- Factors that are associated with a low risk of developing ovarian cancer
- Symptoms of ovarian cancer
- Diagnosis of ovarian cancer
- Ovarian cancer treatment
- Surgical treatment of ovarian cancer
- Systemic drug treatment (chemotherapy) for ovarian cancer
- Monitoring of patients with ovarian cancer
- Prices at Euroonko for treatment of ovarian cancer
The etiology of the development of ovarian tumors, as for most human tumors, is completely unknown. But there are certain risk factors for developing this disease in women:
- Up to 10% of ovarian cancer cases are familial. The risk of ovarian cancer is increased if you have a relative with breast or ovarian cancer, especially if diagnosed during childbearing years. Genetic predisposition in women who carry BRCA1 or BRCA2 gene mutations. Therefore, if a genetic predisposition to the development of breast or ovarian tumors is suspected, a genetic examination is performed to determine the presence/absence of mutations in the BRCA1 or BRCA2 genes.
- Early onset of menarche and late onset of menopause are also thought to increase the risk of developing ovarian cancer.
Symptoms of ovarian cancer
The insidiousness of ovarian cancer is that in the early stages it is asymptomatic, or the symptoms are minor and patients do not pay attention to them. Most often, the first signs of ovarian cancer are detected when the process is already at stages 3-4.
The most common symptoms are:
- Pain in the lower abdomen. Usually this is a mild or nagging pain, often one-sided, which goes away on its own for quite a long time.
- Feeling of heaviness in the lower abdomen.
- An increase in the volume of the abdomen, the appearance of areas of “hardening” in it.
- Impaired urination and difficulty in bowel movements. This is due to the pressure of tumor masses on the wall of the bladder or rectum. Because of this, there is a frequent urge to urinate, constipation, a feeling of incomplete emptying of the bladder or intestines, and bloating.
- Metastasis of the tumor through the peritoneum leads to the development of ascites (accumulation of fluid in the abdominal cavity), which is accompanied by an increase in abdominal volume, general deterioration of health, shortness of breath, inability to eat or a feeling of fullness from a small amount of food.
- In the last stages, general symptoms characteristic of a malignant process appear - weight loss, even cachexia (exhaustion), deterioration of general condition, severe weakness, etc.
Causes and risk factors
Risk factors for ovarian cancer include:
- Late labor or absence of childbirth in a woman.
- Illiterately selected OK. The same applies to cases when oral contraceptives are selected correctly, but are used for other purposes.
- Menopause.
- Age 45-50 years.
- Long-term treatment for infertility.
- Some gynecological diseases - cysts, fibroids, etc.
- Bad heredity.
- Bad habits.
- Severe weakening of the immune system for various reasons - physical, stress, etc.
Women who have several such factors should monitor their health even more closely.
Diagnosis of ovarian cancer
Transvaginal ultrasound (trusound) and determination of the CA 125 marker in blood serum are used as diagnostic methods. The combination of these two methods has high specificity for diagnosing ovarian cancer.
