobacteria. Body temperature can be elevated in the evening and at night, up to subfebrile and febrile (unlike cancer, in which most often the temperature does not rise above subfebrile). During the oncological process, a localized dry cough is more often observed.
The course of tuberculosis is usually polysymptomatic, but the signs are weakly expressed, and in the oncological process, as a rule, 1-2 main symptoms can be clearly identified. When analyzing sputum, a pathognomonic sign will be the detection of pathogens of tuberculosis, and in case of cancer - atypical cells (in most cases). Also, a specific result will be given by subcutaneous tuberculin tests, which give a positive result for infection with mycobacteria, and a negative result for malignant lung tumors.
Radiologically, with tuberculous infiltration, you can see polysegmental darkening of a round or cloud-like shape, areas of bronchogenic contamination in remote areas of the lung or in another lung. With atelectasis (which often occurs in the central form of cancer), a bronchial stump is revealed; against the background of darkening, light stripes of the bronchial tree are not visible (unlike tuberculosis).
If we compare the cavernous form of tuberculosis with cavitary formations in cancer, then at first it is difficult to distinguish them radiologically - in both cases the cavern has thick, uneven walls with perifocal inflammation and infiltration, with the presence of fluid inside. After the necrotic masses are rejected, the walls of the tuberculosis cavity become thinner and smoother, the darkening itself is rounded (closer to the correct shape), and the infiltration around the formation decreases.
Difficulties may arise in the differential diagnosis of nodular peripheral cancer and tuberculoma. The latter has clearer, rounded contours, and the cancer has a specific radiance. Tuberculoma is characterized by areas of calcification and calcifications.
In any case, biopsy results are most often decisive for the differential diagnosis of lung cancer and tuberculosis.
Symptoms of metastatic lung disease
One of the most characteristic symptoms of metastases in the lungs is coughing. At first it can occur under the guise of prolonged bronchitis, then it becomes permanent, dry, hysterical and painful. Bloody streaks are often found in the sputum.
When a large part of the lung tissue is affected, compression or blockage of the bronchial lumen occurs, the accumulation of malignant pleural effusion (metastatic pleurisy) occurs. The patient experiences shortness of breath, the intensity of which depends on the volume of pathological fluid.
Sometimes the body temperature rises to subfebrile levels (37-38 °C) and remains there for a long time.
Lung cancer and pneumonia
Not so often, but still it is necessary to carry out differential diagnosis of peripheral lung cancer and focal pneumonia in clinical practice. The following symptoms are characteristic of the inflammatory process of pulmonary tissue of infectious origin:
- Pneumonia is more common in patients under 50 years of age (although it can occur at any age).
- There are no particular differences in the gender of patients (in cancer cases there are more male smokers).
- The onset of the disease in most cases is acute, with febrile fever.
- Shortness of breath may be absent, but with extensive lesions of the lung tissue it almost always appears (in oncology - in advanced cases).
- Pain may occur when the pleura is involved.
- Pronounced changes as a result of the use of physical diagnostic methods. Breathing especially changes: at first it becomes harsh, then dry and moist wheezing appears.
- When performing a general blood test, characteristic signs of inflammation can be identified (cancer in this case can be characterized by a high ESR with a normal leukocyte count).
- An X-ray image shows foci of inflammation of homogeneous density, more often in the lower lobes, with blurred boundaries, with an intensification of the pulmonary pattern and an increase in the roots of the lung.
Pathomorphology of metastatic nodes
Metastatic nodes that form in the lungs, in their density, are an almost complete reflection of the primary malignant neoplasm. Cancer cells delivered to the lung tissue through the blood or lymphatic fluid form metastases of various shapes.
By localization, metastatic nodes are unilateral and bilateral, and by number - solitary (single peripheral neoplasms), single (2-3 nodes) and multiple (more than 3 foci).
Depending on the effectiveness of the therapeutic effect in the treatment of primary cancer, metastases in the lungs are divided into:
- for those sensitive to radiation and chemotherapy (screenings of choriocarcinoma, osteosarcoma, ovarian and testicular cancer);
- partially amenable to conservative therapy (secondary foci of non-small cell lung and breast cancer);
- resistant to radiation and chemotherapy (screenings of melanoma, cervical, endometrial, colon, kidney cancer).
What pathologies have symptoms similar to lung metastases?
