Many patients are interested in what lancets for collecting blood are. Taking blood from a finger is a procedure that an adult or child must undergo at least once in their life.
But while adults tolerate the tests normally, children are afraid of this procedure, especially of pricking their finger with a needle.
But technology does not stand still, so for several years now an automatic scarifier has been used instead of a conventional device.
Blood sampling with this device is painless, since a special device called a lancet is used for analysis. This device can be used to analyze even infants.
What is the instrument?
A lancet for taking blood from a child is a special disposable device made of plastic, inside of which there is a scarifier (special pen) made of medical steel. The instrument is designed for painless collection of capillary blood from children for general analysis or testing for glucose levels.
The design of the lancet was created in such a way that it was not possible to even accidentally use the instrument twice. The needle is hidden in a plastic cap and after use it is returned and then locked inside.
The skin can be punctured automatically by touching the skin or by pressing a special button. Lancets are safe and convenient devices that can be used not only in the laboratory, but also at home.
Modern technologies for qualitative analysis of capillary blood
Blood collection systems:
23.11.2018

In clinical practice, situations quite often arise when it is impossible to take blood for laboratory tests from peripheral veins. These are, first of all, premature babies and children of the first year of life, elderly people and obese patients in critical condition. For this purpose, there are systems designed for the collection, transportation and subsequent examination of capillary blood. The largest range of microtubes (microtainers with a built-in collector) for collecting capillary blood with the same range of reagents as for tubes intended for collecting venous blood (with the exception of tubes for studying hemostasis) is produced.
As you know, laboratory research is divided into three main stages: preanalytical (outside the laboratory), analytical and postanalytical. The analytical stage is directly related to the function of the laboratory, and it is easily controlled by laboratory specialists, and the use of modern diagnostic systems (automatic analyzers, diagnostic kits, control materials and calibrators) minimize errors at the laboratory stage. The preanalytical stage can be least controlled by the laboratory, since a significant part of this stage is carried out by employees of medical institutions. And it is this stage that accounts for up to 93% of errors in the production of analyzes [].
The centralized clinical diagnostic laboratory carries out research for 40 medical institutions in the city of Krasnoyarsk. Therefore, the issue of proper preparation of patients and taking biological material from children is very urgent. Control of preanalytical factors is key to ensure quality results. By reducing the number of errors at any stage of preanalytical preparation, you can significantly improve the quality of research, reduce the number of repeated samples, and reduce the cost of working time and money for examining patients. The psychological and physical discomfort of the patient is also important when the question of re-obtaining biomaterial arises (children and pregnant women).
The Central Clinical Children's Hospital performs studies for children in the city's outpatient clinics, which accounts for 43% of all studies performed. And 57% is performed for patients at antenatal clinics in the city.
The analysis of rejected hematological samples over the year allowed us to estimate the frequency of errors at the preanalytical stage. Hemogram examinations average 17,500 per month. To perform hematological examinations, we use capillary and venous blood. We carry out hematological studies from capillary blood only in children, and this share is 58%, and 42% is the study of venous blood (these are older children and the female population). The percentage of defects when obtaining capillary blood was 2.2%, when receiving venipuncture the percentage was 0.7%. Thus, the percentage of errors when taking capillary blood is three times higher than when taking venous blood. The main reasons for the poor quality of the blood samples taken are: clots in the sample and a violation of the sample volume, which leads to a violation of the blood-anticoagulant ratio (Fig. 1).
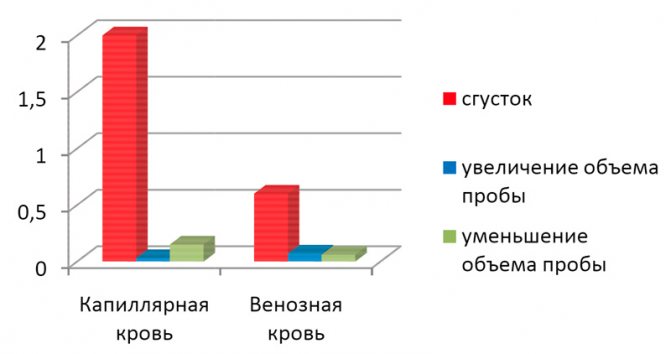
Fig. 1 - The main reasons for the low quality of blood samples taken.
