Iron deficiency state (IDS, hyposiderosis) is a lack of total iron in the human body that does not meet current physiological needs. One of the special cases of manifestation of iron deficiency anemia (IDA) is iron deficiency anemia. Iron deficiency anemia is the most common form of anemia , laboratory confirmed by a decrease in hemoglobin content per unit volume of blood. A decrease in hemoglobin and anemia occurs as a result of iron deficiency. IDA is a clinical manifestation of a complete lack of iron reserves in the human body and is accompanied by dysfunction of all organs and systems due to insufficient oxygen supply to cells and a decrease in the synthesis of iron-containing enzymes.
Causes of anemia

In the vast majority of cases (up to 90%), anemia is caused by iron deficiency. Iron is part of hemoglobin and is involved in the process of hematopoiesis. Iron-deficiency anemia
occurs when there is insufficient consumption of iron-containing foods (primarily meat and vegetables). Anemia can also occur with the right diet, for example, if iron is not absorbed by the body due to existing problems with the gastrointestinal tract. Blood loss can also contribute to the development of anemia. However, blood loss does not have to be large. Frequent nosebleeds, bleeding gums, hemorrhoids, and heavy periods can cause anemia.
Possible causes of anemia include a lack of vitamin B 12 or folic acid, but these types of disease are much less common. Hemolytic anemia is also isolated, characterized by increased (faster) destruction of red blood cells.
Anemia can be genetically determined, that is, it can be hereditary.
Hemolytic anemia
DEFINITION, ETIOLOGY and PATHOGENESIStop
Hemolytic anemia (HA) is a heterogeneous group of diseases characterized by abnormal premature breakdown of red blood cells. Hemolysis can occur intravascularly or extravascularly - in the spleen or liver.
1. Hereditary HA - as a result of a genetic intracellular defect:
1) defects in the cell membrane of erythrocytes - congenital spherocytosis, ovalocytosis (elliptocytosis);
2) enzymopathies - deficiency of glucose-6-phosphate dehydrogenase (G-6-PD [G-6-PD]), deficiency of pyruvate kinase (PK);
3) hemoglobinopathies - sickle cell anemia (pathological Hb - HbS); methemoglobinemia;
4) thalassemia - quantitative disorders of the synthesis of globin chains (usually β).
2. Acquired HA - erythrocytes are normal, the cause of decay is external factors, with the exception of paroxysmal nocturnal hemoglobinuria (PNH):
1) immune (anti-erythrocyte antibodies present)
– autoimmune HA with warm antibodies (idiopathic, during other diseases [including SLE, chronic lymphocytic leukemia, non-Hodgkin lymphoma, immunodeficiency], drug-induced [methyldopa, cephalosporins, purine analogues], after organ transplantation or allo-HSCT [if inappropriate blood groups between donor and recipient], after red blood cell transfusion [during or shortly after alloimmunization]);
– autoimmune HA with cold antibodies: cold agglutinin disease (idiopathic; with infection [mycoplasma, Epstein-Bar virus], with lymphomas), as well as paroxysmal cold hemoglobinuria (idiopathic; with an infectious or autoimmune disease, with lymphoproliferative tumors), post-transfusion hemolytic reaction ; hemolytic disease of newborns;
2) non-immune - microangiopathic HA caused by endovascular damage to erythrocytes by fibrin threads, including thrombotic thrombocytopenic purpura [TTP] and hemolytic-uremic syndrome [HUS], causes → section. 15.19.3), disseminated intravascular coagulation, infections (malaria, babesiosis, toxoplasmosis, leishmaniasis, Clostridium perfringens), chemical and physical factors (methemoglobinemia, drugs [mitomycin C, cyclosporine, tacrolimus, ticlopidine, sulfonamides, sulfasalazine, dapsone, platinum derivatives ], drugs [cocaine], metals [lead, copper], animal poisons [Loxosceles spiders, bees, wasps, cobras, snakes], severe burns), PNH, hypersplenism.