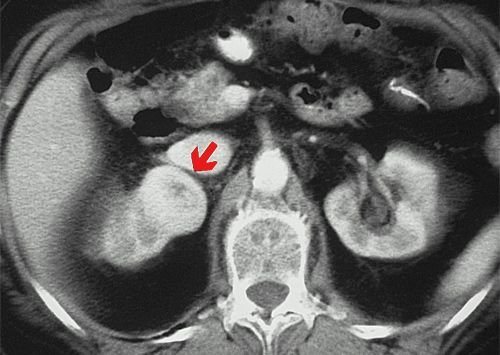
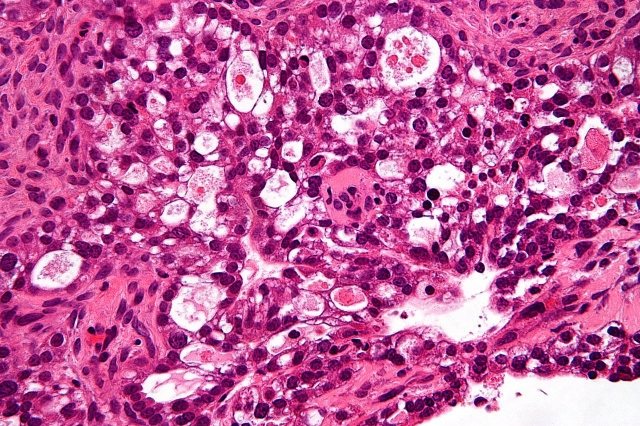
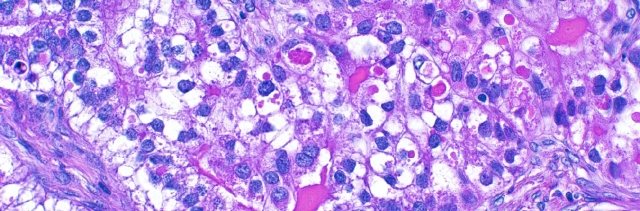
Additional research methods such as magnetic resonance imaging (MRI) or positron emission tomography (PET) can provide additional information, but are not necessary studies in routine practice during preoperative preparation. If the results of TRUS are questionable, the use of MRI can help us in correctly diagnosing ovarian tumors (malignant/benign tumor). The final diagnosis of ovarian cancer is made only after a morphological (examination of cellular/tissue composition) examination.

CA 125 (carbohydrate antigen 125) is the main marker of ovarian cancer. Normal levels in blood serum are up to 35 IU/ml. In most cases of ovarian cancer, its concentration increases 5 times or more. The concentration of CA 125 in the blood serum can also increase in various non-tumor diseases: inflammatory changes in the abdominal cavity, pelvis, menstruation, benign tumors of the female reproductive system (ovarian cysts). However, in most of these cases, the concentration of CA 125 in the blood serum does not exceed 100 IU/ml.
Follow-up and control
Treatment for people diagnosed with cancer does not end when active therapy is completed. Your doctors will continue to check to see if the cancer has returned, monitor any side effects, and monitor your overall health. This is called follow-up.
Experts recommend pelvic examinations every 2-4 months for the first 4 years after treatment, and then every 6 months for the next 3 years. For all three types of cancer, follow-up may include x-rays, CT scans, MRIs, ultrasounds, and blood tests (CA-125 determination).
Women who have had ovarian/fallopian tube cancer have an increased risk of developing breast cancer, colon cancer, or Lynch syndrome (some types of ovarian/fallopian tube cancer).
Relapse control
One of the goals of follow-up is to monitor relapse. The cancer process resumes due to the fact that small areas of undetected cancer cells may remain in the body. Over time, the number of these cells may increase until they appear on test results or cause abnormal signs.
Monitoring long-term and delayed side effects
Long-term side effects may persist after the treatment period. Other side effects, called delayed ones, may take months or even years to develop.
Discuss with your doctor the risk of these side effects depending on the type of cancer, your individual treatment plan, and your overall health. If your treatment is known to cause some late effects, you may need to have certain physical examinations, scans or blood tests to detect and treat them.
Maintaining your own medical records
You and your doctor will work together to develop a personalized follow-up plan. Be sure to discuss any concerns about your future physical or emotional health.
Surgical treatment of ovarian cancer
The goal of surgical treatment is to remove as much of the primary tumor and its metastases as possible. The operation that is preferred for ovarian cancer is extirpation of the uterus and appendages and resection of the greater omentum (i.e. complete removal of the uterus, fallopian tubes and ovaries on both sides). For patients who want to preserve reproductive function, it is possible to perform unilateral removal of the appendages with adequate staging and no changes in the preserved structures.

For ovarian cancer, there is such a thing as cytoreductive surgery, an operation that is performed to reduce the volume of the tumor. It can be optimal (when the volume of the residual tumor does not exceed 1 cm in the greatest dimension) and non-optimal (the volume of the residual tumor is more than 1 cm). For patients who did not undergo maximum cytoreduction at the first stage, it is possible to perform an intermediate cytoreductive operation if there are positive dynamics or stabilization during chemotherapy.