- Samples obtained with clots accounted for the largest proportion of errors in both capillary and venous blood collections. Three times more clots were obtained in capillary blood than in venous blood. How can this fact be explained?
- Contact activation of coagulation when taking capillary blood;
- The release of tissue thromboplastin under finger pressure;
- Relatively time-consuming blood collection procedure;
- Small sample volume and therefore problematic mixing;
- Insufficient and untimely mixing of the test tube.
Venous blood is considered the best material for laboratory research. With a certain standardization of the processes of collection, storage, and transportation of venous blood, it is possible to achieve minimal trauma and activation of cells, admixture of tissue fluid, while it is always possible to repeat and/or expand the analysis (for example: in case of low hemoglobin, prescribe reticulocytes) and, as a result, minimize the need repeated blood collection procedures (a very important factor for children) and the impact on the correctness and accuracy of the results.
Capillary blood collection for laboratory research is possible in the following situations:
- for burns that occupy a large surface area of the patient’s body;
- if the patient is severely obese;
- with an established tendency to venous thrombosis;
- in newborns;
- with the persistent desire of the parents.
The anatomical structure of the circulatory system of children determines the need to correctly select the puncture site and medical instruments. In pediatric practice, it is possible to take capillary blood from a finger, heel and, in rare cases, from the earlobe. Finger taping should not be performed on infants as it may cause bone damage. In this case, a suitable puncture site for obtaining a sample is the heel at the distal part of the calcaneus. In this regard, it seems important to use automatic lancets that guarantee low trauma and compliance with the required puncture depth, depending on the type of lancet chosen. There is a direct relationship between the volume of blood received and the depth of the puncture. In this regard, the type of lancet should be selected in accordance with the puncture site and the volume of the resulting sample. produces disposable lancets with different types of piercing devices: needle or blade, as well as with different puncture depths. BD Microtainer® Violet Contact Activated Lancets are designed to obtain a single drop of blood and provide at least 90% pain-free patient experience [], while BD Microtainer® Blue Lancets are designed to obtain up to 0 .5 ml of blood and provide a capillary blood flow rate of at least 2 µl/s []. For capillary blood collection from newborns, preference should be given to contact-activated BD Quikheel™ with a blade that performs a semicircular cutting movement, which allows you to obtain a good current from the wound in at least 90% of cases [].
Taking into account the age-related characteristics of children’s behavior during the blood collection procedure (mobility, emotional stress, etc.), attention should be paid to the sequence of filling the tubes. To correctly collect capillary blood, you should start with tubes with anticoagulants (for hematological studies), and then use microtainers or tubes to obtain serum or plasma intended for biochemical, immunological and other types of research. For example, the use of the BD Microtainer® PST™ amber tube ensures that plasma samples are stable for bilirubin testing for at least 24 hours at room temperature []. It should be noted that the study of hematological parameters, blood group, glucose and some other biochemical parameters in children is possible from capillary blood, but the study of indicators of the hemostatic system and hormones must be carried out only from venous blood.
