Detailed description of the study
Anti-Mullerian hormone (AMH, AMH, MIS) is a dimeric glycoprotein belonging to the family of β-transforming growth factors, a protein hormone that limits the processes of excessive growth in the reproductive organs of male and female organisms. AMH must be monitored when diagnosing and treating infertility in women and men, and when preparing patients for IVF. AMH is a marker of ovarian tumors. Named after the German scientist Johann Muller , who identified a common channel-tube in male and female embryos - the Mullerian duct, from which the uterus, fallopian tubes and vagina develop in women; prostatic uterus and epididymis in men. This hormone ensures sex differentiation in the embryo and is also involved in spermatogenesis and follicle maturation. It serves as an indicator of the function of the gonads, and is used to find out the cause of impaired sex differentiation, male and female infertility, as well as in the diagnosis of certain tumors. Normally, it is synthesized only by Sertoli cells of the testes (both during embryonic development and after birth) and granular cells of the ovaries (only after birth). It gets its name from its unique property of preventing the development of female reproductive structures from a germ called the Müllerian duct. Although the sex of the child is determined at the time of conception, until the 6th week of pregnancy the fetus has undifferentiated sex gonads and the rudiments of the internal reproductive structures of both sexes: the mesonephritic duct (Wolfian) and the paramesonephritic duct (Müllerian). Androgens and developing spermatocytes inhibit AMH . In the absence of androgens and germ cells (or androgen resistance), the AMH expression-enhancing effects of follicle-stimulating hormone (FSH) occur. AMH studies can be useful in the differential diagnosis of intersex disorders, diagnosis of premature puberty (AMH is reduced relative to age) or, conversely, delayed sexual development (AMH is increased relative to age), and assessment of testicular function.
In childhood, AMH may be a real marker of the presence of testicular tissue in conditions where testosterone concentrations are very low.
MG is not expressed during the final FSH-dependent stages of follicle growth. It is believed that changes in AMH expression play an important role in the mechanisms of follicle recruitment and selection, since in the absence of AMH, follicles are more sensitive to FSH. A number of studies have shown that AMH is a quantitative marker of ovarian reserve and can be used when using assisted reproductive technologies in a complex of examinations to assess ovarian reserve and predict the ovarian response to ovulation stimulation.
Men. During differentiation of the male fetus, AMH is produced by Sertoli cells and induces degeneration of the Müllerian duct. Dysfunction of AMH causes persistence of Müllerian duct derivatives in men. This condition is clinically manifested by cryptorchidism, inguinal hernias and reproductive dysfunction and is called persistent Müllerian duct syndrome (PMDS). Before puberty, AMH is produced by the testes, and then its level gradually decreases to residual post-pubertal values. AMH is involved in the transformation of gonocytes and spermatogonia, inhibiting the entry of germ cells into meiosis and the proliferation of Leydig cells until late puberty. Androgens and developing spermatocytes inhibit AMH secretion. In the absence of androgens and germ cells (or in the presence of androgen resistance), the production of AMH by Sertoli cells increases under the influence of FSH. AMH levels are normally elevated in the serum of prepubertal men. The concentration of AMH falls during puberty, then in adult men AMH is maintained at a relatively low level throughout life. Anti-Mullerian hormone is used in the diagnosis of premature puberty - a decrease in AMH relative to age; delayed sexual development - AMH is increased relative to age, in assessing testicular function. In preschool age, AMH is a marker of the presence of testicular tissue in conditions where testosterone concentrations are very low.