Make an appointment with an oncologist-gynecologist
Diagnostics
Suspicion of ovarian cancer requires a comprehensive comprehensive diagnosis, which includes the following:
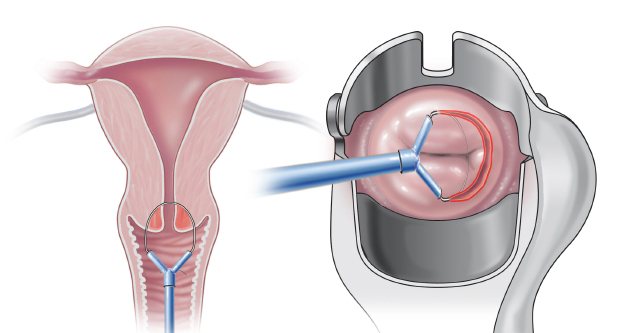
- Examination by a gynecologist, colposcopy, palpation of the abdomen, rectovaginal examination.
- Transvaginal ultrasound, CT and MRI of the pelvis.
- Laparoscopy for diagnostic purposes. It is needed to do a biopsy - to take a piece of the tumor for laboratory testing, as well as materials for a number of other tests.
- Blood test for different types of tumor markers.
- Studies to exclude metastases. This group includes mammography, X-rays of the lungs and stomach, ultrasound of the abdominal and pleural cavity, thyroid gland, FGDS, and various intestinal studies.
Clinical guidelines for ovarian cancer suggest undergoing a large number of procedures - but this is necessary, especially since the disease is often discovered when it is actively developing.
Systemic drug treatment (chemotherapy) for ovarian cancer
For ovarian cancer, different chemotherapy options can be used depending on the stage of the disease.
Neoadjuvant chemotherapy is preoperative chemotherapy for patients who cannot undergo surgical treatment at the first stage. When the desired effect is achieved, the patient subsequently undergoes surgical treatment.
Adjuvant chemotherapy is postoperative chemotherapy, carried out in the postoperative period in patients depending on the stage of the disease; in the early stages it is carried out in patients with intermediate and high risk (determined by the attending oncologist depending on certain characteristics).
Curative chemotherapy is carried out in the case of initially widespread disease or the presence of relapse of the disease.
When the disease relapses after previously administered platinum-based chemotherapy, attention is paid to the time from the end of treatment until the relapse occurs. If less than 6 months have passed since the end of chemotherapy or a relapse occurred during chemotherapy, the tumor is considered not sensitive to platinum drugs (platinum-resistant), and these drugs are not used in further treatment. Chemotherapy for patients with platinum-resistant disease is usually characterized by low antitumor effect and short life expectancy.
If 6 months or more have passed, the tumor is sensitive to platinum drugs (platinum-sensitive). With the development of a stable and long-term effect after platinum-containing chemotherapy, there is a high probability of a repeated response to treatment regimens with platinum derivatives.
As first-line therapy (i.e., what is used first), in the absence of contraindications, combinations based on platinum drugs are used, for example, paclitaxel at a dose of 175 mg/m2 with carboplatin AUC6 every 3 weeks for 6 courses of treatment. Carboplatin can also be combined with gemcitabine, docetaxel, liposomal doxorubicin, but in accordance with European recommendations, the combination of carboplatin with paclitaxel is in first place in terms of evidence.
Treatment methods
“Standard of care” refers to the best known therapies. When deciding on a treatment plan, you are encouraged to consider clinical trials as an option. This is a study that tests a new treatment approach. Doctors want to know whether the new therapy is safer and more effective than standard treatment. Clinical trials are an option for treatment and cancer care at all stages of cancer. Your doctor can help you consider all your options.
Treatment Overview
When cancer is diagnosed, different doctors, called a multidisciplinary team, work together to create an overall treatment plan for the patient.
Treatment options for ovarian/fallopian tube cancer depend on several factors, including the type and stage of cancer and possible side effects. The woman's personal preferences, general health, or personal considerations, such as the woman's age and plans to have children in the future, are taken into account.