Lung cancer
— Solitary node
— Irregular shape
— Blurred boundaries
— Pleural spicules
Fungal infection
-Increase in size of lesions at a faster rate
— Fuzzy boundaries
— Background disease predisposing to the development of opportunistic infection
Rheumatoid nodules
— Usually solitary
— The disease that caused the formation of nodules is known
Primary pulmonary lymphoma
- Rarely seen
— Morphologically indistinguishable
Diagnosis of pulmonary metastases
Due to the fact that metastatic nodes are most often localized in the peripheral parts of the lungs, their identification is a rather difficult task. Comprehensive diagnosis of pulmonary metastases includes the following techniques:
- Plain radiography of the lungs in frontal and lateral projections. It is carried out to clarify the location and extent of the tumor, its interaction with the root of the lung and organs located in the mediastinum.
- Computed tomography of the chest with intravenous contrast. The technique makes it possible to determine the condition of the pulmonary root, clarify the nature of the metastatic process, detect small foci with a diameter of up to 10 mm and affected intrathoracic lymph nodes.
- MRI. Magnetic resonance imaging allows you to obtain sections of the lung parenchyma to identify structural changes and the exact location of the tumor. But this method is not very informative for lung damage.
- PET-CT (positron emission tomography). Used to measure the metabolic activity of lung tissue. Allows detection of active metastatic tumors in the lungs and other organs. It is the most informative method for assessing metastatic spread.
- Fiberglass bronchoscopy. This endoscopic technique makes it possible to assess the condition of the inner surface of the bronchi and take a biopsy sample of the tumor to make the most accurate diagnosis.
- Fine needle aspiration biopsy. Prescribed for suspected tumor formation in the peripheral parts of the lung. It is performed under the control of x-ray equipment.
- Thoracentesis (pleural puncture). It is performed in the presence of pleural effusion (if the malignant tumor affects the pleura).
Secondary formations are divided
• diffuse lymphatic; • nodular; • mixed.
Nodular form - solitary formations, round nodes with clear contours, which are located mainly in the basal region. In terms of growth rate and development characteristics, they are similar to the primary tumor. Focal form - small foci are found together with lymphangitis of nearby lung tissues, and clinical symptoms (dry cough, shortness of breath and general weakness) are observed in the early stages. Diffuse-lymphatic appearance - reveals itself by changes in the cord pattern, which on x-ray will be presented in the form of thin linear compactions. The spread of the malignant process contributes to the growth of tumor shadows. Such patients are given stage 4. Pleural form - similar to exudative pleurisy - the x-ray reveals tuberous-type layers and the presence of significant effusion. Malignant processes of the pleura are accompanied by deterioration of health, pulmonary failure and low-grade fever. Mixed form - in addition to node damage, it is manifested by lymphangitis and effusion of the pleural zone. Mediastinal nodes are often involved in the pathological process. These formations are called pulmonary-pleural.
For consultation on treatment methods, it is necessary to provide the following documents: discharge summary, results of histological examination, CT or MRI findings, information about previous treatment (if any).
Treatment of metastases
Not so long ago, when a metastatic process was detected in the lungs, only symptomatic therapy was carried out, designed to alleviate the patient’s condition. However, with the introduction of innovative equipment and new, more effective treatment and diagnostic techniques, oncologists have more opportunities to radically destroy secondary tumors.
Treatment of metastases in the lungs is prescribed taking into account the histological type of the tumor, the age and general condition of the patient, as well as the presence of concomitant diseases. To increase the effectiveness of therapy and reduce the risk of complications, smoking patients are strongly recommended to quit smoking.
Currently, the following methods of combating metastases in the lungs are used in clinical practice.
Surgical removal
Classic surgical treatment of metastases in the lungs is carried out only after resection of the primary tumor (or if it is possible to completely remove it). The operation is performed with a limited number of localized nodes, their accessibility to the surgeon, the absence of screening out cancer cells in other organs, and absolute confidence that the patient will tolerate the planned treatment.
Laser resection
This type of treatment is more often used for recanalization (restoration of patency) of a bronchus with a lumen blocked by a tumor.
Chemotherapy
This is the main type of treatment for multiple metastases in the lungs. When developing a chemotherapy treatment regimen, the nature and extent of the primary tumor is taken into account.
Radiation therapy
It is prescribed both for single lesions and for multiple ones (in rare cases). The possibility of application is determined by the morphological appearance of the primary tumor, its sensitivity to radiation exposure, location and size of the lesion.