CLINICAL PICTURE AND NATURAL COURSE to top
Hereditary forms, as a rule, appear at an earlier age; autoimmune HA is more common in middle-aged and older people. In patients with mild hemolysis, especially with a long course, clinical symptoms of HA are usually absent. General symptoms of anemia usually appear only when Hb levels are <8 g/dL or when anemia develops very quickly. Jaundice appears during periods of increased red blood cell breakdown and is often absent in patients with chronic hemolysis. Enlarged spleen (sometimes also liver) usually occurs in some forms of GA that occur in the presence of a systemic disease (lymphoproliferative or autoimmune). Clinical features of some forms of GA →see. below.
Complications of HA: crises (hemolytic, aplastic [most often caused by infection with parvovirus B19 in hereditary HA]), venous thrombosis with the risk of embolism, cholelithiasis (due to hyperbilirubinemia, with the formation of bilirubin stones), folic acid deficiency (due to increased demand), skin ulceration ( in the case of thrombotic processes in the microcirculatory bed), secondary hemosiderosis → section. 7.9.2.
1. Hereditary microspherocytosis: the most common form among hereditary HA. Characteristic disorders of bone development (in severe forms), splenomegaly, periodically occurring hemolytic and aplastic crises, cholelithiasis.
2. Glucose-6-phosphate dehydrogenase (G-6-PD) deficiency: usually affects men. Manifests itself as an acute hemolytic crisis (sudden jaundice, dark urine, abdominal pain), after taking certain medications (chloroquine, sulfonamides, dapsone, nitrofurantoin, large doses of vitamin C, doxorubicin →also: www.g6pd.org and www.g6pddeficiency.org ) or consumption of food products (seeds of leguminous crops), during infections and stress.
3. Pyruvate kinase (PK) deficiency: the second most common hereditary GA, can occur in adults who, in the presence of a stable clinical condition and normal peripheral blood picture, experience crises due to acute infection, stress or pregnancy.
4. Methemoglobinemia: characterized by the presence of ferric iron in the heme, which does not combine with oxygen; may be congenital (hemoglobin M) or acquired (much more often), caused by compounds that oxidize iron (sodium nitroprusside, phenacetin, sulfonamides, lidocaine, benzocaine, dapsone, rasburicase, nitrates, nitroglycerin, nitric oxide, nitrites, aniline, chlorites); cyanosis occurs when the concentration of methemoglobin (metHb) is >1.5 g/dl; in most patients with the congenital form, the only symptom is cyanosis; in the acquired form, symptoms of anemia occur when metHb levels are >40% of total Hb.
5. Thalassemia: usually splenomegaly, severe GA only in the homozygous form, appears before the age of 1 year.
6. Sickle cell anemia: jaundice, cholelithiasis, growth and developmental delay, cardiomegaly; thrombosis of blood vessels, leading to tissue ischemia with the development of recurrent severe pain in the hands and feet (the most common and earliest symptom), embolization of internal organs, acute chest syndrome, splenomegaly, skin ulcerations in the ankle area, priapism.
7. Autoimmune HA with warm antibodies: the most common acquired HA, with the presence of additional symptoms of the underlying disease (fever, lymphadenopathy, articular syndrome, etc.).
8. Cold agglutinin disease: symptoms of underlying disease (lymphoma or infection), acrocyanosis (purple discoloration of the distal parts of the body after cold exposure), livedo reticularis, pain when swallowing cold foods and drinks. Paroxysmal cold hemoglobinuria (symptoms occur several minutes or hours after cold exposure): pain in the back, lower extremities, abdomen, fever with chills, red or red-brown color of the first portion of urine.
9. PNH: paroxysm of the disease can be caused by infection, stress, physical activity; in addition to symptoms associated with hemolysis (eg, dark urine at night or in the morning), thrombosis (in ≈50% of patients, especially venous in atypical locations) and often symptoms caused by concomitant aplastic anemia or MDS (bleeding, infections).
