Glycated hemoglobin is one of the indicators of a biochemical blood test. Allows you to determine the average blood sugar level over the past three months. In tests it may be referred to as HbA1C or A1C.
Knowing its significance is important in order to promptly identify diabetes mellitus, monitor the course of the disease and the effectiveness of the therapy used.
What is glycated hemoglobin?
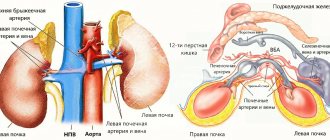
Glycated, or glycosylated, is called hemoglobin bound to glucose (abbreviated as “glycohemoglobin”). As you know, hemoglobin is contained in red blood cells - erythrocytes. Sugars penetrate the red blood cell membrane and interact with hemoglobin, resulting in glycohemoglobin. Unlike the level of free glucose, not bound to hemoglobin, the level of glycated hemoglobin remains relatively constant in the blood because hemoglobin is normally stable inside red blood cells. After working for 4 months transporting oxygen and carbon dioxide, red blood cells are destroyed in the red pulp of the spleen. Their hemoglobin and glycohemoglobin are broken down in the spleen and liver. The end product of hemoglobin breakdown, bilirubin, does not bind to sugar.
Just because red blood cells live for 4 months, the level of glycohemoglobin remains constant for 120 days. It is not affected by the time of day, physical activity, food intake, or emotional state.
What may affect the results
Glycated hemoglobin test results may be inconsistent in patients with hemoglobinopathy, including sickle cell disease, pregnancy (second and third trimesters) and the puerperium, HIV, recent bleeding or transfusion, erythropoietin therapy, and patients on hemodialysis. reflect the true glucose content.
Only plasma glucose criteria should be used to diagnose diabetes in these situations. Interpretation of the result may be complicated by the presence of variant forms of hemoglobin: hemoglobin A2, which increases in beta thalassemia (a genetic disease), and fetal hemoglobin (fetal hemoglobin), which remains high until 6 months after birth.
What does this indicator mean?
The content of glycated hemoglobin is proportional to the content of sugar in the blood - glycemia. The higher its level, the more hemoglobin will bind to glucose and the more the level of glycated hemoglobin will rise. For both diabetics and those who are not sick, an increase in glycohemoglobin levels is a reason to consult a doctor. Patients are prescribed therapy or recommended to change their lifestyle in time. To prevent the disease, a low-carbohydrate diet is prescribed.
Correspondence between glycated hemoglobin (HbA1C) and average blood glucose levels for 3 months
| HbA1C,% | Glucose, mmol/l | What does it mean |
| 4 | 3,8 | Carbohydrate metabolism is normal, the risk of diabetes is minimal |
| 4,5 | 4,6 | |
| 5 | 5,4 | |
| 5,5-5,7 | 6,5 | |
| 5,7-6,0 | 6,5-7,0 | Increased risk of diabetes. It is advisable to limit your consumption of sweets and consult an endocrinologist. |
| 6,1-6,4 | 7,0-7,8 | High risk of diabetes. It is necessary to consult an endocrinologist. |
| 6.5 or more | 7.9 or more | The diagnosis of diabetes mellitus is made preliminary. Additional tests are needed to confirm or refute. |
Complexes with this research
Cola and chips Analysis of metabolic disorders caused by an unbalanced diet RUR 3,020 Composition
Women's check-up No. 1 38 studies for annual preventive examination RUR 19,290 Composition
Nutritionist recommends Metabolic status assessment RUB 7,570 Composition
IN OTHER COMPLEXES
- Prediabetes and diabetes 950 R
- Advanced women's anti-aging diagnostics RUB 28,680
- Anti-aging diagnostics in postmenopause RUB 12,630
- Preventive check-up RUB 11,960
- Risk of severe COVID-19 RUB 1,090
Sources
- Ribeiro de Lima JG., Abud GF., Freitas EC., Bueno Júnior CR. Effects of the COVID-19 pandemic on the global health of women aged 50 to 70 years. // Exp Gerontol - 2021 - Vol150 - NNULL - p.111349; PMID:33892133
