Video-EEG monitoring is a study in which synchronous recording of EEG, video and audio data on the motor and behavioral activity of the subject is carried out over several hours with sleep registration, therefore it is often called video sleep monitoring, or EEG-night monitoring. This study is of great importance for the diagnosis of various paroxysmal conditions and disorders in neurology, primarily in the differential diagnosis of epilepsy.
➥ More details: EEG monitoring for epilepsy
The wide polymorphism of clinical manifestations and variability of circadian rhythms of epileptic seizures create difficulties in the timely detection and adequate diagnosis of this disease, leading to diagnostic errors, incorrect treatment, or unreasonable drug burden on the patient.
For a neurologist-epileptologist, it is extremely important to assess the bioelectrical activity of the brain both in the interictal period and at the moment of paroxysm. A standard EEG recording in a state of wakefulness lasting up to 20 minutes reveals epileptic activity in 24.5% of patients suffering from epilepsy. In the remaining patients, despite ongoing seizures, epileptic activity was not detected. In 29% of patients with pathology detected on the EEG, longer recordings, including sleep EEG, revealed additional foci of epileptic activity and revealed various epileptic EEG patterns that were not identified during a standard EEG study. All this became the reason for the intensive development of a new direction in clinical neurophysiology - video-EEG monitoring.
Story
In the last two decades, with the development of computer technology, video-EEG monitoring has become a standard in epileptology. Based on the same principles as conventional EEG, video-EEG monitoring has its own characteristics, primarily associated with the enormous recording duration, covering various stages of the patient’s daily activity during wakefulness and sleep.
The method of video-EEG monitoring did not arise on its own, but was the result of a long, step-by-step improvement of the method of clinical electroencephalography. Monitoring developed and took shape gradually, first of all, as the technical component improved, and also as doctors realized the diagnostic significance of analyzing the bioelectrical activity of the brain in all phases of its functioning. Let us consider the main milestones in the development of the method.
In 1934, spouses Eric and Erna Gibbs (Gibbs) from Harvard Medical School created a neurophysiological laboratory where they recorded ictal and interictal activity in patients, using initially a single-channel and later a three-channel ink-writing electroencephalograph. In 1937, they created the first classification of EEG disorders. In 1939, based on research carried out by the Gibbs couple and co-authored by Alfred L. Loomis, a work was published on long-term EEG recordings of wakefulness and sleep. Based on these studies, the Gibbs formulated the most important principle of monitoring studies: “One minute of EEG recording during sleep can tell more about the epilepsy process than an entire hour of EEG recording of the waking brain.”
Alfred Loomis, working in New York by 1938, created an electroencephalographic laboratory consisting of several consecutive rooms. In a separate shielded chamber there was a patient’s bed and part of the EEG equipment, in another there were devices that made it possible to record the patient’s respiratory, cardiac and motor activity, and in a remote “control room” there was a six-channel recording device equipped with a roller paper feed mechanism, which made it possible to carry out long-term recordings with various stress tests, including photo and phonostimulation. In addition, the Loomis system was equipped with a camera. The equipment he developed made it possible to record and systematize the bioelectrical activity of the brain during night sleep.
In 1938, Robert Schwab from Harvard used the “photographic method”: he used two cameras in conjunction with an electroencephalograph. The use of marks to synchronize photographs subsequently made it possible to edit a single film. This technique can be considered as one of the predecessors of video-EEG monitoring.
In 1966, RS Goldensohn and R. Koehle from the Neurological Institute of New York first presented simultaneous EEG recording and video transmission to a television screen. Subsequently, video recording was used.
The fruitful scientific union between the neurophysiologist Jasper and the neurosurgeon Penfield enriched both neurophysiology and epileptology. In 1939, Jasper and Penfield established an electroencephalographic laboratory at the Montreal Institute. Their laboratory was equipped with soundproof, shielded chambers that had a special window for systematic monitoring of the patient's condition during recording. In 1949, Jasper and John Hahn introduced a technique for recording EEG, combined with recording clinical events on a movie camera.
In 1969, JR Stevens reported the first use of radiotelemetric long-term EEG monitoring in a patient with epilepsy.
