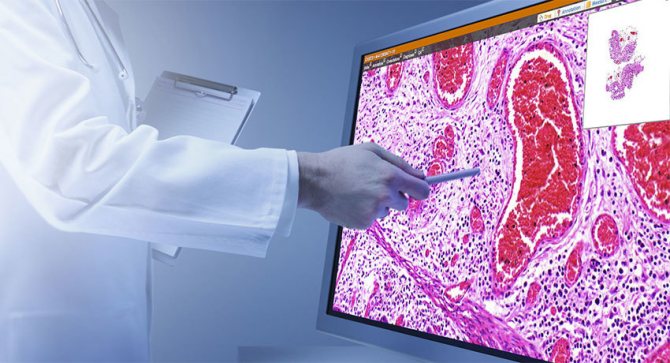
Histological examination is the examination of body tissue samples under a microscope. It is widely used in modern medicine and helps to establish an accurate diagnosis for a number of diseases, primarily cancer. In most cases, this is the only way to definitively determine whether a tumor detected during an ultrasound, CT, MRI or endoscopic examination is malignant.
Our expert in this field:
Gotovtseva Vladlena Alexandrovna
Oncologist
Call the doctor
Histological studies appeared and were introduced into clinical practice quite a long time ago. Over time, technology has improved, and new methods for studying tissue samples have emerged. Many processes have been automated, digital technologies have helped to significantly improve the quality of images, sending them to colleagues from other clinics and laboratories with one click of a button. Thanks to the rapid development of molecular biology and genetics, immunohistochemical tests, chromosome studies and genetic code sequences have become available.
Clinic Medicine 24/7 cooperates with leading laboratories that conduct histological studies and all types of molecular genetic diagnostics. Analyzes are performed by the best pathologists using the latest equipment. This helps to establish the most accurate diagnosis and prescribe optimal treatment.
Indications
The main indication for histological examination is suspicion of a malignant tumor. The transformation of a normal cell into a cancerous one begins with disturbances at the molecular level. Certain mutations occur in genes, because of this the structure of the corresponding proteins changes, or they begin to be produced in too large quantities. As a result, the appearance of the cells and the architecture (structure) of the tissue change. These changes can be detected by examining the tissue under a microscope. Histological examination helps to establish a final diagnosis, determine the histological type of malignant tumor, the stage of the disease and prescribe the correct treatment.
In addition to oncological diseases, histological studies help in diagnosing the following pathologies:
- benign neoplasms, precancerous conditions;
- liver diseases, such as cirrhosis;
- peptic ulcer of the stomach, duodenum;
- kidney diseases;
- some infectious, inflammatory processes;
- autoimmune pathologies, systemic vasculitis, connective tissue diseases;
- after organ transplantation, histological examination helps to determine whether rejection has begun or whether the disease has recurred.
For many diseases, histological studies help not only to correctly establish the diagnosis, but also to monitor the effectiveness of treatment when it is already carried out.
How is material obtained for histological examination?
A tissue sample is obtained through a procedure called a biopsy. It comes in different types:
- Excision - the pathological formation is completely removed. Such operations are both therapeutic and diagnostic.
- Incisional - part of the pathological formation is removed.
- Endoscopic - material for research is obtained during endoscopic examinations of hollow organs, for example, the stomach, intestines, bladder, uterus.
- Razor - the doctor uses a sharp blade to shave off a growth that rises above the surface of the skin.
- Thick-needle ( trephine biopsy ) - obtaining a column of tissue using a trephine, a special instrument in the form of a tube with a pointed edge.
- Fine needle aspiration - using a needle connected to a syringe.
- Pipelle biopsy is the collection of tissue samples from the uterine cavity using a tube with a side hole at the end, inside of which there is a piston to create negative pressure.
- Diagnostic curettage of the body and cervix.
- Fine-needle endoscopic biopsy under EUS guidance - obtaining material using a needle inserted through the wall of an organ during an endoscopic examination.
- Smears, prints, scrapings.
Not all of these procedures make it possible to obtain organ tissue with preserved structure. Sometimes individual cells are enough for diagnosis - their study is called a cytological study. The doctor chooses the appropriate type of biopsy, depending on the nature of the disease, size, location of the pathological formation and other factors.
Skin biopsy
The final diagnosis of melanoma or skin cancer can only be confirmed by a biopsy - the removal of a small amount of tissue for examination under a microscope. The choice of a specific biopsy technique depends on the size, location of the suspicious tumor and some other factors.

Biopsy of a skin lesion
Biopsy of moles is performed under local anesthesia; a small scar may remain after the procedure.
Types of biopsy:
- Razor. It is performed when the risk of a mole degenerating into melanoma is minimal. This type of biopsy helps identify not only melanoma, but also other skin diseases. Using a scalpel, the doctor cuts off the epidermis and superficial layers of the dermis in thin layers.