Hormone therapy
The use of hormonal drugs is advisable for metastatic spread of hormone-positive cancer. The purpose of this technique is to influence the level of hormones that can stimulate the growth of malignant tumors.
Radiosurgery
Today, one of the most progressive methods of non-invasive treatment of single metastases in the lungs is stereotactic radiosurgery. During treatment, the Cyber-Knife radiosurgical complex is used, which exposes the tumor to high-precision, high-intensity radiation.
Using sophisticated software, the system consists of a specialized linear accelerator mounted on a robotic arm. It is capable of moving in 6 directions, providing exceptional flexibility, maneuverability and precision. The targeted use of CyberKnife photon radiation beams can relieve the patient of a metastatic lesion without prolonged irradiation and the use of surgical interventions.
This page contains only the text of the article. The full article with pictures and tables is here. Adobe Reader is required to view.Differential diagnosis of single lesions in the lungs
I.E. Tyurin, Doctor of Medical Sciences, Head. Department of Radiation Diagnostics, Radiation Therapy and Medical Physics RMAPO (Moscow)
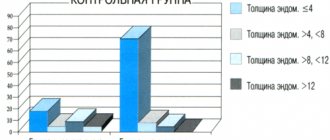
A solitary pulmonary lesion (SLP) is a relatively common radiological syndrome. In domestic and foreign literature, the term focus is defined differently. Such changes represent a local area of compaction of lung tissue of a round or similar shape with a diameter of up to 3 cm, surrounded on all sides by lung tissue. This international definition is somewhat different from the traditional domestic idea of pulmonary lesions, the source of which is TB practice. In the classification of tuberculosis, the size of lesions does not exceed 1 cm, and all larger lesions are defined as infiltrates, tuberculomas and other types of changes. The maximum size of a single lesion, equal to 3 cm, corresponds to the currently accepted staging scheme for non-small cell lung cancer, in which lesions of this size are classified as stage T1 of tumor growth. Lesions in the lung tissue can be single, isolated, ranging from 2 to 6 inclusive, and multiple. The latter refer to X-ray dissemination syndrome. They are usually considered in the context of differential diagnosis of interstitial (diffuse parenchymal) lung diseases. The main task of radiation research is the non-invasive differential diagnosis of malignant and benign processes, as well as the identification of individual forms of pulmonary tuberculosis among them. In some cases, this is possible based on characteristic symptoms detected by radiography or routine computed tomography (CT). However, the specificity of most of these signs is low, so additional methodological techniques and alternative technologies are necessary to correctly assess OBL. These include assessment of the growth rate of a lesion in the lung, analysis of probabilistic factors of malignancy [7], dynamics of accumulation of contrast agent in CT and 18fluorodeoxyglucose (18FFDG) in PET studies, as well as morphological assessment of changes based on the results of transthoracic needle aspiration biopsy or video thoracoscopy (VTS) . It is obvious that a single differential diagnostic algorithm intended for all patients and for all clinical situations is unlikely to exist in clinical practice. The goal of any clinical recommendations is to accurately assess the capabilities of individual diagnostic methods and their combinations. Detection Until now, the method of primary detection of foci in the lung tissue remains conventional x-ray examination in the form of radiography or fluorography. Single lesions are observed in 0.2–1.0% of all chest x-rays. Plain radiographs or fluorograms rarely reveal a single lesion less than 1 cm in size. Even larger lesions may be missed due to the interposition of anatomical structures (heart shadow, roots of the lungs, ribs, etc.) or the presence of so-called distracting factors, for example, developmental anomalies or heart pathologies. CT is becoming increasingly important in the diagnosis of pulmonary lesions, which can be performed both in cases of suspected presence of AOL based on radiography, and for other reasons, for example, excluding pneumonia, pulmonary embolism, assessing patients with COPD and emphysema, etc. In general, CT can detect 2–4 times more lesions in lung tissue than radiography, while the average size of detected lesions is half as large. However, CT is also not an absolute diagnostic method. The results of lung cancer screening using low-dose CT show that the main reasons for missing pathology are small lesion sizes, low density of ground-glass lesions and their localization in the central zones of the lung. Anatomical assessment Assessment of the skialological features of a single lesion according to radiography or CT is of great importance in differential diagnosis. The lesions can be divided by size, nature of the contours, structure, density, and condition of the surrounding lung tissue. Almost all signs have probabilistic meaning. those. more or less characteristic of a benign or malignant process. Only in exceptional cases can a nosological diagnosis be assumed on the basis of radiation examination data. Thus, the presence of fatty inclusions