The volume of the thyroid gland is equal to the sum of the volumes of the right and left lobes; the isthmus is neglected. It is required to display a longitudinal and transverse image of the thyroid lobe in the plane of maximum section. Measure the length, height and width of each lobe. Most ultrasound machines calculate the volume of the thyroid lobe using the volume formula for an ellipsoid of revolution: Length*Height*Width*π/6, where π/6=0.523.
Studying cadaveric material, in 1984 Brunn calculated a correction factor that most accurately corresponded to the actual volume of the thyroid gland - 0.479 (instead of 0.523).
If the thyroid volume is greater than normal, it is hyperplasia, and if it is less than normal, it is hypoplasia. When the volume of the gland is at the upper limit of normal, the anteroposterior size of the isthmus is taken into account: if the isthmus is more than 3 mm before 10 years or more than 5 mm after 10 years, then the gland is considered enlarged.
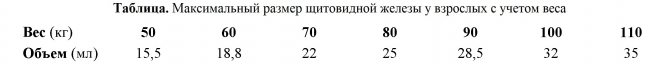
Thyroid gland size on ultrasound in adults
The maximum normal volume of the thyroid gland for women is 18-20 ml, and for men 20-25 ml. The minimum normal volume of the thyroid gland for women is about 4 ml, and for men - 7 ml.
Table. Maximum size of the thyroid gland in adults based on weight - printable
Size of the thyroid gland on ultrasound in children
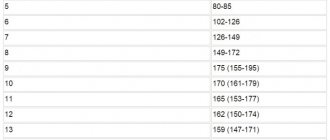
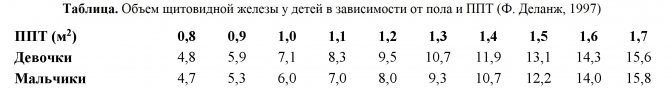
The minimum normal volume of the thyroid gland in children weighing up to 20-25 kg is 1.5 ml. The maximum volume of the thyroid gland depends on gender, age, puberty and body surface area.
In 1997, Professor Francois Delange calculated the maximum values (97th percentile) of thyroid volume in a group of 3 thousand children 6-15 years old living in iodine-sufficient areas of Austria, the Netherlands, Slovakia and France.
Table. The volume of the thyroid gland in children depending on gender and age (Delange, 1997) - for print
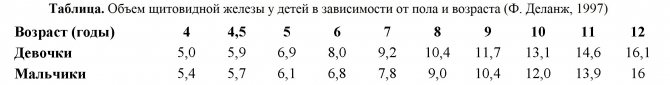
Table. The volume of the thyroid gland in children depending on gender and PPT (Delange, 1997) - for printing
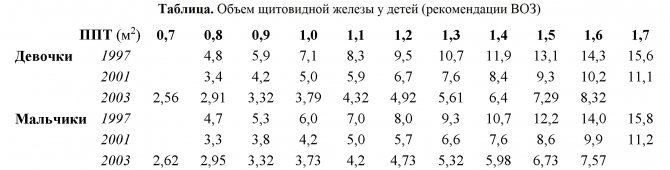
Below are the normal sizes of the thyroid gland in children depending on gender and body surface area according to the World Health Organization (WHO) for different years. Notice how the data differs from year to year. Between 1997 and 2003 there is simply an “abyss”! How to be??? The advanced Endocrinological Research Center of the Russian Academy of Medical Sciences uses the 1997 standards.
Table. Volume of the thyroid gland in children for ultrasound and endocrinologists (WHO recommendations) - for printing
The above standards do not take into account significant differences in the volume of the thyroid gland depending on the physical development of the child and the presence of puberty in the adolescent.
New approaches in the differential diagnosis of diffuse non-toxic goiter in children and adolescents
Ultrasound scanner RS80
A benchmark for new standards!
Unparalleled clarity, resolution, ultra-fast data processing, and a comprehensive suite of advanced ultrasound technologies to solve the most challenging diagnostic problems.
One of the pressing problems of modern clinical endocrinology is diffuse non-toxic goiter, the endemic prevalence of which among children and adolescents has reached in recent years from 5 to 40% or more in different regions of the Russian Federation [2, 3].