- Puncture. Allows you to obtain a larger sample from the mole tissue. A special tool is inserted into the skin with a screwing motion, capturing all 3 layers of it.
- Excision. It is performed if the doctor suspects that melanoma has grown through all layers of the skin. The entire tumor along with a section of skin is excised with a scalpel, after which the edges of the wound are sutured.
- Incisional. Simultaneously with tissue collection for examination, part of the mole is removed.

Lymph node biopsy
If melanoma is suspected of spreading from the primary site through the lymphatic system, a biopsy of sentinel and regional lymph nodes is necessary.
A fine-needle aspiration biopsy is performed under ultrasound or CT guidance with a fine-needle syringe, and a tissue sample is taken from large lymph nodes. This technique is gentle for the patient, but when using it it is not always possible to take a sufficient amount of tissue for analysis.
Surgical biopsy replaces fine-needle aspiration; during it, the enlarged lymph node is removed through a skin incision.
A sentinel lymph node biopsy can detect metastases in regional lymph nodes. The sentinel node can be detected using the radioisotope method - a small amount of radioactive drug is injected into the melanoma area, and an hour later the doctor examines the lymph nodes using a radioactivity detector. The node in which the maximum level of the radioisotope is detected is excised and taken for examination. If there is an enlarged lymph node near the melanoma, a biopsy is performed; in this case, a sentinel search is not carried out.
If no melanoma cells can be found in the sentinel lymph node, it means that the tumor has not yet spread. In this case, the study of the lymphatic system is stopped. If malignant cells are found in the sentinel lymph node, lymph node dissection is performed - removing the remaining lymph nodes and assessing their condition. Based on the results of the examination, the doctor decides on further tactics for managing the patient.
Book a consultation 24 hours a day
+7+7+78
How are histological studies performed?
In order for tissue to be examined under a microscope, it must be prepared in a special way. They begin by treating the sample with a fixing solution, otherwise the cells will be destroyed by their own enzymes. Then the fabric is given density by filling it with paraffin - a paraffin block is obtained.
In such a block there are many layers of cells that overlap each other and block light. Because of this, under a microscope it will not be possible to examine the structure of the tissue and individual cells. To make this possible, the blocks are cut into very thin, from 1 to 8 microns, layers using a special tool - a microtome. Then they carry out staining - treatment with special chemicals that react with various molecules in the cells and color different structures.
After this, a pathologist (also called a pathologist, clinical morphologist, histopathologist) examines the samples under a microscope and draws up a conclusion. The entire process takes about 7–10 days.
There are cases when the result of a histological examination is needed urgently. For example, surgeons are performing an operation and they need information right now to make the right decision. In such situations, accelerated preparation is carried out: the tissue sample is frozen, cut with a microtome and immediately examined under a microscope.
Request a call back. We work around the clock
Main goals of pathohistological examination
A pathological examination begins with the removal of a small sample of internal tissue from the patient’s body that requires examination for abnormalities. This analysis makes it possible to accurately determine the structure of tissues, the pathological processes that occur in them, and also monitor the effect of treatment. Tissue is taken during surgery or through a biopsy and then examined under a microscope.
Diagnostics can be prescribed for a number of reasons:
- accurate diagnosis when the clinical picture is unclear;
- detection of tumors at an early stage of their development;
- determination of the prevalence of the malignant process;
- dynamic control over the development of the disease;
- determining the need for surgical intervention and its volume;
- conducting a differential examination of detected pathological abnormalities;
- clarification of the development of the tumor process, proliferation, enlargement.
In modern medical practice, cancer patients are not treated with chemotherapy or radiation without prior histological analysis of tissue. In addition, a detailed study is necessary to identify the slightest deviations in the development of the disease and treatment.
Carrying out a biopsy and tissue analysis plays an important role in the selection of effective treatment in various branches of medicine: hematology, nephrology, gastroenterology, gynecology, pulmonology, otorhinolaryngology, urology, etc.
In addition, pathohistological examination is often used in thoracic and abdominal surgery. Types of biopsy according to the method of collecting biomaterials for examination Typically, material for analysis is taken under visual control; for this, an ultrasound machine or surgical access to tissue can be used.
The following may be removed as biomaterial:
- muscle fibers;
- individual parts or entire organs;
- The lymph nodes;
- leather;
- Bone marrow;
- selected fabrics;
- areas of the mucous membrane of the stomach, bronchi, duodenum or other parts of the intestine;
- elements of the prostate gland or cervix, etc.
A biopsy can be performed using the open method (external), when biomaterial for study is taken through smears and swabs. It can also be diagnostic and therapeutic. The latter option involves the complete removal of pathological tissues with their subsequent study.