Advantage of EEG
EEG has an important advantage: it shows brain activity in real time, because the electrical signal travels almost at the speed of light. The time resolution of other methods is much worse - on the order of seconds, at best, fractions of tenths of seconds, and with their help only relatively slow processes can be observed. Most often, 19 electrodes are used for recording, which make up the standard installation in Russia, as well as in many other countries. Sometimes it is permissible to reduce the number of electrodes when recording in children under one year old or with a small head size, but it is advisable to use at least 16 channels.
What can be analyzed using EEG?
- presence or absence of a basic rhythm;
- background rhythm surrounding the main rhythm;
- changes in rhythms during special tests;
- changes in brain activity during various functional states, for example, when a person’s level of wakefulness changes, he begins to doze off or falls asleep.
Indications and contraindications for the video-EEG monitoring method
Indications
- Epileptology: Diagnosis of epilepsies and epileptic syndromes;
- Paroxysmal conditions of unknown origin, raising suspicion of the presence of epilepsy.
- Pharmacoresistant seizures (in order to identify pseudoepileptic paroxysms or clarify the form of epilepsy);
- Monitoring the effectiveness of treatment;
- Drug remission (objective statement of remission);
- Preparation for discontinuation of anticonvulsant therapy;
- Presurgical examination;
- Subclinical epileptic activity;
- Progressive cognitive and behavioral disorders in children;
- First seizure.
- Localization of the epileptogenic zone in the surgical treatment of drug-resistant structural epilepsy;
- Delayed mental and speech development in children;
- Differential diagnosis of syncope and epileptic seizures;
Contraindications
There are no contraindications to video-EEG.
Rhythms on the EEG of the brain
The main rhythm in the EEG of the brain after 7-8 years is the alpha rhythm. In younger children, the main rhythm is the rhythms of a lower frequency - theta and delta - range. Moreover, each of the rhythms has its own characteristic spatial organization and response to various external stimuli.
In various diseases, the ratio of these rhythms and their localization change; pathological forms of activity may occur, the main of which are epileptiform activity and slowing.
Logistics of the method
Video-EEG monitoring room
Scheme of organization of a video-EEG monitoring room
A video-EEG monitoring room is usually part of the neurophysiological department of a medical institution, usually of a psychoneurological or neurosurgical profile.
The staff of the video-EEG monitoring room consists of a functional diagnostics doctor and several operators (usually with a nurse certificate in the specialty of functional diagnostics). The operator’s responsibilities include performing the examination itself with functional tests, recording paroxysmal and atypical events with markers in the recording, as well as first aid to the patient in the event of an epileptic attack. The research carried out is recorded in the journal of completed research. The doctor’s responsibilities include collecting a medical history from the patient, filling out a special questionnaire, analyzing the data obtained and drawing up a medical report. Before starting the study, the patient is asked to sign an informed consent for the examination.
The video-EEG monitoring room (laboratory) consists of one or more soundproof rooms for patients and a work area for staff: monitoring operators and neurophysiologists (Fig. 1).
The wards are equipped with comfortable beds for those being examined. The room may also have a chair or bed for an accompanying person. The monitoring room should provide the ability to be completely darkened, preferably with continuously adjustable lighting. Of course, the room must be maintained at a comfortable temperature and have good ventilation. The ward can be equipped with an observation window. Next to the room there should be a bathroom combined with a shower.
Equipment for video-EEG monitoring room
Currently, the video-EEG system is based on powerful computer systems; synchronization of the EEG and video signal is carried out in digital format, which significantly expands the possibilities for processing results; the recording duration is practically unlimited and can be more than 1 week of continuous recording.
The basis of the video-EEG system is a multi-channel signal amplifier, which has the ability to record 19-32-64-128-channel EEG, ECG channel, respiration sensor, electromyographic and electrooculographic channels. The corresponding recording sensors are connected to the amplifier. For long-term recording, EEG electrodes are attached using a special cap or adhesive paste. The design of the electrode system allows the patient to move around the room, does not cause inconvenience and makes the examination comfortable.