is typical for hamartoma, ring-shaped or total calcification of the lesion is usually observed in tuberculomas, the presence of afferent and efferent vessels with typical contrast enhancement distinguishes arteriovenous malformations. The localization of the lesion in the lung tissue is not of fundamental importance, since exceptions and coincidences are observed here too often. It is known that more than 70% of single lesions in peripheral lung cancer are located in the upper lobes of the lungs, more often in the right lung than in the left. This localization is typical for most tuberculous infiltrates. Lower lobe localization is typical for lung cancer arising against the background of idiopathic pulmonary fibrosis. Tuberculous infiltrates located in the lower lobes are more often localized in their apical segments. Lesions in the lung tissue can have different contours, including smooth or uneven (wavy, bumpy), as well as clear or indistinct (radiant or blurred due to the ground glass zone along the periphery). In general, fuzzy and uneven contours are more characteristic of malignant neoplasms, although they can also be observed with inflammatory infiltrates. When the lesion size is more than 1 cm, such contours are a strong argument in favor of the presence of a malignant process and, therefore, an indication for morphological verification of the process (Fig. 1). Clear, even contours can be observed in benign diseases, but are constantly observed in single metastases, certain histological forms of lung cancer (squamous cell, small cell) and pulmonary carcinoids. Therefore, the round shape and clear contours of the lesion in themselves are not signs of a benign process and cannot serve as a reason for completing the differential diagnosis process. The density of the entire area, determined by CT, allows us to divide all lesions into three groups: ground-glass lesions, mixed or partially solid lesions, and solid-type lesions. Ground glass lesions are characterized by low density; against their background, the walls of the bronchi, the contours of blood vessels and elements of the altered pulmonary interstitium are visible. They are observed in non-destructive inflammatory processes, atypical adenomatous hyperplasia and well-differentiated adenocarcinomas. Lesions of mixed or partially solid type are characterized by the presence of a denser area in the center and a low-density zone of ground glass type along the periphery. Such lesions usually arise around old scars in the lung tissue, including post-tuberculosis scars. In most cases, they represent the growth of a glandular tumor. Solid lesions have a typical structure of local compaction of a rounded shape of soft tissue density with various contours, which can be observed in almost any pathological process in the lung tissue. The structure of the pulmonary tract, detected by CT, can be different: homogeneous, with areas of low density caused by necrosis, with air, fat, liquid and high-density inclusions, with visible lumens of the bronchi. None of these symptoms are specific to any particular pathological process, with the exception of the already mentioned fatty inclusions in hamartomas. X-ray examination can reveal only part of the calcifications and air inclusions in the form of cavities, air cells (syn.: honeycombs, pores), observed, for example, with glandular carcinomas, or bronchial lumens. Calcifications in the primary area are detected with CT twice as often as with conventional X-ray examination (Fig. 2). Calcifications can be focal (like popcorn), layered, including the form of calcification of the lesion capsule, and diffuse, occupying the entire volume of the lesion (Fig. 3). Such calcifications are typical of benign processes. The only exceptions are metastases of bone sarcomas, metastatic foci of glandular cancer of the colon and ovaries after chemotherapy, and pulmonary carcinoids. In all other cases, the probability of a non-tumor process is extremely high. In malignant foci, including glandular carcinomas, dotted or amorphous, without clear contours, calcium inclusions are often detected. In general, the incidence of calcification in peripheral cancer tumors according to CT data reaches 10%, but in lesions less than 2 cm in diameter this figure usually does not exceed 2%. Such changes are visible only with high-resolution CT and are not a differential diagnostic sign, since they can also be detected in benign formations. Fat inclusions are commonly seen in hamartomas (Fig. 4). Areas of fat density can also be detected in primary lipomas, which are extremely rare, as well as in metastases of liposarcomas and glandular tumors of the kidneys. In the absence of extrapulmonary malignancy, the presence of fat in the pulmonary lesion is almost pathognomonic of hamartoma. Estimation of growth rate Comparison of the size of the primary tumor on previous photographs is of great importance in differential diagnosis. This comparison can be made using any images - fluorograms, radiographs, linear or computed tomograms. The absence of enlargement of the lesion for two or more years is one of the reliable signs of its benign nature. A significant portion of lesions in the lung tissue are missed in any initial study due to the skiological features of the pathology or psychophysiological