- Manaer T., Yu L., Nabi XH., Dilidaxi D., Liu L., Sailike J. The beneficial effects of the composite probiotics from camel milk on glucose and lipid metabolism, liver and renal function and gut microbiota in db/db mice. // BMC Complement Med Ther - 2021 - Vol21 - N1 - p.127; PMID:33888105
- Mani Deepthi D., Vaikkakara S., Patil A., Ganta S., Sachan A., Raghavendra K., Kiranmayi VS., Chowhan AK. Effect of Correction of Hyperthyroidism with Anti-thyroid Drugs on the Glycated Hemoglobin in Non-diabetic Patients with Primary Hyperthyroidism. // Int J Endocrinol Metab - 2021 - Vol19 - N1 - p.e105751; PMID:33815517
- Pohanka M. Glycated Hemoglobin and Methods for Its Point of Care Testing. // Biosensors (Basel) - 2021 - Vol11 - N3 - p.; PMID:33806493
- Hu X., Deng H., Zhang Y., Guo X., Cai M., Ling C., Li K. Efficacy and Safety of a Decision Support Intervention for Basal Insulin Self-Titration Assisted by the Nurse in Outpatients with T2DM: A Randomized Controlled Trial. // Diabetes Metab Syndr Obes - 2021 - Vol14 - NNULL - p.1315-1327; PMID:33790599
- Okamoto T., Shima H., Noma Y., Komatsu M., Azuma H., Miya K., Tashiro M., Inoue T., Masaki C., Tada H., Takamatsu N., Minakuchi J. Hereditary spherocytosis diagnosed with extremely low glycated hemoglobin compared to plasma glucose levels. // Diabetol Int - 2021 - Vol12 - N2 - p.229-233; PMID:33786277
- Mazahery H., Gammon CS., Lawgun D., Conlon CA., Beck KL., von Hurst PR. Pre-diabetes prevalence and associated factors in New Zealand school children: a cross-sectional study. // NZ Med J - 2021 - Vol134 - N1531 - p.76-90; PMID:33767489
- Abbas E., Ahmed Siddiqui I., Khan MS., Perveen K., Butt A., Fawwad A. Fasting Glucagon Level in Type 2 Diabetes and Impaired Glucose Tolerance and Its Association With Diabetes-Associated Clinical Parameters: A Study From Karachi, Pakistan. // Cureus - 2021 - Vol13 - N2 - p.e13430; PMID:33758717
- Alkethiri K., Almtroudi T., Jurays AB., Abanumay F., Aldammas M., AlKhodheer M., Iqbal M., Habib SS., Bashir S. The relationship between type 2 diabetes mellitus with cognitive functions. // Heliyon - 2021 - Vol7 - N3 - p.e06358; PMID:33748460
- Jaber H., Issa K., Eid A., Saleh F.A. The therapeutic effects of adipose-derived mesenchymal stem cells on obesity and its associated diseases in diet-induced obese mice. // Sci Rep - 2021 - Vol11 - N1 - p.6291; PMID:33737713
Reasons for a decrease in glycated hemoglobin in the blood:
- Hypoglycemia (low blood glucose).
- Normalization of glucose levels in patients with diabetes (effective treatment).
- False underestimation in hemolytic anemia.
- False underestimation after bleeding, blood transfusion (blood transfusion).
Sources:
- Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2021 American Diabetes Association Diabetes Care Jan 2021, 44 (Supplement 1) S15-S33; DOI:10.2337/dc21-S002
- Cas Weykamp, Ph.D. HbA1c: A Review of Analytical and Clinical Aspects. Ann Lab Med 2013;33:393-400
- Wenjia Guo, Qi Zhou, Yanan Jia, Jiancheng Xu. Increased Levels of Glycated Hemoglobin A1c and Iron Deficiency Anemia: A Review. Med Sci Monit 2021 Nov 7;25:8371-8378.
- Oliver Schnell, J Benjamin Crocker, Jianping Weng. Impact of HbA1c Testing at Point of Care on Diabetes Management. J Diabetes Sci Technol 2021 May;11(3):611-617.
Glycated hemoglobin: the norm in a blood test, which shows whether it is increased or decreased
It would seem, how can iron-containing protein be an indicator of the latent course of diabetes mellitus? However, with an increased concentration of glucose in the body, glycosylated (glycated) proteins begin to form: glycated hemoglobin, fructosamine or glycated albumin, glycosylated lipoproteins. An increase in sugar content, even for a short time, leaves a trace in the body that can be detected a month and a half, or even two, after this event.