An ultrasound specialist who examines the thyroid gland in children and adolescents most often encounters in his practice diffuse euthyroid (non-toxic) enlargement of the thyroid gland. Therefore, he must always remember that this condition is not a diagnosis, but a universal pathological symptom of various diseases belonging to a heterogeneous group that unites individual nosologies. This group includes endemic goiter, which occurs mainly in response to chronic iodine deficiency, autoimmune thyroiditis, which is formed as a result of cellular and humoral autoaggression against antigens of the own thyroid gland in genetically predisposed individuals with innate characteristics of immunity, and familial sporadic goiter with dyshormonogenesis, appearing as a result of an inherited deficiency of one of the enzymes that are involved in the synthesis of thyroid hormones. The course, prognosis, outcomes and therapeutic approaches to treating these diseases are fundamentally different.
To select the most effective and safe treatment for diffuse non-toxic goiter in childhood, reliable differential diagnosis and identification of its specific nosological variant are necessary [3-5, 8]. The difficulty of making a differential diagnosis and clarifying the cause of goiter is associated with several factors. Firstly, the pediatrician catches the disease at its onset, when, unlike long-term ill adult patients, the child has not yet developed pronounced clinical and morphological changes in the thyroid gland, including according to ultrasound data. Secondly, the diagnostic efficiency of existing methods for recognizing this pathology remains low. Thus, one of the most important diagnostic symptoms of such a variant of diffuse non-toxic goiter as autoimmune thyroiditis is a serological assessment of the production of organ-specific autoantibodies to thyroid antigens: they are detected, according to various authors, in 29-79% of cases - to thyroglobulin and in 23-98 % - to microsomal antigen, i.e. not in all cases of the disease. At the same time, antithyroid antibodies are sometimes detected in non-immune pathology of the thyroid gland, and even in healthy children (in the form of subclinical antibody carriage) [7]. Previously popular scanning of the thyroid gland with radioactive isotopes has not found widespread use in pediatric thyroidology due to the increased sensitivity of the thyroid gland in children to ionizing radiation, as well as due to the low specificity of the scintigraphic picture for autoimmune thyroiditis in childhood. The most accurate method for diagnosing thyroid diseases remains a puncture biopsy with cytomorphological analysis of thyroid punctures [1]. However, this method is invasive, which introduces additional difficulties into the diagnostic search process in pediatric practice. Thus, existing methods for diagnosing diffuse non-toxic goiter in children and adolescents are either not specific enough or are unsafe for use in pediatrics.
Ultrasound is a non-invasive, highly accurate and cheapest method for diagnosing thyroid diseases. However, the existing criteria for diagnosing diffuse non-toxic goiter, firstly, are practically not developed for pediatric thyroidology, and secondly, the vast majority of them are subjective. At the same time, the emergence in recent years of new objective (quantitative) ultrasound techniques opens up new opportunities for their use in thyroidology [6, 8]. In this regard, the question of assessing the clinical significance of advanced ultrasound technologies in order to optimize the diagnostic search for diffuse non-toxic goiter in children and adolescents arises.
Materials and methods
To solve this issue, we examined 143 children - residents of Moscow - aged 6-16 years: 66 patients with Hashimoto goiter (a hypertrophic form of autoimmune thyroiditis in the euthyroid phase), 26 - with goiter of non-immune origin (25 - with endemic iodine deficiency goiter and 1 - with dishormonal goiter), 51 healthy children served as controls. In terms of gender and age composition, the main and control groups were comparable. In all cases, the diagnosis of the disease was verified by fine-needle puncture biopsy of the thyroid gland. The severity of each cytomorphological feature was assessed using a four-point system (from 1 - absence of a sign, to 4 - severe severity). Functional and immunological assessment of the state of the thyroid gland in various diseases and types of echographic picture included highly sensitive laboratory techniques: enzyme immunoassay of hormones of the thyroid complex (thyroid-stimulating hormone, free fractions of thyroxine and triiodothyronine) and specific antithyroid autoantibodies (to microsomal antigen and to thyroglobulin). For a more complete assessment of the ultrasound picture of the thyroid gland, in addition to traditional echotomography of longitudinal-oblique and transverse sections of the lobes of the organ under study, a complex of ultrasound techniques was used: echovolumetry, echotomography, echodensitometry, color Doppler mapping and pulse Doppler, which qualitatively and quantitatively reflect the degree of ultrasound changes in various types of echographic picture thyroid gland in children.