Deviations from standards during sample collection, sample transportation and storage, and patient-related factors can lead to incorrect or inaccurate test results and therefore misdiagnosis. We looked at the effect of the volume of the sample obtained on the research results. Capillary blood was taken simultaneously from one patient in microtainers with K2EDTA and K3EDTA from different manufacturers. Samples were taken taking into account the manufacturers' recommendations and with a violation of the volume, as is often the case in practice (Fig. 2, 3).
|
|
| Rice. 2. Samples with K2EDTA with labels for collecting 250–500 μl of blood | Rice. 3. Samples with K3EDTA with labels for collecting 500 μl of blood |
Excess EDTA, regardless of concentration, negatively affects red blood cells, first causing them to shrink and then, over time, to swell, which leads to an increase in the average volume and a decrease in the average hemoglobin content in one red blood cell. In addition, the use of K2EDTA in BD Microtainer® tubes is accompanied by the absence of microclot formation [], and the BD Microtainer® MAP tube with K2EDTA, designed specifically for automatic capillary blood analyzers, ensures the risk of microclot formation of no more than 2% [] and the stability of hematological parameters is no less 12 hours when storing samples at room temperature []. At the same time, the violations identified during our studies are most pronounced in samples with KZEDTA. Violation of the blood-anticoagulant ratio leads to swelling of platelets and their splitting, which is expressed in an increase in their number, since the resulting fragments are quite large in size and can be counted as normal blood platelets. CZEDTA also causes a decrease in the total number of leukocytes and their degenerative changes. In this regard, attention should be paid to the anticoagulant used, to strict compliance with the sample volume recommended by the manufacturer, as well as to thorough and timely mixing of the sample.
When research is centralized, blood collection can be least controlled by the laboratory. Often, the choice of material and puncture site is carried out by health care facility staff without taking into account the requirements of the laboratory, which forces some samples to be rejected. Our laboratory has developed criteria for refusing to conduct research in the following cases: the material taken is in the wrong test tube (i.e., with the wrong filler); the presence of clots in a sample with anticoagulants; sample volume discrepancy (deviation +10% allowed); hemolysis of the sample (except for studies that are not affected by hemolysis); absence of a barcode on the direction or tube; lack of a list of studies, etc. Since the procedural nurse is not part of the laboratory staff, and the laboratory is responsible for the final result to the patient, it is necessary to develop clear instructions:
- by choosing the blood collection procedure (venous or capillary);
- by choosing medical instruments for drawing blood (a needle with a certain diameter, a lancet with a different type and depth of a piercing device);
- by choosing test tubes and microtainers with the necessary filler;
- according to the sequence of their filling.
We consider it important to train nurses in advanced training courses in the techniques and rules for collecting capillary and venous blood using vacuum systems and microtainers, with the subsequent issuance of a certificate.
Compliance with the rules of the preanalytical stage will minimize laboratory errors.
Table 1. Results of a comparative analysis of hematological parameters when taking different volumes of capillary blood into tubes with K2EDTA
| K2EDTA | Sample volume recommended by the manufacturer | Sample volume violation | % change | ||
| 500 µl | 250 µl | 120 µl | 60 µl | ||
| MSN | 27,0 | 26,8 | 24,9 | 26,0 | 3,0 |
| MCV | 77,1 | 78,2 | 79,3 | 79,5 | 3,0 |
| Hematocrit | 33,0 | 33,2 | 33,4 | 33,1 | 0,3 |
| Platelets | 170 | 173 | 180 | 183 | 7,0 |
Table 2. Results of a comparative analysis of hematological parameters when taking different volumes of capillary blood into tubes with K3EDTA
| K3EDTA | Sample volume recommended by the manufacturer | Sample volume violation | % change | ||
| 500 µl | 250 µl | 120 µl | 60 µl | ||
| MSN | 27,7 | 27,2 | 27,6 | 26,6 | 4,0 |
| MCV | 73,5 | 76,0 | 75,7 | 77,0 | 5,0 |
| Hematocrit | 31,0 | 31,6 | 31,0 | 31,7 | 2,2 |
| Platelets | 174 | 180 | 186 | 186 | 7,0 |
You can read the full version of the article here"
Literature
- 1. Comparative Evaluation of the BD Microtainer® Contact-Activated Lancet (High Flow, Blue) with Other Market-leading Lancets for Blood Flow and Ease of Use during Finger Puncture Procedures // VS7607?WHITE PAPER (2008).