Find out the price
Find out the price
Error! Please fill in all required fields
Thank you! We will contact you shortly
✕
Scientists distinguish the following types of biopsy:
- Puncture - to take samples, a tissue or organ is punctured with a special biopsy needle.
- Excision - taking biomaterial is performed by excision of the entire organ or pathological formation during surgery.
- Pincer - tissues are taken by pinching from internal systems. Used for colonoscopy, gastroscopy and other diagnostic methods.
- Incisional - excision of a certain part of tissue affected by pathological changes.
- Trepene biopsy - taking bone tissue samples using a special thick needle.
- Curettage is the taking of samples from cavities and the female uterus.
- Aspiration - taking biomaterial with a thin needle by sucking out fluids from hollow areas of the body.
The biopsy method is used not only for histological analysis (study of tissue sections), but also for cytological analysis (study of cellular structures).
Resection margin
After radical surgery for oncological diseases, it is often necessary to evaluate the resection margin, and this can also be done during histological examination:
- A negative resection margin means that there are no tumor cells near the cut line. This means that the tumor was completely removed and the risk of recurrence is minimal.
- A positive resection margin indicates that tumor cells were found near the cut line. Some of the tumor tissue may remain in the body, and the disease may recur. In such cases, repeated surgery or radiation therapy and antitumor drugs are prescribed.
Grade of differentiation/grade of malignancy
The degree of differentiation and degree of malignancy characterize the aggressiveness of the tumor and influence the choice of treatment tactics and prognosis.
The degree of differentiation is indicated by the letter G:
- High degree of differentiation (G1): tumor tissue closely resembles normal tissue.
- Moderate differentiation (G2): tumor tissue is more different from normal, but still similar to it.
- Low grade of differentiation (G3): The tumor tissue is very different from normal tissue.
- Undifferentiated tumors (G4): cancer cells completely lose the features of normal ones, they all become the same, and are located chaotically.
The lower the degree of differentiation, the higher the degree of malignancy. Tumors G3 and G4 are the most aggressive, quickly invade surrounding tissues and metastasize.
Pathological staging
In oncology, there are such concepts as clinical and pathomorphological stages of cancer. These terms are often used for malignant breast tumors. The clinical stage is determined based on clinical examination data, and the pathomorphological stage is determined based on the results of histological examination of removed tissues. The pathomorphological stage is more accurate; once it is established, the treatment program can change significantly.
What affects the accuracy of histological examination?
Histological examination is a very accurate diagnostic method. But still, in rare cases, errors occur. They are associated with various factors:
- Lack of experience on the part of the doctor who collects the tissue sample.
- The biopsy failed to obtain the required amount of tissue, or it was obtained from the wrong location.
- Violation of the conditions of transportation of biomaterial, technologies for the preparation of histological preparations.
- Insufficient level of qualification of the pathologist who studies the tissue under a microscope.
To get the most accurate and reliable result, you need to pay attention to the choice of the clinic where the biopsy will be performed. It is important that experienced doctors work in it and modern equipment is used. You need to ask which pathology laboratories the clinic cooperates with. If doubts creep in about the accuracy of the diagnosis, you can order a review of histological preparations in another laboratory. Most often, this does not require a repeat biopsy: the material is stored in the laboratory where the study was carried out, and can be obtained by filling out an application. If an error occurred during collection of material, the procedure will have to be repeated.
We will call you back
Leave your phone number
Tasks
Histological analysis has great advantages over x-rays and ultrasound.
His tasks in oncology (and not only in it) are clearly outlined. Here are some of them:
- Confirmation of a preliminary diagnosis or its refutation;
- Detection of cancer at an early stage;
- Distinguishing the nature of tumors;
- Establishing the stage and dynamics of the disease;
- Checking the effectiveness of previously prescribed treatment, etc.
We will not talk about the biopsy procedure itself here, since there are articles on this topic on our website, but we emphasize: the accuracy of the research results largely depends on the biopsy procedure.
What other tests are performed in the pathology laboratory?
In addition to histological examination, additional tests can be performed to help clarify the type of disease, assess the prognosis, and select the correct treatment:
- Immunohistochemical analysis (immunohistochemistry) helps detect specific proteins using labeled antibodies.
- Fluorescence in situ hybridization (FISH) is a method for identifying defective genes using DNA probes.
- Polymerase chain reaction (PCR) is a study during which the desired DNA fragment is copied many times using enzymes, after which it becomes available for study.
- Next generation sequencing (NGS) is a technique that allows you to completely “read” the genetic code and detect various mutations.
These studies play a particularly significant role in oncology: they help to select the right combinations of anticancer drugs, prescribe effective targeted therapy, and immunotherapy. All types of molecular genetic diagnostics are available at the Medicine 24/7 clinic.
The material was prepared by oncologist, surgeon at the Medicine 24/7 clinic, Valentin Valentinovich Semushin.