factors of image perception. Therefore, analysis of previous images is the first and mandatory stage in the differential diagnosis of any AOL, and the presence of an image archive (for example, fluorographic) significantly increases the efficiency of radiation examination. It is obvious that malignant tumors increase in size at a greater or lesser rate, which is reflected in the images. The doubling time of tumors varies widely, from 40 to 720 days. Therefore, the appearance of a new lesion in the lung tissue within a month or a lesion with unchanged size for two or more years is unlikely to represent a malignant tumor, with the exception of ground glass lesions, which represent well-differentiated adenocarcinoma. Patients with these types of lesions require longer follow-up. Another factor limiting the possibilities of dynamic or retrospective observation is the size of the lesion is less than 1 cm. Doubling the volume of a tumor lesion measuring 5 mm leads to an increase in its diameter by 1.5 mm, to 6.5 mm. Assessing such dynamics is beyond the capabilities of not only traditional radiography, but also. in most cases, CT. In this regard, great importance is today attached to computer assessment of the volume of lesions based on spiral CT data, when a computer builds three-dimensional models of identified lesions and compares changes in their volume. This technique, which is part of CAD systems, is designed for solid lesions and cannot be used with confidence for ground glass lesions and partially solid lesions. Characteristics of lesions with dynamic CT Assessment of the blood supply to the peripheral tract with dynamic CT has shown its effectiveness in numerous studies. It is known that the density of the lesion in the lung tissue during native examination varies widely and does not have any diagnostic value (except for inclusions of fat and calcium). The meaning of dynamic CT is that with intravenous administration of a contrast agent in the form of a 100 ml bolus, pathological formations that have their own vascular network actively accumulate it, and their density increases (Fig. 5). A typical example of such lesions are malignant tumors. On the contrary, formations devoid of their own vessels or filled with avascular contents (pus, caseosis, exudate, etc.) do not change their density. Such lesions can be represented by tuberculomas, cysts, abscesses and other pathological processes. The dynamic CT technique for AOL is of greatest importance in regions with a high incidence of tuberculosis, since it allows one to accurately separate malignant tumors from tuberculomas. Dynamic CT is performed in the form of a series of tomographic slices through the pathological formation, which are performed before the administration of the contrast agent, during its administration, and 1, 2, 3 and 4 minutes after administration. To distinguish between benign and malignant processes, it is necessary to select the so-called amplification threshold, i.e. the numerical value of the attenuation coefficient, the excess of which suggests the presence of a malignant tumor. Since 2000, this threshold, empirically determined in a large multicenter study, has been 15 HU. Despite its high sensitivity for malignant tumors, the technique has a number of disadvantages. These include difficulties in assessing small lesions less than 1 cm, low specificity, technical errors associated with the patient's breathing and artifacts from bone structures and contrast media. These shortcomings are partially compensated by the introduction of multi-slice CT (MSCT) into clinical practice. In addition, most studies assessed the accumulation, but not the removal, of contrast from the lesions. Metabolic characterization of ALC with 18FDG PET All anatomical imaging methods, including X-ray, ultrasound, CT or MRI, are focused on macroscopic signs of pulmonary lesions, most of which are not specific enough. In recent years, studies of the metabolic characteristics of the lesion using 18FDG PET have become increasingly widespread. It is known that malignant tumors are characterized by higher metabolic activity, which is characterized by rapid and significant accumulation of 18FDG in the lesion and its long-term persistence. Numerous studies have shown that the method is distinguished by high sensitivity but relatively low specificity for malignant lesions in the lungs. Better results are obtained with the combined use of PET and CT scanners, the so-called PET/CT studies with subsequent combination of the metabolic and anatomical picture. False-positive results are observed in active inflammatory processes, including active pulmonary tuberculosis. A negative result of a PET study is considered extremely important in excluding the malignant nature of a pulmonary lesion. False negative conclusions can be observed in primary lung tumors of the ground glass type and in the presence of lesions less than 7 mm in size. In this regard, PET data must be compared with the results of CT studies for a more accurate understanding of their clinical significance. In general, it should be recognized that at present, PET examination is the most accurate method for distinguishing benign and malignant lesions in lung tissue larger than 1 cm in size. Biopsy For lesions that have anatomical or metabolic