- 2. Comparison of BD Microtainer® Contact-Activated Lancet (Low Flow) with BD Microtainer® Genie™, LifeScan OneTouch® SureSoft™ Gentle, and SurgiLance™ One-Step PLUS Safety Lancets for Comfort, Ease of Use, and Blood Volume // VS7499?WHITE PAPER (2006).
- 3. A Comparison of BD Microtainer® MAP Microtube for Automated Process with the BD Microtainer® Tube with Microgard™ Closure for Routine Hematology Testing on the Beckman Coulter® LH 750 Over Time // VS8114?WHITE PAPER (2010).
- 4. Comparison of BD Microtainer® PST™Amber Tubes with BD Microgard™ Closure to BD Microtainer® PST™ Clear Tubes with FloTop Collector for visual and Total Bilirubin // VS5815 (2004).
- 5. Sang Hyuk Park, Hyun-Sook Chi, Mi-Ok Choi, Borae G. Park, Seongsoo Jang and Chan-Jeoung Park. Improved turnaround time for neonatal hematology profile tests (complete blood count) using a new microcollection tube // Clin. Chem. Lab. Med. 2011; 49(6):1083–1085.
- 6. Parul Singla, Anuj Anand Parkash, Jayshree Bhattacharjee. Preanalytical Error Occurrence Rate in Clinical Chemistry Laboratory of a Public Hospital in India // Clin. Lab. 2011; 57:749–752.
- 7. Shah V., Taddio A., Kulasekaran K., O'Brien L., Kelly E. Evaluation of a New Lancet Device (BD QuikHeel) on Pain Response and Success of Procedure in Term Neonates // Arch. pediatrician adolesc. med. 2003; 157.
Authors T. G. Skorokhodova, S. V. Matushkina, D. A. Grishchenko.
Centralized clinical diagnostic laboratory, Krasnoyarsk Federal State Budgetary Institution "Federal Center for Cardiovascular Surgery" of the Ministry of Health of Russia, Krasnoyarsk
Source Scientific and practical journal “Clinical and Laboratory Consilium”, No. 1 (45) February 2013
Tags: Blood test, Hematology, Diagnostics, Blood, Laboratory, Medicine, Test tubes
« Back to article list Share on
How to use the tool?
Choosing a lancet as a tool for collecting blood from children has many advantages. The main advantage is that the child does not see the needle, so an adult can safely draw blood. In addition, the instrument fits tightly to the skin, so children do not feel pain at the time of the puncture, and the wound heals much faster. The properties of blood do not change in any way during such sampling, so lancets reasonably replace conventional scarifiers in hospitals.
Algorithm for collecting blood from a child using a lancet:
- A special protective cap is removed to ensure sterility;
- The lancet is firmly applied to the baby's skin;
- When you lightly press the device (if it is automatic) or press the button, blood sampling begins.
Main advantages

When using a scarifier to draw blood after a puncture, the healthcare worker squeezes the patient's finger to obtain the amount of biofluid necessary for analysis. In this case, blood appears on the surface of the skin and interacts with air, which can affect its composition and reduce the reliability of the data obtained. The use of a lancet allows you to avoid this, because the biomaterial immediately goes into a special reservoir. In addition, the emotional state of the patient, which also affects the composition of the blood, can distort the results, albeit slightly.
And this is not the only advantage of the modern device. Lancets have a number of other advantages:
- the needles used have minimal dimensions: 0.25-0.8 mm in diameter and 1.8 mm in length, so no hematomas remain at the puncture site, and a small wound heals in 1.5-2 hours, which is especially important when diagnosing diseases in newborns , infants;
- the absence of the human factor, such as hand trembling, excessive or insufficient physical effort, ensures rapid penetration, which reduces the time of the procedure and makes it painless;
- the sterility of lancets for blood collection is ensured by the presence of a sealed package, which is opened immediately before the start of the procedure in the presence of the patient, so the possibility of infection is absolutely excluded;
- The device is easy to use, it can be used not only by specialists, but also by ordinary consumers, which is especially important for people with diabetes who have to constantly monitor their blood sugar levels.