Sexual health and fertility issues
Women with ovarian, fallopian tube, and peritoneal cancer may worry about whether and how their treatment may affect their sexual health and fertility. These issues should be discussed with your healthcare team before starting treatment.
Surgery
A gynecological oncologist is a doctor who specializes in the treatment of gynecological cancer, including surgical and chemotherapy methods.
To find out if ovarian/fallopian tube cancer has spread, your surgeon will take lymph nodes and samples of tissue and fluid from your abdomen for tests. If surgery shows that the cancer has spread, the surgeon will remove as much of the tumor as possible. There are several options for surgical treatment of ovarian/fallopian tube cancer. The stage of the tumor determines the type of surgery.
Sometimes doctors perform 2 or more procedures during one operation:
- Salpingo-oophorectomy. The fallopian tubes and ovaries are removed. If both ovaries and both fallopian tubes are removed, it is called a bilateral salpingo-oophorectomy. If a woman wants to become pregnant in the future and has early stage cancer, there is a possibility of having the appendages removed on only one side. This operation is called unilateral salpingo-oophorectomy. In patients with germ cell cancer, it is often necessary to remove only the ovary containing the tumor, preserving the woman's ability to become pregnant.
- Hysterectomy. The operation is aimed at removing the uterus and, if necessary, surrounding tissue. If only the uterus is removed, it is called a partial hysterectomy. Total hysterectomy – removal of the uterus and cervix.
- Lymphadenectomy. The lymph nodes in the pelvic and para-aortic areas are removed.
- Omentectomy. Removal of the thin tissue covering the stomach and intestines.
- Cytoreductive/reducing surgery. This surgery is suitable for women with metastatic cancer. The goal of cytoreductive surgery is to remove as much of the tumor as possible. This may include removing tissue from nearby organs such as the spleen, liver, and part of the small or large intestine. This may involve removing part of each of these organs. The procedure may help reduce symptoms. It may also help improve the effectiveness of chemotherapy given after surgery to control remaining disease. If the tumor has spread beyond the ovaries, fallopian tubes, or peritoneum, doctors may use chemotherapy to shrink the tumor before cytoreductive or reduction surgery. This is called neoadjuvant chemotherapy.
Side effects of surgery
Surgeries cause pain and weakness. If a woman experiences pain, the doctor will prescribe appropriate medications. For several days after surgery, you may experience difficulty urinating and/or defecating.
Shortly after having her ovaries removed, a woman will experience menopausal symptoms, including hot flashes and vaginal dryness. The patient will no longer be able to get pregnant.
Drug therapy
Systemic therapy is the use of medications to kill cancer cells. These drugs are administered through the bloodstream to reach cancer cells throughout the body. Systemic therapy for cervical cancer is usually prescribed by an oncologist or gynecological oncologist.
Common systemic treatments include inserting an intravenous (IV) catheter into a vein using a needle or swallowing (oral) tablets.
For ovarian, fallopian tube and peritoneal cancer, the following types of systemic therapy are used:
- Chemotherapy
- Targeted therapy
- Hormone therapy
The patient may receive several medications at the same time. They may also be part of a treatment plan that includes surgery or radiation therapy.
Chemotherapy
This is the use of drugs that destroy cancer cells, preventing them from growing and dividing.
The regimen consists of a series of chemotherapy treatments. At the same time, the patient can receive either one drug or combination therapy of different chemotherapy drugs. Classification of treatment types:
- Neoadjuvant chemotherapy. This is the medical term for therapy given before surgery. Its goal is to reduce the size of the tumor before surgery. It usually begins after a biopsy so the doctor can determine where the tumor begins. Typically, 3 or 4 cycles of neoadjuvant chemotherapy are given before deciding on surgery, called interval surgery. Such treatment usually consists of carboplatin administered intravenously along with paclitaxel or docetaxel.
- Adjuvant chemotherapy. Prescribed after surgery to destroy residual cancer. For these cancers, the specific drug is usually carboplatin administered with intravenous (IV) paclitaxel or docetaxel. Adjuvant chemotherapy drugs can also be injected directly into the abdominal cavity. This is called intraperitoneal or "IP" chemotherapy. This approach may be suitable for women with stage III disease.