Women. In female fetuses, AMH is produced by ovarian granulosa cells in the postnatal period. AMH expression begins in the granulosa cells of primary follicles, is maximum in the granulosa cells of preantral and small antral follicles, then gradually decreases at subsequent stages of follicular development and is practically absent when the follicle size is more than 8 mm. AMH is not expressed during the final FSH-dependent stages of follicle growth. In the ovary, AMH inhibits the selection of primordial follicles, as well as the stimulation of folliculogenesis by FSH. The fact that AMH is specifically produced in granulosa cells of growing but unselected follicles makes it an ideal marker for determining the size of the ovarian follicular reserve. In addition, AMH is not controlled by gonadotropins, is not involved in the classical feedback loop (unlike FSH, estradiol and inhibin B), does not depend on the menstrual cycle, acts not as a systemic, but rather as a paracrine regulatory factor and reflects the population of follicles in the ovary . AMH levels in the blood reflect the number of follicles in a woman's ovaries that are capable of reproduction and allow for monthly ovulation. Low levels of AMH in the blood are associated with a small number of follicles in the ovaries, as a result of which AMH is increasingly being measured in women undergoing treatment for infertility. AMH levels are elevated in polycystic ovary syndrome, in which there is an increase in the pool of antral follicles. An increase in the number of antral follicles by 2-3 times is accompanied by a 2-3 times increase in the level of AMH in the blood serum. Another area of application of AMH is the detection of ovarian granulosa cell tumors, in the presence of which the level of AMH increases significantly.
Anti-Mullerian hormone
How to prepare for an Anti-Mullerian hormone (or Müllerian inhibitory substance) test?
In accordance with the instructions of the attending physician.
- For women, the study is usually carried out on the 3rd day of the cycle (both with an intact menstrual cycle and with stimulation of ovulation in the IVF procedure).
- For men, the study is usually carried out on any convenient day.
3 days before taking blood, avoid intense sports training. Acute stress can have a noticeable effect on the secretion of gonadotropins; The study should not be performed during any acute illness.
Do not smoke 1 hour before taking blood.
Deadline for testing for Anti-Mullerian hormone (or Müllerian inhibitory substance)
Laboratory analysis: every week – on Wednesdays .
What are the normal levels (decoding) of Anti-Müllerian hormone (or Müllerian inhibitory substance)?
| Floor | Anti-Mullerian hormone, ng/ml |
| Women: 0 – 9 years Reproductive age ( 15 – 41 years ) Decreased functional ovarian reserve A sharp decrease in the functional reserve of the ovaries | 3.5 ±1.8 (always < 10 ) 1,1 – 2,5 < 1,1 < 0,8 |
| Men | 0.49-5.98 |
What is Anti-Mullerian hormone or Mullerian inhibitory substance?
Anti-Müllerian hormone or Müllerian inhibitory substance (AMH/IVM, AMH/MIS) is a dimeric glycoprotein that belongs to the family of β-transforming growth factors.
During embryonic development, it is secreted by Sertoli cells and is responsible for regression of the Müllerian ducts in men. Before puberty, AMH is produced by the testes and then gradually declines to residual postpubertal levels. Anti-Mullerian hormone dysfunction causes persistence of Müllerian duct derivatives in men. This condition is clinically manifested by cryptorchidism, inguinal hernias and reproductive dysfunction and is called persistent Müllerian duct syndrome (PMDS). SPMP is a rare form of false male hermaphroditism. Despite the fact that testicular differentiation is not impaired in patients with SPMS, they often experience infertility.
In women, from birth until menopause, AMH is produced by ovarian granulosa cells. Women have relatively low serum AMH levels compared to men until puberty. After this, the concentration of circulating AMH slowly decreases to undetectable values.
The concentration of AMH in women correlates with the number of antral follicles , with age, best reflecting the decline in reproductive function in healthy women with proven fertility. The patient's ovarian reserve according to the results of the triple test (inhibin B, AMH and FSH on the 3rd day of the cycle) is compared with the expected reserve for a given age, which allows monitoring reproductive function.
Anti-Mullerian hormone (AMH, AMH) - a test to assess premature or delayed sexual development in men and women; used to assess the ovarian reserve in women (assessing the number of functionally active follicles in a woman’s ovaries); indicator in the diagnosis and monitoring of women with normogonadotropic anovulatory infertility; indicator of tumor processes in ovarian granulosa cells.
In women, AMH synthesis occurs in the granulosa cells of the primary follicles. The maximum amount of AMH is in preantral and antral follicles with a diameter of 4 mm. and is not expressed in dominant follicles. After selection of a dominant follicle, AMH expression decreases. If the number of antral follicles decreases, AMH expression also decreases . With further development of the follicle, its synthesis decreases and is practically absent (FSH-dependent stages) with a follicle size of more than 8-9 mm in normal ovaries, which is a necessary condition for the selection of a dominant follicle. There are two main effects of AMH on the ovary: 1. it suppresses the primary stages of follicle growth; 2. suppresses FSH-dependent growth and selection of preantral and small antral follicles. It is believed that AMH is not under the control of gonadotropic hormones (FSH, LH) and adequately reflects the number of follicles . Therefore, its determination is considered an important test as a marker for determining the ovarian follicular reserve (estimation of the number of functionally active follicles in a woman’s ovaries, i.e. the number of eggs in women at a given time that can be used for fertilization), also for assessing ovarian dysfunction and ovarian aging. Reduced AMH values indicate a decrease in ovarian reserve.