Not only children, but also many adults are frightened by the very sight of a medical scarifier. The use of a modern lancet does not cause such fear. The procedure is quick, painless and not accompanied by negative emotions.
Types of lancets
To collect blood from children, only automatic disposable instruments are used. They are selected individually, as they have different sizes. Their characteristic features:
- Disposable feathers (blocked or discarded after blood collection);
- There is an additional protection mechanism;
- Automatic determination of puncture depth;
- A replaceable drum is provided for storing needles.
There are also universal lancets that diabetics use to measure blood glucose using glucometers.
Kinds
Today, pharmacies and online stores offer a wide variety of lancets produced by leading companies in the world. All diversity can be classified taking into account certain parameters. For example, according to their purpose, they are divided into three types.
- Automatic blood collection lancets are easy to use. The procedure takes little time and does not require any additional equipment. Upon contact with the skin, the trigger mechanism is activated, a thin needle quickly and painlessly penetrates the skin and takes a sample, the volume of which is sufficient to obtain accurate, informative results.
- Universal devices are usually used by diabetic patients in conjunction with glucometers. They also do not cause pain and do not leave a wound after the puncture. This lancet is used in conjunction with a special handle (body). Before the procedure, the device must be adjusted taking into account the thickness of the patient’s skin.
- Children's lancets are not only smaller in size. In order to minimize trauma to the skin surface, they are equipped with very sharp and thin needles. The procedure for taking a sample in this case is so short that the baby does not even have time to get scared. These devices are optimal for diagnostics in infants.
The second common way to classify devices is based on the size (diameter and length) of the needle. Taking these parameters into account, the laboratory technician selects a device depending on the patient to be worked with: age, mental characteristics, thickness of the skin, location of the puncture.
- For children, newborns, preschoolers, primary schoolchildren, patients with diabetes mellitus, who are forced to perform the procedure repeatedly, lancets with a needle thickness of 0.25 mm and a length of 1.2 mm are used.
- For glucometers, lancets with needles 1.5 mm long and 0.5 mm in diameter can also be used.
- In cases where it is necessary to obtain a sample for carrying out a general analysis or diagnosing the gas content in the blood, other indicators, when a large amount of material is needed or a deep puncture is required, devices with needles 0.8 mm thick and 1.8 mm long are used.
- The thickness of the skin varies from person to person. In some patients, due to natural characteristics, under the influence of production factors, it becomes very rough, dense, and thick. For such cases, needles with a length of 2.5 mm and a thickness of 0.8 mm are intended.
- In children, especially infants, sometimes it is not possible to take blood from a finger. In this case, the sample is taken from the baby's heel. These lancets use needles with a diameter of 0.8 mm and a length of 2 mm.
If it is necessary to carry out the sample collection procedure on their own, people cannot always choose the right lancet option. In this case, you need to consult your doctor, who will tell you which needles will be optimal in this particular case.
Features of recycling
All consumables for injection procedures and sampling of biomaterials, including capillary blood, must be disposed of after use. In particular, the reuse of disposable lancets in most cases is impossible due to the design features: after performing a puncture and taking a sample, the needle is automatically hidden inside the body and blocked there. This is done in order to prevent the spread of infection. At home, when using universal lancets together with a glucometer, usually only the needles are changed, which are also a source of danger. They should not be thrown into the bin with normal household waste.
In medical institutions, all consumables that were used for collecting and conducting blood tests, syringes and other accessories after use are placed in special tanks for class B medical waste. Before disposal, they are disinfected under high temperature, chemicals or other means. Only after they become safe for people and the environment are they destroyed.