DIAGNOSTICS up
Additional research methods
1. General analysis of peripheral blood: normocytic and normochromic anemia, and in some cases macrocytosis or microcytic hypochromic anemia (with thalassemia); reticulocytosis, spherocytes in the blood smear and increased MCH and MCHC in spherocytosis and autoimmune GA, Heinz bodies in G-6-PD deficiency and methemoglobinemia, sickle erythrocytes and Howell-Jolly bodies in erythrocytes in sickle cell anemia, echinocytes in PC deficiency, thyroid erythrocytes at thalassemia; fragments of erythrocytes (schizocytes) in microangiopathic HA (hemolytic-uremic syndrome and thrombotic thrombocytopenic purpura); erythroblasts for severe anemia
2. Other blood tests: increased LDH activity, decreased (or undetectable) haptoglobin level, increased unconjugated bilirubin level (usually <4 mg/dL), decreased osmotic resistance of red blood cells (in hereditary microspherocytosis and other GAs that are accompanied by [acquired] spherocytosis ).
3. General urine analysis: increased excretion of urobilinogen, and dark color of urine and a positive benzidine urine test with intravascular hemolysis.
4. Other studies specific to certain forms of GA:
1) hereditary microspherocytosis - positive test with acidified glycerol solution (AGLT), cryohemolysis or eosin-5 maleimide binding test (EMA);
2) G-6-PD deficiency - decreased activity of G-6-PD in erythrocytes (not determined in acute hemolysis);
3) PC deficiency - PC deficiency of erythrocytes, PC gene mutations;
4) methemoglobinemia - increased metHb levels, dark urine, increased excretion of urobilinogen, hemoglobinuria (positive benzidine test) with intravascular hemolysis;
5) thalassemia - electrophoresis shows the absence of HbA and an increased level of HbF;
6) sickle cell anemia - electrophoresis shows the absence of HbA and increased levels of HbS and HbF;
7) autoimmune HA with warm antibodies - positive direct antiglobulin test (with anti-IgG or anti-C3d antibodies, the maximum activity of which is manifested at a temperature of 37 ° C);


9) PNH lack of expression of proteins associated with glycosylphosphatidylinositol (CD55 and CD59) in granulocytes and erythrocytes (according to flow cytometry), which leads to increased sensitivity of cells to the action of complement.
5. Aspiration biopsy and bone marrow trephine biopsy: increased erythropoiesis, often megaloblastic type of hematopoiesis.
6. Imaging methods: enlarged spleen, cholelithiasis (according to ultrasound).
Diagnostic criteria
Anemia of varying degrees, usually normocytic and normochromic (exceptions →see above), with increased serum LDH activity, decreased plasma haptoglobin, increased serum unconjugated bilirubin, and increased reticulocyte counts.
Differential diagnosis
Anemia in chronic diseases, chronic hepatitis, benign hyperbilirubinemia (Gilbert's syndrome), acute blood loss (in acute intravascular hemolysis.
TREATMENT to the top
Instructions general for GA
1. Secondary (symptomatic) HA: the underlying disease should be treated and medications that can cause hemolysis should be discontinued.
2. Transfusion of red blood cells - only if necessary.
3. Chronic HA: folic acid 1 mg/day should be constantly used. Iron supplements only after verification of absolute iron deficiency → section. 15.1.2 (in most cases contraindicated) or the use of drugs that eliminate excess iron → section. 7.9.2; splenectomy - for some severe hereditary HA (microspherocytosis, G-6-PD deficiency, PC deficiency, thalassemia) and glucocorticoid-resistant HA with warm antibodies.