Side effects of chemotherapy
The side effects of treatment largely depend on individual tolerance and dose of the drug. They manifest themselves as fatigue, risk of infection, dyspepsia, and hair loss. Complaints go away after treatment is completed.
Possible side effects of chemotherapy include problems with concentration and memory. This phenomenon is sometimes called "chemical brain". Other negative consequences include infertility and early menopause. Very rarely, some drugs cause hearing loss or kidney problems.
Targeted therapy
This is a treatment aimed at the gene code of cancer cells, tumor tissue. Targeted therapy inhibits the growth and development of the cancer process, while simultaneously preventing the destruction of healthy tissue.
To find the most effective treatment, a specialist conducts diagnostic tests to determine various factors of the tumor. This helps doctors, if possible, select the most effective solution to the problem for each patient. About 20% of high-grade tumors have mutations in the BRCA genes. They are usually diagnosed at later stages. Other tumor mutations are less common.
BRCA mutations, even those found only in tumors and not in the blood, can enhance the effectiveness of certain classes of drugs, particularly poly(ADP-ribose) polymerase (PARP) inhibitors.
Other less common types of ovarian/fallopian tube cancer include serous, endometrioid, clear cell, and low-grade mucinous tumors. These tumors have multiple mutations, including BRAF, PI3KCA and PTEN, meaning targeted treatments may be possible.
- PARP inhibitors. They block an enzyme involved in repairing damaged DNA. By blocking this enzyme, the DNA inside cancer cells is less likely to be repaired, leading to cell death and possibly slowing or stopping tumor growth.
- Angiogenesis inhibitors. They block the action of a protein called vascular endothelial growth factor (VEGF). These drugs have been shown to enhance the cancer's response to treatment and slow the time it takes for the cancer to return. VEGF promotes angiogenesis, that is, the formation of new blood vessels. Tumor growth and spread require nutrients supplied through blood vessels, so the goal of antiangiogenic therapy is to “deplete” the tumor.
Maintenance therapy based on targeted therapy
This is the medical term for treatment aimed at reducing the risk of relapse. The drugs are used to “maintain” clinical remission, that is, a period without signs of disease after completing a course of chemotherapy. Targeted therapy is aimed at “maintaining” clinical remission in women in whom the oncological process turned out to be completely susceptible to primary chemotherapy, and the disease “went into clinical remission.”
Hormone therapy
May be used to treat some low-grade tumors if they come back. Hormone therapy drugs include tamoxifen and aromatase inhibitors. The treatment is suitable for eliminating stromal tumors such as recurrent granulosa cell tumor.
Radiation therapy
Not used as primary cancer care. It can sometimes be a treatment option for small, localized, recurrent cancers.
Radiation therapy is the use of high-energy X-rays or other particles to destroy cancer cells. A doctor who specializes in radiotherapy is a radiation oncologist. The most common type of radiation therapy is called external beam radiation therapy. In this case, the radiation comes from a device outside the body. When radiation therapy is given using implants, it is called internal radiation therapy or brachytherapy.
Negative effects may include fatigue, mild skin reactions, upset stomach, and loose stools.
Physical, emotional and social consequences of cancer
Cancer and its treatment cause physical symptoms and side effects, as well as emotional, social and financial consequences. Managing all of these effects is called palliative (supportive) care. Palliative care aims to improve your well-being during treatment by managing symptoms and supporting the non-medical needs of patients and their families. Palliative care is varied and often includes medications, dietary changes, relaxation techniques, and emotional and spiritual support. Chemotherapy, surgery, or radiation therapy may also be involved.
General information
Stages of the disease:
First stage. The tumor does not spread beyond the ovaries. The tumor is localized in one or both ovaries. At this stage, surgical removal of the tumor can be performed while preserving the ovary/ovaries.
Second stage. The tumor has grown outside the ovaries. The organs adjacent to the uterus are affected. At this stage, surgical treatment with preservation of organs is also still possible.