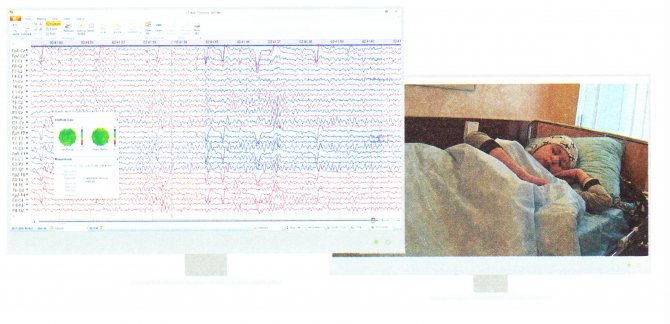
Fig.2. Workplace of video-EEG monitoring operator
The video image is recorded using digital video cameras; their number can be arbitrary; most systems provide the possibility of using 1-2 cameras: a general-view dome camera and a high-resolution camera for monitoring and video recording the activity of facial muscles. A dome PTZ video camera with infrared illumination, a built-in microphone and remote control is mounted in the room opposite the patient’s bed. A speaker is also mounted on the wall to transmit information to the patient and an emergency call button for medical staff. A button for recording a paroxysmal event is placed near the patient’s hand, which could be the development of an aura, the onset of an attack, or any other sudden unusual change in well-being without clinical manifestations that the patient has realized. If the button is pressed, a marker will be recorded on the EEG indicating the duration of this episode (Fig. 2).
The main part of the equipment is installed in the operator room: a computer for recording and subsequent processing of data, or several computers when deploying several patient rooms. These computers are necessarily equipped with uninterruptible power supplies to prevent loss of survey data in the event of a power failure in the electrical network. In the operator's room, EEG data and video signals from cameras are displayed on separate computer screens. The most important factor in the effectiveness of monitoring is the most accurate synchronization of the EEG with the video signal and audio, and therefore it is important to comply with the system requirements recommended by the equipment manufacturer for the computers used for recording and video cameras certified for this device.
The control room also needs to be equipped with comfortable chairs for operators to comfortably carry out long-term night recordings and communication means for an emergency call to a resuscitator or orderlies if it is necessary to restrain the patient (for example, in the event of the development of a psychomotor attack with aggressive behavior).
Via a local network, all received information is transferred to the resident’s room on the doctor’s computer. In this case, it is desirable that the equipment also allows viewing the current recording without interrupting the study.
When performing outpatient video-EEG monitoring or when performing monitoring in a regular ward, the room is equipped with a portable dome PTZ video camera with IR illumination, a built-in microphone and remote control. An autonomous recorder is placed on the body or directly on the EEG helmet, allowing recording directly to the built-in memory card or in real time via wireless communication channels (usually Bluetooth or WiFi), transferring the results to a remote data storage. With this type of research, the premises for doctors and operators can be located at any distance from the recording site, making it possible to quickly monitor the condition of the electrodes and provide assistance to the patient.
The results are processed by studying synchronous EEG and video images; the image scrolling speed is chosen arbitrarily. A prerequisite is perfect synchronization of the video image and EEG in time. The EEG processing program includes spectral and coherence analysis capabilities, three-dimensional dipole localization programs, and other computer analysis options.
There are mobile video-EEG monitoring systems that allow you to conduct research at the patient’s home or travel to other medical institutions. However, the technical capabilities of these systems are significantly inferior to stationary ones. Due to the possibility of provoking severe epileptic seizures, there are restrictions regarding provoking loads on the patient during recording at home. Currently, systems from Nicolett (USA), Grass Telefactor (USA), NPKF Medicom MTD (Taganrog, Russia) are presented on the Russian market; systems from other manufacturers are being prepared for release.
Description of the method. Rules of the event. Diagnostic algorithm
A video-EEG study includes all standard functional loads (photostimulation, hyperventilation); it is possible to simulate situations that provoke paroxysm (sleep deprivation, working on a computer, watching TV, etc.). After performing functional loads, the patient, while in the ward, leads a normal lifestyle. Restrictions apply only to movements - they are possible within the ward. It is highly advisable to record EEG during sleep. Premedication before the study, as a rule, is not carried out, since the administration of drugs not included in the treatment regimen can change the EEG picture, and this will not allow assessing the true parameters of the bioelectrical activity of the brain. It is not recommended to cancel or change the treatment regimen on the day of the study - this will also not allow you to evaluate the effects of therapy.
