Ovarian hyperstimulation syndrome, what is it and how to avoid it?
Most women suffering from infertility have heard about ovarian hyperstimulation syndrome; fear of this complication of IVF often pushes women away from the program. Ovarian hyperstimulation syndrome (OHSS) is a condition based on the reaction of the ovaries in response to the administration of hormonal drugs (ovulation inducers), doses of which exceed physiological values. This condition was first described in 1930 using serum from pregnant mares.
Ovarian hyperstimulation syndrome is characterized by a fairly wide range of clinical manifestations: from minor changes in laboratory parameters to quite serious conditions requiring hospitalization.
The main reasons for its occurrence are high doses of hormonal drugs that are used to stimulate ovulation, as well as high levels of activity of the hormone estradiol, which is produced in growing follicles, and high levels of the hormone hCG. The main risk group for the formation of this syndrome are girls diagnosed with polycystic ovary syndrome, since this group has a high follicular reserve and a large number of follicles “come into growth” during induction.
Ovarian hyperstimulation syndrome is currently a well-studied syndrome; for this reason, reproductive specialists around the world are trying to perform ovarian stimulation using a minimal hormonal load, pursuing the main goal: to obtain the maximum number of mature and high-quality oocytes, to avoid ovarian hyperstimulation syndrome. All patients who are preparing for the IVF program undergo a thorough examination (in accordance with Order 107n of the Russian Federation), all possible risks are assessed by a reproductive specialist, and preventive measures are taken in the presence of risk factors for the occurrence of OHSS.
Women at high risk of developing the syndrome are recommended to undergo an IVF protocol followed by cryopreservation of embryos and embryo transfer in another cycle.
So, modern knowledge about the peculiarities of stimulation of patients with a high risk of hyperstimulation makes it possible to minimize cases of ovarian hyperstimulation through the use of minimal protocols and embryo transfer in an unstimulated cycle.
Limitations of using the IVF method
This technique has limitations. It should not be used frequently for the following reason: in the process of preparation for the procedure, the woman’s ovaries are hyperstimulated, which causes a hormonal imbalance; the body will be ready to repeat the procedure only after complete recovery.
The method is considered completely safe, but the success of its use is determined by several factors, including the characteristics of the body. The number of possible attempts can only be determined by a doctor. If the transfer is repeated, then previously obtained embryos are used. You can repeat the procedure six months after the previous unsuccessful replantation.
Cancer risks and IVF: myth or reality?
A lot of fears among our patients are caused by rumors about an increase in the risk of cancer after the program. Indeed, IVF is an intervention in the human body - exposure to hormonal drugs.
Does the program really increase the risk of various cancers: breast, ovarian, uterine, colorectal cancer, melanoma, etc. or is this an unfounded fear? Scientists have been closely studying this issue for decades; as a result of their efforts, it was established that there is no pattern between ART and the occurrence of cancer.
Here are the results of international research in this area:
- According to one randomized study, including more than 100 thousand people and a follow-up period of 25 years, it was proven that the risk of developing ovarian and uterine cancer does not increase in patients after the program.
- According to the American Gastroenterological Association, a randomized study involving 20 thousand people with a follow-up period of 21 years also proved that there was no pattern in the occurrence of rectal cancer and the implementation of an IVF program.
- According to a large randomized study in Oxford (England), including more than 25 thousand patients, it was proven that IVF does not affect the risk of melanoma.
- According to many randomized studies (2010-2016), it was shown that there was no effect on the incidence of breast cancer in women after completing the program. The more “frequent” detection of breast cancer in this population group compared to other women is associated with careful examination and follow-up, early detection of the disease in women of the older age group who have a genetic predisposition to its occurrence. Moreover, one of the risk factors for breast cancer is infertility. This is also worth remembering.
- Moreover, a history of cancer is currently not a strict contraindication for ART, as it was before. Each case is discussed at a consultation of doctors, where the optimal tactics for managing the woman are determined.
Thus, hormonal drugs used in ART do not provoke the development of cancer. However, in underexamined women with the presence of precancerous diseases, their own increased background of endogenous hormones can activate an already existing process.
Will my child be “normal”?
One of the biggest concerns any pregnant woman faces is whether her baby will be “normal” or not? When it comes to IVF, concerns increase due to the introduction of an “unnatural” component into the equation, which can increase the likelihood of abnormal offspring.
Several studies have been published that demonstrate an increased risk of developing defects in children after IVF: Down syndrome (trisomy 21), Edward syndrome (trisomy 18) and Turner syndrome (monosomy X0). However, a careful analysis shows that most of the listed malformations are due to an increase in the average age of women entering the IVF program compared to comparable ages in fertile groups of the female population as a whole, and there is a connection between age and the occurrence of chromosomal abnormalities. For example, at age 30, a woman's chance of having a child with Down syndrome is approximately 1 in 1,000, while at age 40 the risk is approximately 1 in 150 and at age 45 it is 1 in 35. This occurs due to the “wear and tear” of the eggs over time.
Thus, the patient’s late reproductive age increases the risk of chromosomal abnormalities, both during spontaneous conception and after IVF.
Superovulation stimulation protocols
During in vitro fertilization, different types of protocols are used. It should be remembered that there are no strict treatment regimens; individual variations are possible for each of the protocols below.