Research results
An attempt to involve a large arsenal of new ultrasound techniques when planning this study was associated with the hope of developing an algorithm for the differential diagnosis of diffuse non-toxic goiter in children and adolescents, based solely on the use of ultrasound imaging of the affected thyroid gland. Unfortunately, each of the methods individually and even their combination turned out to be unacceptable for solving this problem. Although the average parameters of various ultrasound techniques for endemic and autoimmune goiter differed, it was not possible to establish clear discriminatory thresholds and differential diagnostic criteria based on them (due to the large range of individual fluctuations). Therefore, optimization of the examination of children and adolescents with diffuse non-toxic goiter became possible only thanks to the improvement of the method of interpreting the results of traditional echotomography in close connection with the data of immunological and morphological studies.
In general, in healthy children and with various types of diffuse non-toxic goiter, we have established four types of echographic patterns (Fig. 1):
- unchanged thyroid gland - has a homogeneous fine-grained structure and normal echogenicity, comparable to its own parotid salivary gland. This type of echogram is typical for a healthy thyroid gland (n=51) and endemic goiter (n=25);
- slightly changed thyroid gland - characterized by the presence of small, different-sized (2-4 mm in diameter) hypoechoic round-shaped inclusions with clear contours of non-vascular origin against the background of normal structure and echo density of the surrounding tissue. This type of echogram was found in half of the patients with autoimmune thyroiditis (n=33), mainly in the early stages of the disease;
- altered thyroid gland - characterized by similar foci, but against the background of reduced echo density of the surrounding tissue. A similar type of echographic picture was also observed only in autoimmune thyroiditis - in almost a third of patients (n=19);
- sharply changed thyroid gland - hyperechoic inclusions of a point and/or linear (stringent) nature against the background of a general decrease in echo density and foci with an even more reduced echo density (of various sizes and shapes without clear contours). This picture, recognized as the “classical” description of Hashimoto’s goiter, was rarely detected in autoimmune thyroiditis in children (only in every fifth child, n = 14), and also occurred in the case of a non-autoimmune disease - Pendred’s goiter (n = 1; congenital defect organification of iodine, leading to the formation of hypofunction of the thyroid gland, the growth of diffuse goiter with subsequent nodular formation, which is combined with congenital sensorineural hearing loss).
Rice. 1.
Sonographic picture of various types of diffuse non-toxic goiter.
A)
Unchanged thyroid gland.
b)
Slightly changed thyroid gland.
V)
Changed thyroid gland.
G)
Sharply changed thyroid gland.
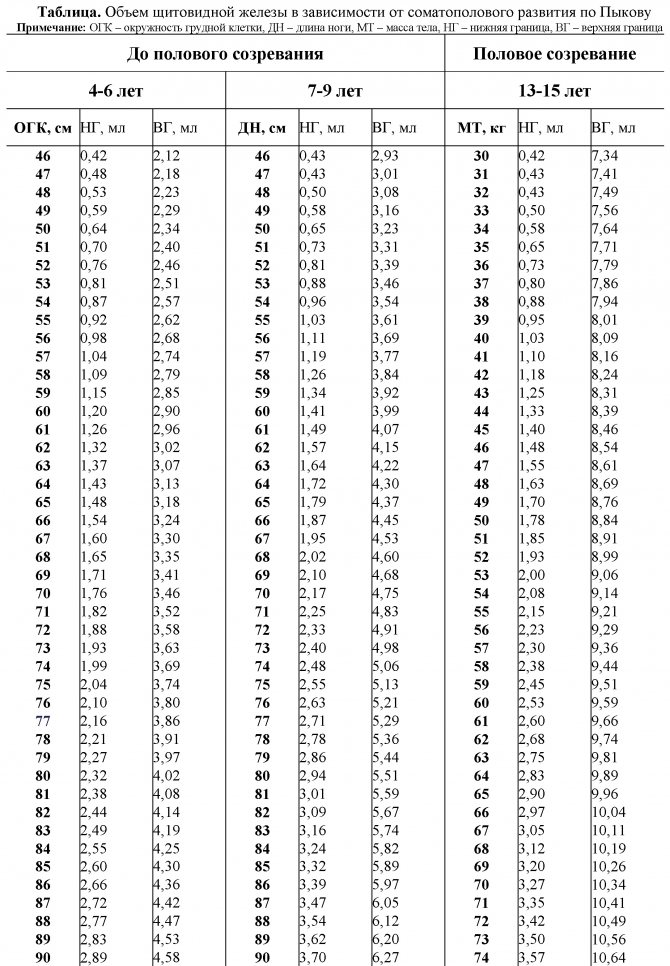
The size of the thyroid gland on ultrasound in children according to Pykov
M.I. Pykova is considered the main ultrasound expert on children in Russia. Calculation of the normal size of the thyroid gland according to Pykov was developed during an examination of more than 12 thousand children 4-15 years old living in a large industrial city (Moscow, Klin, Moscow region), rural areas of central Russia with moderate iodine deficiency (Moscow, Klin, Moscow region). Bobrov of the Voronezh region, the village of Kolpny of the Oryol region), as well as in five radiation control zones affected by the accident at the Chernobyl nuclear power plant (Valuiki and the village of Rovenki of the Belgorod region, the village of Repyevka of the Voronezh region, the city of Volkhov and the village of Naryshkino Oryol region).