Where does glycosylated hemoglobin come from?
Having reached the bloodstream and not being utilized due to exceeding the permissible amount, glucose reacts with the proteins present there (hemoglobin, albumin, lipoproteins), forming a strong compound. This process is irreversible and is called glycation or glycosidation (Maillard reaction).
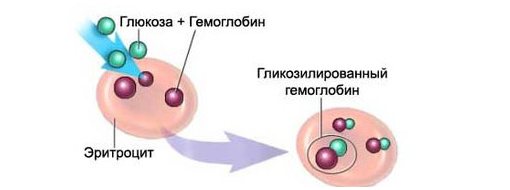
Considering the relatively high life expectancy of red blood cells (up to 3 months), and, consequently, the hemoglobin contained in them, this interaction of glucose with hemoglobin is taken as the basis in such a biochemical blood test for sugar as glycated hemoglobin. An increase in the amount of glucose in diabetes mellitus is a catalyst for this reaction; sugar combines faster (2-3 times) with hemoglobin, which subsequently will no longer be able to get rid of the side component and will carry information about it until its destruction, that is, as long as the red blood cells are alive . The amount of hemoglobin reacting with glucose will express the degree of glycation, which, in turn, indicates the average amount of glucose 1.5 - 2 months before the study. However, the reader should not think that glycated hemoglobin (hemoglobin Ale, HbAl) is some kind of foreign substrate for the body; during the metabolic process it is formed normally in healthy people (no more than 6% of the total Hb content), which will be mentioned below.
Thus, the analysis for glycated hemoglobin allows you to catch the seemingly lost trace of carbohydrates and shows what the diabetic’s blood sugar level was, for example, a month ago. Glucose that has jumped out of the range of normal values for a short time will not be able to “sneak away”: it will react with Hb, combine with it, but will not be able to come back, so it will remain in its composition and will be detected when analyzing glycated hemoglobin.
Norm and scope of laboratory test
The norm of glycated hemoglobin in people who do not have diabetes mellitus does not reach 6% and usually ranges from 4 to 5.8%. Differences due to gender, age, and geographic location are somehow not provided for for this indicator, since they simply do not exist. Glycohemoglobin may be slightly increased in children in the first months of life, which is explained by the presence of fetal hemoglobin in their blood (by the age of one year the baby will completely get rid of it), otherwise - no more than 6% for all healthy groups of the population.
Diabetics can expect different digital values of the indicator (up to 12% and higher), so the results are assessed in accordance with generally accepted criteria for determining the regulation of carbohydrate metabolism:
- A hemoglobin A1C indicator that does not reach 6% indicates the absence of violations of the regulatory mechanisms of carbohydrate metabolism;
- An Hb A1C level of 6–8% indicates good regulatory and compensatory abilities of the body and the effective participation of sugar-lowering drugs in relation to carbohydrate metabolism;
- The proportion of glycated hemoglobin, approaching 9%, indicates that the regulation process is still going satisfactorily and diabetes mellitus is well compensated, but therapy requires revision;
- The 9 - 12% content of hemoglobin that has undergone glycosidation is alarming - these values give reason to believe that the regulatory mechanisms are on the verge of exhaustion, the body cannot cope with the disease, drugs that reduce sugar, it is only partially compensated;
- An increase in glycosylated hemoglobin of more than 12% indicates a lack of regulatory and compensatory abilities - diabetes is not compensated, and therapeutic measures are ineffective.
Obviously, this indicator is increased in diabetes mellitus. It can also indicate how high the risk of developing complications of carbohydrate metabolism disorders (kidney disease, diseases of the organs of vision) is, therefore it is successfully used:
- For diagnosing a latent form of “sugar disease”, and therefore suitable for screening studies;
- In case of long-term monitoring of the course of the disease and the effectiveness of the prescribed therapy;
- To determine the regulation of carbohydrate metabolism and the degree of compensation of the pathological process.
In addition to the listed tasks, the determination of glycohemoglobin serves as a good addition to the glucose load test (sugar curve) when searching for the causes of increased blood glucose in people who are not yet classified as diabetics. In addition, the test is also used when examining for the detection of gestational diabetes mellitus, however, during pregnancy, the analysis of glycated hemoglobin is not a fundamental study. In the case of searching for the hidden course of diabetes mellitus during pregnancy, other methods for determining an increase in the concentration of glucose in the blood, which can trigger the development of the pathological process, are more acceptable.
