What is breast ductography?
Breast ductography is a method of x-ray examination of the milk ducts by artificially contrasting them (that is, introducing a special contrast agent into them). This method can also be called “galactography”.
Ductography is carried out to identify a number of pathologies of the mammary glands in the presence of specific signs of disease. This procedure is preceded by a cytological examination of the fluid released from the mammary gland. The complex of these procedures helps with a 96% probability to identify diseases such as intraductal papilloma, Mintz disease, intraductal cancer and others.
Is it painful to do ductography?
Breast clinics describe ductography as a painless diagnostic method. In fact, about half of the women who were diagnosed said it was painful.
When a contrast agent is injected into the nipple, pain may occur. Some people feel discomfort when performing this action, while others experience severe pain. Much depends on the individual characteristics of the female body and pain threshold. The further stages of the x-ray and completion of the examination are absolutely painless.
If the patient tells the doctor in advance about a low pain threshold or fear of the procedure, he may prescribe additional local anesthesia.
However, the pain associated with the use of contrast is secondary, so 95% of women tolerate it calmly. The doctor clamps the nipple, determines the location of the hole and inserts the needle. The amount of the substance is also determined individually; administration of 0.5 to 8 ml of contrast is allowed.
Indications
Almost every woman knows the procedure of mammography, which is an X-ray of the breast. It is often prescribed for preventive purposes and helps to detect dangerous pathologies in the early stages. Ductography may be prescribed for additional and more detailed diagnostics in cases where mammography has given controversial results or if the patient complains of frequent discharge from the nipples (there are other indications).
Discharge from the nipple of bloody or brown fluid (sometimes serous discharge)
Nipple discharge is normal when it occurs during pregnancy or lactation. If these factors are not present, but discharge is present, this should be a reason to go to a mammologist for examination and to identify the cause of the alarming symptom.
The discharge may be colorless, or it may have a specific shade - yellowish, greenish, brown or brown, red. The last two are the most serious symptoms, since most often these colors are caused by breast cancer, mastopathy or intraductal papilloma. The appearance of such discharge is explained by the fact that neoplasms appear in the milk ducts, which provoke the rupture of small blood vessels. Bloody discharge can appear directly when you press on the nipple or spontaneously.
Suspicion of intraductal papilloma
Intraductal papilloma, in addition to pathological discharge from the nipples, may have another symptom. On palpation, a large lump is felt in the area around the nipple. At the same time, on the periphery of the gland, compactions and outgrowths of the milk ducts are almost impossible to recognize. In this case, ductography of the mammary gland (breast) must be prescribed, since it is important to identify how far the disease has progressed, where the tumors are located and what their size is.
Suspicion of intraductal cancer
Intraductal cancer is one of the most complex and dangerous breast diseases. Dark-colored discharge from the nipples is a symptom of this pathology, but besides them, there are others: pain, redness, changes in breast shape, color and structure of the skin.
In this case, ductography is an event that will help determine the stage of oncology development, the localization of tumors, their size, structure, which in the future will help to correctly prescribe therapy or plan an operation.
Breast adenoma
Breast ductography is perhaps the most informative method for identifying mammary adenoma. The symptoms of this pathology are often not clearly expressed. When examined by a doctor
or during self-examination, an elastic formation with clear contours can be detected in the chest (sometimes there may be several such formations). The woman does not feel pain when pressing on the sites where adenomas form, and the skin of the breast does not change color or structure. In other words, ductography helps to identify a disease that is difficult to determine externally, by palpation, and even by mammography.
Breast cyst
Against the background of a hormonal imbalance in a woman’s body, as well as due to the lack of pregnancy, frequent abortions, cysts (one or more) may appear in the mammary gland (in the milk ducts). These are neoplasms filled with liquid contents. In the early stages of development, cysts are difficult to identify (they do not have clear symptoms), but with the help of ductography, mammologists receive fairly reliable information about the presence/absence of the disease.
Nodular or diffuse mastopathy
Nodular or diffuse mastopathy can develop together with existing fibrous mastopathy. Its symptoms are similar to those of many other pathologies of the mammary gland: neoplasms, thickening, increase in size, change in shape, pain on palpation, discharge from the nipple. In this case, ductography will help to accurately make a diagnosis.