The staff of the video-EEG monitoring room consists of a functional diagnostics doctor and several operators (usually with a nurse certificate in the specialty of functional diagnostics). The operator’s responsibilities include performing the examination itself with functional tests, recording paroxysmal and atypical events with markers in the recording, as well as first aid to the patient in the event of an epileptic attack. The research carried out is recorded in the journal of completed research. The doctor's responsibilities include:
- collecting anamnesis from the patient;
- filling out a special questionnaire by the patient;
- analysis of the obtained data;
- drawing up a medical report.
Before starting the study, the patient is asked to sign an informed consent for the examination.
Technique and methodology of monitoring research
Clinical diagnostic tasks of video-EEG monitoring can be divided into “daytime” and nighttime sleep monitoring. The total duration of daytime video-EEG monitoring can range from 2-3 to 12 hours. The study should be carried out, if possible, in the first half of the day. The purpose of video-EEG monitoring is to search for epileptic correlates. Video-EEG monitoring uses a fairly large number of electrodes to accurately localize the irritation zone, and with an ictal pattern, the seizure onset zone.
The night before video-EEG monitoring, the patient’s sleep duration should be reduced to 2-3 hours, since nighttime sleep deprivation is one of the powerful “probes” for disavowing covert epileptic processes. The patient before the examination and on the day of the examination takes all prescribed antiepileptic drugs according to the previously prescribed regimen. Reducing the dose of antiepileptic drugs or their short-term withdrawal is also a provocative load. Studies on the background of reducing the dose of antiepileptic drugs, as a rule, should be carried out in a hospital setting, since in the case of a low concentration of the drug in the blood of a patient with sleep deprivation, functional tests can provoke an epileptic attack. The use of any sedatives as part of premedication is not carried out, as it can significantly distort the results of the examination.
The video-EEG monitoring technique includes continuous EEG recording and ECG recording in one of the standard leads. In addition, if indicated, monitoring can be supplemented by recording an electrooculogram and recording breathing (chest excursion or air movement through the nasal passages). During the examination, the patient is in a bed in a supine position, usually in a loose sports suit (pajamas), not covered with a blanket, which ensures complete fixation of the motor components of the attack. Considering the duration of recording and multiple changes in the position of the patient’s body and head during monitoring, increased requirements are placed on the placement and fixation of EEG electrodes. For this purpose, an EEG helmet with integrated electrodes is used. Currently, it is extremely rare, mainly for duck research, that cup electrodes are used, placed using a special adhesive conductive paste and cleol.
Daytime video-EEG monitoring includes three sequential stages of the study:
- recording EEG while awake with standard functional tests (similar to ambulatory EEG);
- EEG monitoring when falling asleep and during sleep;
- awakening, registration of EEG of wakefulness after awakening.
Of course, each stage combines not only EEG monitoring, but also synchronous audio and video recording of the patient’s behavior. The duration of registration of passive wakefulness is usually 30-40 minutes. This time is necessary for recording the background EEG and performing standard functional tests (opening and closing the eyes, photostimulation, hyperventilation). In some cases, additional tests are performed, recommended by an epileptologist, based on the clinical picture of seizures. So, for example, if it is indicated that watching TV or reading provokes seizures, appropriate tests can be performed. After recording the EEG of passive wakefulness, the patient is asked to take a comfortable position and try to fall asleep. Next, the sleep is recorded. 15-20 minutes before the end of the study, the patient is woken up and an EEG recording of passive wakefulness after sleep is performed.
When carrying out night EEG monitoring, the recording duration is 8-12 hours. Under the instructions of the epileptologist, the patient is woken up at about 5-6 a.m. and the EEG of passive wakefulness is recorded with standard stress tests, after which the patient falls asleep again with awakening 20-30 minutes before the end of the recording, when the waking EEG is recorded again and functional tests are performed.