signs of malignancy, morphological verification is necessary before starting any treatment. This rule is mandatory, since the tactics of examination and treatment for primary non-small cell, small cell and metastatic tumors in the lung may be different. There are several methods for collecting material from a pulmonary lesion, including transthoracic needle aspiration and biopsy, transbronchial biopsy, VTS resection of the lesion followed by biopsy, and open biopsy during thoracotomy. Transthoracic biopsy is performed under the guidance of fluoroscopy, CT, and in recent years, increasingly under CT fluoroscopy. Transbronchial biopsy is usually performed under fluoroscopic guidance. Puncture of lesions adjacent to the chest wall can be performed using ultrasound guidance. Transbronchial biopsy can be performed when the lesion is localized in the hilar regions, especially in cases of so-called centralization of the malignant tumor. In this case, the endobronchial component can be detected during bronchological examination. Another verification option is a brush biopsy, in which material is taken from the inner surface of the bronchus located next to or inside the lesion. To carry out such a procedure, a preliminary assessment of the lesion and the adjacent bronchi using high-resolution CT is mandatory. Diagnostic algorithms Currently, there is no unified approach to determining the nature of ALE. Obviously, for patients with a high risk of malignant tumor, the optimal approach is the earliest morphological verification during transstorac biopsy. For patients with a low risk of malignant process, the observation and assessment of dynamics is more rational. In any case, the modern approach requires the performance of CT in cases of detection of ool during radiography, fluorography or ordinary CT of research. The second mandatory action is the search and study of any previous lung pictures. The result of these actions may be the release of a group of patients with an obviously benign process: the absence of dynamics for more than 2 years, the presence of “benign” calcification, turning on fat (gamartoma), fluid (cyst) in the focus according to CT data, for which only observation is necessary. This also includes the identification of AB malformation and other vascular changes, cases of inflammatory processes of the lungs, such as rounded tuberculosis infiltrate, tuberculoma, mitsetoma and others that require specific treatment. The second possible result is the identification of signs of a malignant process: a focus of more than 1 cm with radiant uneven contours, foci of the type of matte glass and mixed solid type, which should be regarded as potentially malignant, and for which morphological verification is necessary in the conditions of a specialized medical institution. All other foci are defined as intermediate or uncertain. The most large group among them is the first detected foci of more than 10 mm of soft tissue density, with relatively clear even or wavy contours, without any inclusions according to CT data and without the previous X -ray archive. Clarification of the nature of the focus in the lung tissue in such patients can be carried out using a biopsy, dynamic CT, PET and PET/CT research. Waiting tactics and prospective dynamic observation is permissible here only in exceptional cases, justified by clinical expediency. A separate group consists of patients with non -coalcinated foci of less than 10 mm detected by CT. Typically, such foci are detected in CT examination of lungs in various clinical situations, for example, the exclusion of pneumonia or pulmonary, clarification of the nature of emphysema, difficulties of interpretation of x -rays, etc. Such foci are usually not visible with a regular X -ray examination, their verification using transstorakal biopsy is ineffective, the use of PET of the study is associated with a large number of false negative results. In addition, the probability of a malignant process in foci of less than 5 mm does not exceed 2%. In this regard, the following tactics are accepted. Foci of less than 5 mm do not require any dynamic observation. Such patients may recommend a conventional test study (FLG or CT) in a year. Foci of 5-10 mm in size require a control CT study with an interval of 3, 6, 12 and 24 months. In the absence of dynamics, the observation ceases. Any changes in the shape, size, the number of foci is an indication for the biopsy. Thus, the differential diagnosis of OOL is a complex clinical task, which in modern conditions is solved using various methods of radiation and instrumental diagnostics.
magazine "Polyclinic" 3(1) 2014 p.28
Diagnostics and treatment at PET Technology
The federal network of nuclear medicine centers "PET Technology" has extensive experience in conducting PET-CT scanning and radiosurgery using the CyberKnife system. We offer early diagnosis of cancer and a specialized course of treatment for many primary tumors and metastases. Also, to confirm or refute a questionable diagnosis, PET Technology offers its patients to use and receive an expert opinion from our oncologists.
operate in several regions of Russia. To receive an online consultation and make an appointment, you can contact our operator at the contact number, use the form on the website or request a call back.