What reveals
Experts consider malignant tumors in the mammary glands to be the most common cancer. Despite the simple diagnosis - it is enough to regularly take x-rays of the mammary glands (mammography), breast formations are often diagnosed in late stages. Ductography is considered a type of mammography, but this study is performed with a contrast agent.
Using a special device, the drug is injected into the milk duct through the nipple. Thus, all the milk ducts of the mammary gland are clearly visible on the x-ray. The ductography procedure is unpleasant and is associated with discomfort in the nipple area, although modern medical centers provide pain relief, but it allows the doctor to accurately determine the location of the tumor and preliminarily outline treatment tactics.
Using ductography, we determine:
- structure of the milk ducts of the mammary gland;
- location and shape of the formation in the chest;
- a possible cause of discharge (outside of lactation) from the nipples.
This information helps to make a prognosis for the course of pathology of the mammary ducts and the mammary gland as a whole. But this X-ray technique with contrast does not eliminate the need for further diagnostics.
Preparation for the procedure
Immediately before undergoing ductography, it is prohibited to massage the breasts or apply mechanical pressure to the nipples in order to avoid spasms of the milk ducts. Three days before the x-ray diagnosis, the patient should take an antispasmodic drug (the name and dosage are named by the attending physician).
It is necessary to carry out ductography between the 5th and 12th days of the menstrual cycle if the woman’s reproductive system has not entered the menopause stage. During menopause, ductography can be performed any day.
Disadvantages of analogue mammography
- The inability to change the characteristics of the image after taking an exposure. Film images cannot be resized. Digital mammography involves performing mammogram analysis from the monitor screen of a specialized workstation. This provides the radiologist with a wide range of digital image processing and analysis tools. Using functions for changing contrast, brightness, inversion, zoom, etc. allows you to present the mammogram in the most informative form, optimizing the diagnostic process. Special alignment functions make it possible to see tissue of different densities in one diagnostic image. In addition, digital mammography can compensate for inaccuracies in the selection of exposure conditions, minimizing the number of repeat images. New generation digital mammographs equipped with high-performance workstation processors allow you to manage large volumes of data with minimal time. When reading a mammogram, the radiologist can quickly query and retrieve data from the patient's previous studies from the archive to perform a comparative analysis. Workstations are usually equipped with 2 high-resolution monitors, on which a different number of projections can be presented in a convenient format.
- The capabilities of film images are limited when diagnosing small, low-contrast lesions. This is especially true for breast cancer against the background of dense parenchyma (with analogue mammography, such tumors cannot be differentiated from normal dense breast tissue).
- The complexity of selecting exposure, the labor-intensive process of developing film, and, as a consequence, the influence of the human factor. Storage facilities are required to store X-ray films. Special alignment functions make it possible to see tissue of different densities in one diagnostic image. In addition, digital mammography can compensate for inaccuracies in the selection of exposure conditions, minimizing the number of repeat images. Film mammography requires a bulky archive that must be stored for comparison in future studies. The results of digital mammography are stored in a computer database, which provides quick access and search for images. Digital technology ensures immediate availability of study results to the attending physician. The use of an electronic archive not only ensures convenient storage and prompt retrieval of diagnostic data, but also potentially eliminates the problem of lost or damaged images.
- Inability to use computer diagnostic programs. Mammograms can be extremely difficult for a radiologist to interpret. Digital images, unlike conventional X-rays, can be transmitted over the network to other specialists in any medical centers in Russia and abroad.
- The radiation exposure of digital mammography is approximately 25% higher than that of film mammography.
Contraindications

Like any medical procedure, this diagnostic technique has a number of limitations. Let's consider the main contraindications.
Absolute
Absolute contraindications serve as a reason to refuse diagnosis and not carry it out under any circumstances, except for a direct threat to life.
Pregnancy
Breast ductography is contraindicated in pregnant women. In addition to the fact that the image will be uninformative, since the milk ducts will be filled with liquid in any case, the woman will receive a dose of ionizing radiation (albeit small, but capable of harming the unborn baby).
Lactation
The explanations for this contraindication are the same as in the previous case - lack of information and the negative impact of radiation (in this case, on the composition of the secreted milk).