"Clean Protocol"
Some women use stimulation regimens without blocking the pituitary gland. For this purpose, only drugs containing FSH are used, for example Puregon Pan. This scheme is called “pure”. Its disadvantage is the likelihood of premature ovulation (rupture) of the follicle even before puncture, which makes it impossible to obtain eggs. With this protocol, the administration of stimulant drugs begins on the 2nd–3rd day of menstruation and continues for 9–14 days. The daily dose is adjusted by the doctor depending on the ultrasound data, which is usually performed 4-5 times during the entire stimulation period. For the final maturation of the follicles, hCG, for example Pregnil, is injected, and after 35–36 hours the follicles are punctured.
"Long Protocol"
The protocol is called “long” because, as a rule, it begins on the 21st–23rd (rarely from the 2nd–3rd) day of the menstrual cycle preceding stimulation. To block the pituitary gland, only an agonist is taken for the first 5 days from the start of treatment. After blockade of the pituitary gland is achieved, menstruation begins, and from the second to third day from its onset, stimulation is carried out with drugs containing FSH, in the same way as with the “pure” regimen, but together with the continued administration of the agonist.
"Optimal Protocol"
When using the new antagonist Orgalutran, the stimulation protocol is significantly shortened, although a pronounced, easily reversible blockade of the pituitary gland remains. Stimulation begins, as with the “pure” regimen, from 2–3 days of the menstrual cycle by daily administration of a drug containing FSH. Then, from the 5th or 6th day of stimulation, daily injections of Orgalutran are given, but stimulation continues. Thus, the “Optimal Protocol” becomes short and therefore effective. The combination of the new generation drug Puregon with Orgalutran (antagonist) is: - reduction of treatment time; - better tolerance of injections; - proven effectiveness. Thanks to this, the combined use of Puregon with Orgalutran can be called “Two components of hope in the treatment of infertility.”
Does freezing embryos affect the health of the unborn child?
The first “successful” pregnancy with the transfer of cryopreserved embryos was obtained in 1983. Consequently, this method is far from new, it is actively developing, and its technologies have been improved over the past 30 years.
The cryopreservation method allows embryos to be preserved for a long time, so if an IVF attempt is unsuccessful, the “saved” embryos can be used in the future. In cases where the IVF program was successful and pregnancy occurred, the remaining frozen embryos can be used in the future when the couple decides to have another child. An additional advantage of the method is the reduction in the number of repeated ovarian stimulations and follicle punctures, which significantly reduces the drug load on the female body.
It has been proven that the process of storing embryos frozen does not affect their further development, however, damage to the embryos can occur during the “freezing” and “thawing” stages. Currently, a more effective way of “freezing” is the vitrification method, i.e. rapid “freezing”, during which the survival rate of embryos is much higher (more than 98%) than after slow freezing (about 50%), which was popular before.
The number of progressive pregnancies after cryopreservation of embryos is comparable to the number of progressive pregnancies during the transfer of fresh embryos (on average, 41.6% and 44.3%, respectively) and depends on a number of factors, the main of which are: quality, thickness and preservation of the receptive properties of the endometrium, absence of cavity deformation uterus, embryo quality, woman’s somatic health.
Despite the arguments that doctors give in favor of embryo cryopreservation, most women continue to be extremely wary of this process. As a result of an extensive scientific study in Sweden, it was found that children born after a “cryotransfer” are less likely to have low birth weight and are more likely to be born at term compared to children born after a “fresh transfer”.
So, in modern conditions, “cryopreservation” is absolutely safe and effective in terms of the further development of pregnancy.
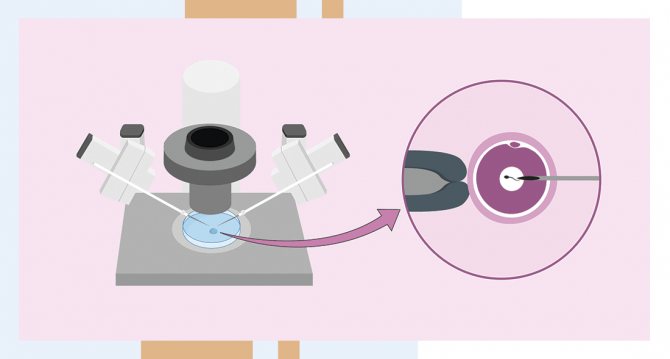
Technique for follicle puncture
Ovarian puncture is a surgical intervention that is performed in compliance with the rules of asepsis and antisepsis in an operating room. The patient is asked to change into sterilized or disposable clothing. Before a woman is put under anesthesia, her blood pressure is measured and some indicators of the cardiovascular system are recorded. After the onset of anesthesia, the gynecologist treats the puncture site with an antiseptic solution. The cervix is exposed in the speculum and fixed with bullet forceps. The inferior speculum is then removed and a hollow needle attached to an ultrasound probe is inserted into the vagina. Using ultrasound, the doctor locates the ovary and follicles, pierces them successively and sucks out the contents.
The average duration of a puncture is 15-20 minutes.
The follicular fluid along with the eggs is transferred to the embryology laboratory. Before fertilization, the oocytes undergo a thorough check. The next stage is the interaction of eggs and sperm. When there is not enough genetic material, fertilization is carried out using the ICSI or PIXI method. In some cases (with massive adhesions in the pelvis, abnormal location of the ovaries), it is impossible to obtain eggs using transvaginal puncture. In such cases, the woman is offered laparoscopy.