In oncological practice, the determination of AMH is important in the diagnosis of granulosa cell tumors of the ovaries, since this leads to a significant increase in its concentration.
In men, AMH is secreted by Sertoli cells (cells lining the seminiferous tubules in the testes and involved in spermatogenesis) and is a factor leading to atrophy/involution of the Müllerian ducts, which are the rudiments of the reproductive tract in women. In women, the Müllerian duct forms the epithelium of the uterus, fallopian tubes and vagina. In addition to AMH, Sertoli cells synthesize androgen binding protein, activin and inhibin. AMH synthesis begins during embryonic development and persists throughout life. The highest concentration of AMH is observed in the prepubertal period, decreasing during puberty and remaining at fairly low levels in adult men throughout life. Dysfunction of AMH causes persistence of Müllerian duct derivatives in men. Clinically, this is manifested by cryptorchidism, inguinal hernias and reproductive dysfunction.
Why is it important to do an Anti-Mullerian hormone (or Müllerian inhibitory substance) test?
- Detection of premature or delayed puberty.
- Determination of gender in doubtful cases.
- Diagnosis of cryptorchidism and anorchism.
- Assessment of male sexual function at any age.
- Study of ovarian reserve and premenopausal changes in women.
- Diagnosis and control of granulosa cell ovarian cancer.
- Unsuccessful IVF attempts, insufficient response to stimulation.
- Infertility of unknown origin.
- Fertilization problems.
- Borderline or elevated FSH values.
- During autotransplantation of ovarian tissue.
- During chemotherapy as a marker of ovarian function.
- Confirmation of the presence of testicular tissue.
- When assessing the effectiveness of antiandrogen therapy.
What diseases are tested for Anti-Mullerian hormone (or Müllerian inhibitory substance)?
- Tumors, infertility, sexual dysfunction.
To check/improve the performance of which organs should you test for Anti-Mullerian hormone (or Müllerian inhibitory substance)?
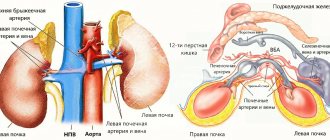
- Ovaries, testicles.
When is it necessary to get tested for Anti-Mullerian hormone (or Müllerian inhibitory substance)?
- For women, as a rule, the study is carried out on the 3-5th day of the cycle.
- For men, the study is usually carried out on any convenient day.
Excesses of the norm of Anti-Mullerian hormone (or Müllerian inhibitory substance) are observed in the following diseases.
- Tumors in ovarian granulosa cells.
- Delayed sexual development.
- LH receptor defects.
- Bilateral cryptorchidism (AMH receptor mutations).
- Normogonadotropic anovulatory infertility.
- Polycystic ovary syndrome.
- Antiandrogen therapy.
Low values (below normal) of Anti-Mullerian hormone (or Müllerian inhibitory substance) are observed in the following diseases
- Decreased ovarian reserve.
- Obesity in late reproductive age.
- Menopause.
- Gonadal dysgenesis.
- Hypogonadotropic hypogonadism.
- Anorchism.
- Premature sexual development.
Results are calculated in ng\ml
Conversion to SI units: 1ng\ml = 7.14 rM
Preparing for analysis
To obtain the most reliable results, you need to first prepare for the AMH analysis:
- 3 days before the test, physical and emotional stress should be minimized;
- 2 days before the study, stop taking any hormonal drugs (after consulting with your doctor);
- do not smoke 3 hours before the test;
- Do not eat for at least 2-3 hours before the test.
Blood for AMH is taken from a vein. Women undergo this analysis on days 2-5 of the monthly cycle. The AMH test is not done during infectious and inflammatory diseases, or after prolonged sports training.