Third stage. The pathology extends beyond the pelvic organs and extends to the abdominal cavity. At this stage, malignant processes can begin in the lymph nodes. The spread of cancer makes a local surgical solution to the problem almost impossible.
Fourth stage. This stage is characterized by the appearance of metastases in organs distant from the ovaries, for example, in the liver, lungs, etc.
Prevention
Preventive measures for ovarian cancer include:
- Regular gynecological examination. Once every six months you need to go to an appointment with a gynecologist and treat all detected diseases in a timely manner. Once a year you need to do a gynecological ultrasound.
- Taking oral contraceptives. According to some reports, the risk of ovarian cancer when using them is reduced by 50%. But OCs are selected strictly individually after tests and consultation with an experienced doctor.
- Maintaining a healthy lifestyle, constantly strengthening the immune system.
- Timely examination if even not very obvious symptoms of ovarian cancer are suspected.
Treatment

When treating ovarian cancer, several approaches are combined:
- Surgical treatment. It comes in different types and volumes - it all depends on the stage and situation. Most often, the uterus is removed, as well as the fallopian tubes and adjacent ovaries. Often, removal of individual lymph nodes and more extensive interventions are required. In later stages, we are talking about inoperable tumors, so surgery is not performed.
- Polychemotherapy. It is carried out to prepare for surgery, after it, and also as an independent means of treatment if the process has already started and surgery is impossible.
- Radiation therapy. As a rule, it is not used in the treatment of ovarian cancer because it has little effectiveness.
After treatment, patients continue to be monitored by a gynecological oncologist in order to promptly detect relapses, if they occur, and other undesirable conditions.
Forecasts
Taking into account the type of tumor, five-year survival at the first stage is possible for 60-90% of patients, at the second stage - for 40-50%, at the third stage - for 11% and at the fourth stage - only 5%.
Treatment at the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency
- Diagnostic methods available to the gynecology department of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency are used in all international clinics, treatment and rehabilitation programs for patients fully comply with European and Russian treatment standards;
- The department uses the most modern and most effective pharmaceuticals that have been tested in the best clinics in Europe and America and have proven themselves in the world market;
- All types of operations for various types of gynecological diseases, including laparoscopic treatment, are performed at the Federal Scientific and Clinical Center FMBA.
Prevalence
Tumor lesions of the ovaries are most often diagnosed in women who have entered menopause and menopause. Although detection of a tumor in young patients is also not uncommon. In the structure of all oncopathology, malignant lesions of the ovaries are given 7th place, they do not exceed 4-6%. If you look at the structure of oncopathologies of gynecological localization, then in this classification ovarian cancer takes 3rd place. In terms of prevalence, it is ahead of oncological lesions of the uterine body and cervix.
Main symptoms
Clinical symptoms are extremely varied. In the early stages of the disease, symptoms usually do not appear. A sharp attack of pain occurs when the tumor stalk is twisted or its capsule ruptures.
As the disease progresses, tumor cells penetrate beyond the female reproductive glands. Patients experience rapid fatigue, muscle weakness, loss of appetite, various gastrointestinal dysfunctions, difficulty urinating, etc.
At stages III-IV, breathing becomes difficult, cardiovascular disorders appear, the legs swell greatly, the liver and bones are affected, and the risk of thrombosis is high. When tumor cells penetrate the peritoneum, ascites develops.
With granulosa cell oncopathology of the gonads, menstruation appears in menopausal women. Teenagers with the same form of ovarian cancer experience accelerated puberty. With adenoblastoma, uterine bleeding disappears, excessive hair growth appears, and the figure changes.
For successful treatment of ovarian cancer, it is necessary to identify the tumor in a timely manner, that is, consult a gynecologist in time.
Causes of ovarian tumors
The main causes of ovarian tumors today are the following:
- Hormonal imbalance. An increase in the hormone estrogen can provoke the formation of tumors of various origins. The risk group includes patients who either started menstruation too early or entered menopause too late.
- Hereditary factor;
- Chronic inflammatory diseases of the uterine appendages;
- Nutritional factors (these may include malnutrition, environmental level).