Deviations of glycated hemoglobin levels from normal
An increased content of glycated hemoglobin can be observed not only in diabetes mellitus and conditions accompanied by impaired glucose tolerance, for example:
- A high concentration of fetal hemoglobin leads to an increase in the level of glycohemoglobin (it is understandable that the indicator increases in children in the first months of life, but when HbF leaves the baby’s blood, the norm of the child’s glycated hemoglobin becomes equal to that of an adult);
- Lack of iron in the body is manifested by an increase in the percentage of Hb A1C;
- After removal of the spleen (splenectomy), changes in many blood parameters can be expected, including an increase in glycosylated Hb.
A decrease in glycohemoglobin levels is also considered an uncommon occurrence. A decrease in its concentration occurs in the following cases:
- Decreased blood sugar levels (hypoglycemia);
- Increased production of red blood pigment, that is, hemoglobin;
- Activation of the hematopoietic system (erythropoiesis) after blood loss;
- Increased destruction of red blood cells in certain pathological conditions (hemolytic anemia);
- Hemorrhages (acute and chronic);
- Kidney failure;
- Blood transfusions.
As you can see, the list of deviations is small, so this biochemical test is most often used by endocrinologists to monitor the course and treatment of diabetes mellitus.
Taking the test is very easy because:
- It does not require coming to the laboratory on an empty stomach or any other restrictions, because information about the glucose level in the blood has not been accumulated in one day and is quite deeply and securely hidden.
- Having firmly bound to hemoglobin, sugar will not leave the blood pigment until the latter is destroyed, so the patient definitely has a month to think about it;
- Doctors have even more time, because they mainly focus on 60 days. This period follows from the lifespan of red blood cells, taking into account the fact that red cells of different ages circulate in the bloodstream.
Diabetics have to take a glycated hemoglobin test every 3 months so that the doctor knows the situation and promptly prescribes the necessary medications or makes adjustments to the treatment regimen used. If the test results are in doubt, which happens in patients with some blood pathology (hemolytic anemia), you should turn to alternative methods of laboratory diagnosis of diabetes, for example, a study of glycosylated albumin (fructosamine). Fructosamine reflects the state of carbohydrate metabolism in a given patient during the last 2-3 weeks before the analysis.
Doctor of the agricultural department of the Central House of Children's Hospital K.I. Vasilevskaya
HbA1C: results and diabetic complications
In 2010, according to the American Diabetes Association guidelines, HbA1C was adopted in many countries as a diagnostic test using a cutoff value of 48 mmol/mol, corresponding to a percentage level of 6.5%.
If the HbA1C level is between 5.7% and 6.4%, a person is considered to be at increased risk of both diabetes and cardiovascular disease and is strongly advised to take appropriate lifestyle measures.
Cardiovascular disease
Each percentage reduction in HbA1C levels results in a corresponding reduction in risk:
- Heart failure – by 16%;
- Heart attack – 14%;
- Stroke – 12%;
- Risk of amputation – 43%;
- Mortality from all causes – 14%;
- Mortality from diabetes – 21%;
- Microvascular diseases – 37%.
The test must be performed using an NGSP-certified assay and repeated if the result is inconclusive. This is necessary to ensure consistency between laboratories and requires that quality assurance programs meet standards.
Although portable tests are not recommended for diagnosis, they may sometimes be necessary if the patient is unable to ambulate. In this case, the best available technology should be used.
Benefits of HbA1C testing
Currently, the HbA1C test is also used to diagnose diabetes, although previously the test was prescribed only for monitoring already diagnosed patients. Endocrinologists believe that the HbA1C test is in many ways better than the traditional fasting glucose test or oral glucose tolerance test for diagnosing diabetes.
Its advantages::
- simplicity;
- ability to perform at any time of the day;
- does not require preparation and abstinence from food;
- only one blood sample is needed;
- reliability in both diagnosing and predicting the risk of some chronic complications of diabetes.
The blood for the test can be taken either from a vein (venipuncture) or from a finger, depending on whether the test is done in a laboratory or in a doctor's office (or at home).