Lung cancer and foreign body in the bronchi
In many cases, aspiration of a foreign body into the bronchus goes unnoticed by adults. In such situations, patients may undergo long and unsuccessful treatment for bronchial or lung cancer. After a foreign body enters, in most cases a convulsive cough occurs, which may go away. Fruit pits, seeds, pieces of plastic, when in the bronchi, become covered with granulation, which causes a chronic inflammatory process. Sluggish inflammation in this case is accompanied by a periodic rise in temperature, cough accompanied by the release of mucous or mucopurulent sputum, slight shortness of breath and chest pain without clear localization.
The radiograph clearly shows a metallic foreign body. Otherwise, one can only discern a vague darkening of the affected bronchus and an area of inflammation around it. Computed tomography will help differentiate a foreign body from cancer, especially if a large segment of the bronchus is obstructed. In this case, a diagnosis of obstructive pneumonitis is made and tactics for removing the foreign body while minimizing damage to the bronchial mucosa are considered.
Endogenous broncholitis, which is a calcified part of a lymph node that has entered the lumen of the bronchus as a result of bronchoglandular perforation, can easily be confused with central lung cancer. In the presence of broncholitis, patients present approximately the same complaints as with central cancer. Tomography performed in two projections will help differentiate these conditions.
Bronchoscopy also has diagnostic value. If the bronchiolitis is large, located in the lumen of the bronchi or partially located in the wall, then the endogenous foreign body can be visualized and removed. However, if bronchodilitis formed many years ago and is completely hidden by granulation tissue, then its removal is possible only if the dense fibrous membrane covering it is destroyed. This is fraught with severe bleeding, since during surgical manipulations there is a possibility of damaging the relatively large bronchial vessels passing directly through the connective tissue membrane.
If darkening is accidentally detected and there are doubts about the choice of diagnosis between central cancer and broncholitis, it makes sense to perform a bronchoscopy with a biopsy. If the oncological diagnosis is not confirmed, then in the absence of complaints from the patient, broncholitis can be left and, if necessary, anti-inflammatory therapy can be carried out.
Lung cancer and syphilis
Pulmonary syphilitic lesions occur in extremely rare cases, and the period from the manifestation of the disease and the appearance of such a complication can be 8 years or more. In the presence of a solitary large syphilitic gumma in the lung tissue, it is necessary to differentiate it from lung cancer.
The symptoms of the disease often do not correspond to the degree of damage to the lungs with syphilis - relatively normal general health can be combined with severe shortness of breath. The course of the disease is long, often asymptomatic. With pulmonary syphilis, there will be no small signs of cancer, which are often an additional criterion for making an oncological diagnosis. A long history of syphilitic illness should also be taken into account, especially if the treatment has been irregular and inadequate throughout the entire period.
Syphilitic gummas are small in size (miliary, from a pea to a hazelnut), mostly localized in the middle and lower lobes of the lung. The formations may have an inhomogeneous structure and disintegrate with the formation of cavities. The results of serological tests for syphilis and the effect of targeted treatment with iodine and bismuth preparations, as well as bicillin therapy, will be decisive in the differential diagnosis.
“Ground glass” for adenocarcinoma (cancer) of the lung
Based on the “ground glass” effect on a CT scan of the lungs, malignant neoplasms—lung cancer—are determined. Adenocarcinoma is the most common type of tumor; a significant “trigger” for its formation is smoking, heredity, and age (over 40 years).
Adenocarcinoma tumor is formed from glandular epithelial cells. On the tomogram it is represented by a single, usually small (from 2 mm) area of compaction of the “frosted glass” type. In some cases, the patient has several “frosted glasses” of a diffuse or diffuse mosaic type. Adenocarcinoma is presented in various morphological subtypes and requires dynamic monitoring.
Do not try to interpret the images yourself. Only a specialized doctor who has been trained and has the appropriate certificate can identify “frosted glasses” and give them a differentiated assessment.
“Frosted glass” on CT scan for tuberculosis

Foci of infiltration of the “frosted glass” type are also found in tuberculosis. It is caused by the bacterium Mycobacterium tuberculosis. It is believed that all adults over 30 years of age are carriers of mycobacteria in a “dormant” form. When the immune system is suppressed, tuberculosis bacteria can become active and the person will become ill.
In tuberculosis, CT scans of the lungs usually show multiple small (miliary) lesions disseminated throughout the lungs. Their concentration in a certain proportion is possible. There is often an infiltrate in the form of a “path” leading to the root of the lung. There is an increase in lymph nodes. It is possible to definitively distinguish tuberculosis from pneumonia based on the results of PCR diagnostics - a blood test for the causative agent of infectious pneumonia.