Specific treatment of individual forms of GA
1. Autoimmune anemia with warm antibodies: use of corticosteroids (eg prednisone 1 mg/kg/day po) for several weeks, then the dose is gradually reduced to the minimum, which ensures remission and a negative Coombs reaction. Hb levels usually increase after 1–3 weeks. treatment. For more severe hemolysis, it is recommended to start with intravenous methylprednisolone on the 1st day, 1500 mg, on the 2nd day - 1000 mg, on the 3rd day - 500 mg, and from the 4th day use prednisone 1-2 mg/kg /day In case of resistance to GCS, their intolerance, or the need to use GCS at a dose of >15 mg/day, after several months of starting therapy, splenectomy is indicated (effective in 60–70%). If there are contraindications to splenectomy or there is no effect from the operation → rituximab should be used in 4 doses of 375 mg/m2 or 100 mg/m2 at weekly intervals. In patients who do not improve with the above treatment, consider other immunosuppressive therapy (azathioprine 1–3 mg/kg/day, cyclophosphamide 100 mg/day po or 500–700 mg/day every 3–4 weeks IV , cyclosporine - the dose is selected in accordance with the concentration of the drug in the blood serum, mycophenolate mofetil 0.5–1.0 g/day po). In patients resistant to GCS, especially in hemolytic crisis, plasmapheresis can be performed or immunoglobulin can be administered intravenously (1 g/kg for 2 days or 2 g/kg for one day).
2. Cold agglutinin disease: in most cases, recommendations to avoid hypothermia and wear warm clothing are sufficient. Red blood cell transfusions and fluid infusions should be performed after rewarming. Transfusion of blood products with high levels of complement components (FFP and TM) should be avoided. In severe cases, rituximab 375 mg/m2 IV is prescribed 1 time per week. within 4 weeks. (most effective in monotherapy or in combination with fludarabine). It is possible to prescribe cyclophosphamide 100 mg/day. p/o or chlorambucil. GCS and splenectomy are usually ineffective. If immediate reduction in antibody titer is necessary, plasmapheresis should be used. Paroxysmal cold hemoglobinuria: low temperatures should be avoided and transfusions of warmed red blood cells should be performed; consider hormone therapy.
3. Methemoglobinemia: it is necessary to discontinue drugs that cause methemoglobinemia. In severe cases (metHb >20%), it is recommended to administer methylene blue 1–2 mg/kg (1% solution in 0.9% NaCl) IV over 5 minutes and consider hyperbaric oxygen therapy. For life-threatening methemoglobinemia (metHb >50%), perform an exchange transfusion. For chronic methemoglobinemia → ascorbic acid 0.3–1.0 g/day. p/o in several doses and riboflavin 20–30 mg/day. By; for exacerbations, methylene blue 100–300 mg/day. By.
4. Thalassemia β: In addition to the above joint recommendations, prescribe vitamin C and zinc. In severe cases, the possibility of allogeneic hematopoietic stem cell transplantation (allo-HSCT) is considered.
5. Sickle cell anemia: in most cases, symptomatic treatment (hydration, analgesics and anticoagulants, physical therapy). RBC transfusions reduce HbS concentrations to ≤30% via hemodilution. Treatment with hydroxyurea 15–20 mg/kg/day should be considered (inhibits HbS polymerization and increases HbF synthesis). In selected cases, consider the need for allo-HSCT.
6. PNH: in the classic form (>50% of the granulocyte population without GPI-AP; overt intravascular hemolysis occurs), patients with clinically significant symptoms and complications require treatment. The drug of choice is eculizumab. The only method that allows for cure (eradication of the PNH clone) is allo-HSCT. In case of thrombotic complications → standard therapy, secondary prevention with vitamin K antagonists, primary prevention with heparin. For severe hemolysis, consider prednisone 40–60 mg/day. By. In patients with moderate to severe anemia, danazol 200–600 mg/day may be considered. divided into 3 doses. In non-classical forms, tactics depend on the concomitant bone marrow failure syndrome (aplastic anemia → section 15.1.7, MDS → section 15.4).
Symptoms of anemia
Lack of hemoglobin leads to oxygen starvation, manifested by symptoms typical of anemia such as:
General weakness
With anemia, muscle tissue does not receive sufficient nutrition. The patient feels constantly tired, he does not have enough strength for normal life activities.