Acute inflammation of the breast (abscess, mastitis, etc.)
The introduction of a contrast agent into the milk ducts can worsen a woman’s condition if her mammary gland is inflamed (for example, mastitis, mastopathy, etc. are diagnosed). In addition, without anesthesia, contrast injection may be accompanied by severe pain.
Relative
Relative contraindications leave the possibility of diagnostics, but impose serious restrictions.
Allergy to iodine
Since the contrast agent contains an iodine component, ductography is not recommended for patients who are allergic to iodine.
Palpable formation in the excretory duct area
Breast ductography may be contraindicated if a neoplasm is detected during palpation of the breast. This may interfere with the injection of contrast into the milk ducts.
Breast punctures. Types, indications, cost
A puncture is a puncture of the breast tissue. A small number of tissue cells are collected from the puncture to determine the cellular composition of the tissue (cytological examination). It is carried out when nodular formations in the mammary glands are detected by ultrasound, mammography or palpation.
Palpable (determined by hand) formations are punctured without instrumental support.
Non-palpable (not detectable by hand) formations are punctured under ultrasound or x-ray control in order to most reliably take material directly from the node.
When puncturing cysts or liquid formations, liquid contents are evacuated from the cavity of the formation. This is not only a diagnostic, but also a therapeutic manipulation. Against the background of subsequent therapy, the empty cyst cavity grows together
Preoperative interstitial marking is the staining of an area of breast tissue before surgical treatment. It is carried out under the control of ultrasound or mammography for the most accurate and less traumatic surgical treatment. To do this, a special coloring marking substance is injected into the location of the tumor.
Our Center's mammologists perform all types of diagnostic and therapeutic puncture techniques. You can make an appointment with mammologists by calling: (495) 942-40-20 from 8.00 to 20.00
Interpretation of results
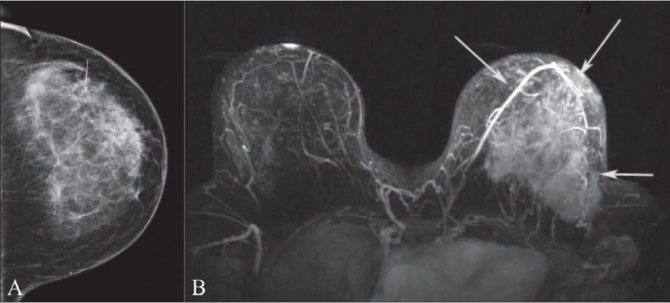
Ductography (what it is and how it is done, you can watch in the video) helps to visualize the ducts and their branches. In the pictures you can see tumors and determine their type - malignant or benign. Most often, ductography helps to recognize defects:
- filling of the milk ducts, indicating the presence of intraductal papilloma;
- milk ducts – short, rigid, dilated, with uneven contours or with neoplasms, these are signs of intraductal cancer;
- filling of the duct in the area of the contrasted cystic cavity is a sign of epithelioma of the cyst wall.
If it is not possible to administer a contrast agent because the excretory ducts are narrowed or swollen, we can talk about the patient having papillomatosis or mastopathy.
Benefits of analogue mammography
- Possibility of obtaining a polypositional image of the breast.
- The ability to visualize non-palpable formations with various manifestations: in the form of a node, in the form of a cluster of microcalcifications ranging in size from 50 microns, in the form of a local stringy restructuring of the structure, cancer inside the duct measuring 1-3 mm.
- Differential diagnosis of nodular and diffuse diseases.
- The ability to use a wide range of non-invasive and invasive techniques that simultaneously diagnose and treat a number of diseases.
- Carrying out ductography - artificial contrasting of the milk ducts with an accuracy of identifying the causes of pathological secretion in 96% of cases.
- The ability to carry out controlled puncture of cysts (pneumocystography) for diagnostic purposes and simultaneous sclerosis.
- Controlled puncture of pathological formations with the possibility of obtaining cytological and histological material.
- X-ray of the remote sector to assess the completeness of the surgical intervention.
- Preoperative interstitial marking of non-palpable formations.
- Assessment of the prevalence of the process.
- The ability to assess the condition of the second breast, which is extremely important for choosing the optimal treatment tactics.