Using the Pykov method, one of the anthropometric indicators (AP) is additionally measured. The upper and lower limits of normal thyroid volume (NVT) are calculated taking into account individual AP using the formula: NVT=APxI1-I2, where
- in children 4-6 years old: AP - chest circumference during exhalation; I1 0.056; I2 for the lower limit of the norm is 2.152, and for the upper limit of the norm is 0.456;
- in children 7-9 years old and children over 10 years old without signs of puberty: AP - leg length (distance from the greater trochanter to the sole); I1 0.076; I2 for the lower limit of the norm is 3.144, and for the upper limit of the norm is 0.566;
- in children 10-15 years old with signs of puberty: AP - body weight; I1 0.075; I2 for the lower limit of the norm is 1.976, and for the upper limit of the norm -5.088.
Table. The volume of the thyroid gland in children depending on somatosexual development according to Pykov - for print
conclusions
If the disease was detected in time and treatment began, then it does not have any serious consequences for the child’s life. As for congenital hypothyroidism in children, today's standards for examining pregnant women make it possible to identify dysfunction in its early stages.

Remember that signs of hypothyroidism in children can appear at 6 years old, 8 years old, 10 years old, and so on, so it is important to monitor your child’s condition and not neglect scheduled visits to specialists.
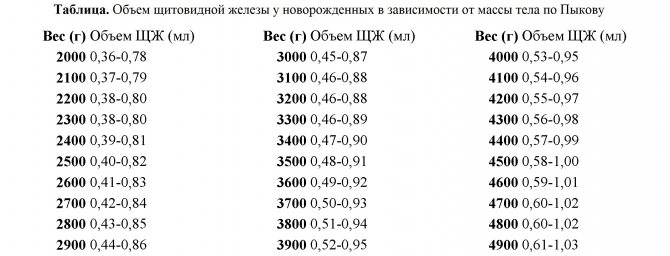
Volume of the thyroid gland on ultrasound in newborns according to Pykov
All cases of thyroid volume with values of 0.9 ml or more in the first week of life should be considered a sign of goitrous enlargement of the thyroid gland, and with values of 0.4 ml or less, a decrease in the size of the thyroid gland should be noted.
For accurate diagnosis of neonatal goiter and thyroid hypoplasia in a newborn, standards are used taking into account the child’s body weight: NTO (ml) = body weight (kg) x 0.088 + K, where K for the lower limit of the norm is 0.182, for the upper limit of the norm -0.602.
The analysis was carried out on two groups of children: 23 infants with neonatal goiter (boys/girls = 16/7) and 361 children (199/162) with normal thyroid volume.
Table. Thyroid gland volume (M+2σ) in newborns depending on weight according to Pykov - for print
Take care of yourself, Your Diagnosticer !
Tags: lectures, ultrasound standards, thyroid gland
Additional examination
When hypoplasia is detected for the first time, additional laboratory tests will be ordered. Researched:
- thyroxine;
- thyroglobulin;
- thyrotropin;
Hormonal status is primarily assessed by TSH levels. For patients with hypoplasia, an increase in the concentration of this hormone is most typical. Excess TSH indicates primary hypothyroidism. The severity of this condition is determined by the levels of T3 and T4. The combination of high TSH and normal thyroid hormones indicates subclinical (mild) hypothyroidism. If the concentration of T4 and/or T3 falls, then the disorder is considered quite pronounced (manifest). Based on the levels of TG and antibodies, the reasons for the decrease in the volume of thyroid tissue are judged. Congenital hypoplasia is not characterized by an increase in these indicators.