Drowsiness
The body lacks strength, which means it needs additional rest. Drowsiness develops. A person suffering from anemia is almost never alert; as a rule, he wants to sleep.
Pallor
Pale skin due to anemia is caused by a decrease in the number of red blood cells (erythrocytes) in the blood.
Dizziness
With anemia, the brain also receives insufficient nutrition. This may cause dizziness.
flickering
The flickering of “flies” before the eyes is caused by insufficient nutrition of the structures of the visual apparatus.
Fainting
If the decrease in hemoglobin is significant, fainting is possible - episodes of loss of consciousness.
Headache
With anemia, headaches are often observed.
More about the symptom
Cardiopalmus
You may experience palpitations with little physical activity or at rest.
More about the symptom
Dyspnea
Shortness of breath with anemia is caused by the fact that the body tries to compensate for the lack of oxygen by increasing its supply. Breathing becomes more frequent.
More about the symptom
Methods for diagnosing anemia
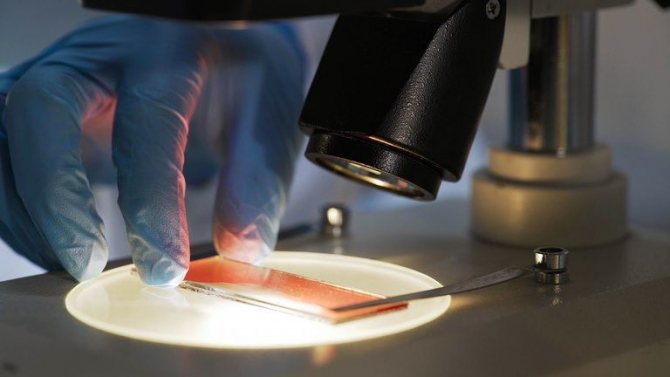
Anemia is diagnosed based on laboratory tests.
General blood analysis
A complete clinical blood test is the basic test for determining anemia. For a more detailed diagnosis of certain types of anemia, additional studies may be prescribed.
More information about the diagnostic method
Sign up for diagnostics To accurately diagnose the disease, make an appointment with specialists from the Family Doctor network.
Anemia Treatment Methods
Treatment of anemia is aimed, first of all, at identifying and eliminating the cause of the disease. In case of detected iron deficiency (vitamin B12, folic acid), replacement therapy is carried out with drugs that compensate for this type of deficiency. A special diet high in essential substances is also prescribed.
Doctor visit
If you are concerned about weakness, dizziness, drowsiness and other symptoms that suggest anemia, we recommend that you consult a general practitioner or family doctor at any of the clinics of JSC “Family Doctor”. The high professionalism of our specialists and modern equipment allow us to effectively treat anemia, including during pregnancy, breastfeeding and other periods that require a special approach.
Make an appointment Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
Rate how useful the material was
thank you for rating
What are the symptoms of anemia (anemia)?
Anemia leads to a pronounced decrease in performance in both men and women, and the risk of mortality sharply increases, including from myocardial infarction, stroke, coronary heart disease, etc. Almost every person can develop deficiency anemia. What are the symptoms of anemia (anemia)
? As a rule, attention is drawn to:
- pale skin,
- increased fatigue,
- dyspnea,
- drowsiness,
- fainting,
- cardiopalmus.
May be:
- hair loss,
- gum problems,
- perversion of taste (desire to eat chalk, aversion to certain foods).
Premature babies, children under 1 year of age, pregnant and lactating women will have iron deficiency
in the body due to its increased need (iron deficiency anemia). In pregnant and breastfeeding women, the symptoms of anemia are the same as in ordinary people. rentgirl.co.nz

How to suspect anemia in a child?
When should one suspect anemia (anemia) in a child?
If your baby has:
- poor appetite
- no interest in games
- cold and damp palms and feet,
- the child is often sick for a long time, is capricious,
It is necessary to undergo general clinical tests as soon as possible (complete blood count, feces for worm eggs, general urine test) and consult a pediatrician.