What does an ovarian cyst look like and what is it? A cyst is a formation on the ovary that is filled with some kind of content. There are many varieties of this pathology, including:
- Cystadenoma. It can be serous, serous-papillary (prone to malignancy) and mucinous. Such a cyst requires only surgical intervention, since it cannot be treated with medication and cannot disappear on its own;
- Endometrioid ovarian cyst. Formed as a result of endometriosis. It is treated promptly with subsequent normalization of hormonal levels;
- Dermoid cyst. Contains debris from teeth, skin and hair. It is large in size. Most often it requires surgical intervention.
- Follicular. Formed in the absence of ovulation and follicle growth. It can resolve on its own, as it is a functional cyst;
- Corpus luteum cyst. It disappears on its own after several menstrual cycles. Also refers to functional cysts;
- Paraovarian cyst. It is located between the ovary and the fallopian tubes and is a fluid-filled formation;
The oncology department of Yusupovskaya employs doctors who specialize in the treatment of benign and malignant tumors of the pelvic organs. The hospital uses all methods for diagnosing ovarian cysts. The department of the Yusupov Hospital is equipped with European equipment, comfortable rooms that allow you to stay in the hospital until the body fully recovers. Conservative therapy and modern types of surgical treatment are used to treat tumor diseases.
Tumor marker CA-125 in ovarian cyst: norm and pathology
Modern oncology has the latest diagnostic methods that allow early detection of various pathologies in the human body. These include a blood test to determine tumor markers, which indicate the presence of tumors. It also reveals the nature of the formation and helps plan treatment in a timely manner.
Tumor marker CA-125 for ovarian cysts has an important role in a woman’s life, because it indicates the presence of a tumor not only of the uterine appendages, but also of other organs.
Ca-125 with an ovarian cyst is normal from 0 to 30 IU/ml. At the same time, 0-15 IU/ml is absolutely healthy, and 15-30 IU/ml is the upper limit of the acceptable value.
The borderline value is 30-40 IU/ml - observed during pregnancy or menopause.
Elevated CA-125 with an ovarian cyst - more than 40 IU/ml. Indicates an ovarian cyst, inflammatory causes, endometriosis, liver diseases (40–100 IU/ml). Over 100 IU/ml - possible development of an oncological process.
Most women with pathology of the appendages, in whose analyzes CA-125 is elevated due to an ovarian cyst, begin to read reviews on forums and thereby set themselves up for the worst scenario. A tumor marker test alone will not make a definitive diagnosis. Such a study only signals the onset of an inflammatory process. A tumor marker shows a discrepancy with the norm, which is not always the cause of the disease. The numbers in the analysis will not accurately indicate the reason for the deviation, so additional research is necessary.
The importance of tumor marker diagnostics lies in identifying the disease even before the appearance of pronounced symptoms.
Diagnostic methods
When contacting a doctor, the first step is to study the clinical picture of the disease and the woman’s medical history.

Next, a gynecological examination is performed on a chair. If the size of the cyst is small, the doctor may not notice it. In this case, a study using an ultrasound sensor will help make a diagnosis. It shows neoplasms of any parameters, allows you to determine their type, location, structure. An examination is carried out through the vagina, which allows you to get closer to the ovaries and get a larger picture. On the monitor, an anechoic ovarian cyst appears as a dark spot.
Tumor marker HE 4
Tumor marker HE 4 for ovarian cysts is used for screening diagnosis and evaluation of the effectiveness of treatment of ovarian tumors.
As a result of numerous studies, the purpose of which was to compare the sensitivity and specificity of tumor markers HE4 and CA-125 in women with various forms of benign and malignant neoplasms of the reproductive organs. All scientific papers provided percentage data that indicated that HE 4 has higher sensitivity and specificity compared to CA-125. This is an innovative discovery in the diagnosis of tumor diseases of the internal genital organs.
Types of cysts
Cystadenomas of an anechoic structure that occur inside or near the ovary are of the following types:
- follicular. Formed from a follicle. This element must rupture, then during ovulation the egg is released. In the presence of a follicular ovarian cyst, rupture does not occur;
- formation of the corpus luteum. Appear when fluid accumulates at the site where the egg exits the follicle;
- serous. They are smooth-walled growths formed from serous tissue that covers the ovaries and contains fluid inside;
- paraovarian. These forms of ovarian cysts are dense, form near the reproductive organs, and can reach large sizes.
Single and multiple, single-chamber and double-chamber cysts are also identified. The type of tumor is determined by performing an ultrasound of the pelvic organs.
What does an ovarian cyst look like on an ultrasound?
An ultrasound examination of a functional (anechoic) ovarian cyst has thin, smooth walls, without internal inclusions, acoustic enhancement behind the formation, and is more than 30 mm in size. Such neoplasms are most often single-chamber, round or oval in shape, the boundaries are clear and even, and healthy ovarian tissue can be seen along the periphery.
Ultrasound of an ovarian cyst: on what day of the cycle should it be done? Ultrasound examination is best done from 2 to 5 days after the end of menstruation. On other days, visibility may be poorer and the structure of the ovary may be altered.
What to do after detecting a functional ovarian cyst on ultrasound?
- Functional cysts up to 3 cm at a young age are the norm → do not require treatment or observation;
- Cysts up to 7 cm in the reproductive period → ultrasound monitoring after the end of menstruation;
- Neoplasms up to 7 cm in postmenopause are almost always benign → Ultrasound observation;
- Ovarian cysts larger than 7 cm are difficult to evaluate using ultrasound → MRI is recommended.
A corpus luteum cyst on ultrasound has characteristic signs - a dense wall and a “ring of fire” with color Doppler mapping, up to 5 cm in size.
On ultrasound, hemorrhagic ovarian cysts look like single-chamber formations with hyperechoic inclusions. There is always no blood flow in the lumen of the cyst. Sometimes levels and an openwork mesh of fibrin threads are visualized. A hemorrhagic cyst has a thick wall and can resemble a huge tumor.
Tactics for patients with hemorrhagic ovarian cysts:
- Cysts less than 5 cm at a young age → do not require control;
- Formations larger than 5 cm in the reproductive period → Ultrasound control after menstruation;
- Hemorrhagic neoplasms in menopause → MRI of ovarian cysts is recommended.
A paraovarian cyst is an anechoic thin-walled neoplasm that is enclosed between the layers of the broad ligament of the uterus. Usually has a size of less than 5 cm. To distinguish a paraovarian cyst from a follicular one, it is necessary to separate the cyst from the ovary with a sensor.
An endometrioid ovarian cyst on ultrasound is a round hypoechoic formation with a double contour, having a wall 2-8 mm thick. There is no blood flow and dense inclusions in the lumen.
Dermoid cyst on ultrasound - an acoustic shadow is detected, indicating the presence of bone density elements.
Ovarian cystadenoma is a multi-chamber formation with tuberous edges, the contents are hypo- and anechoic, the walls are thickened.
Signs of a malignant ovarian cyst on ultrasound:
- Diameter more than 7 cm;
- Thick and lumpy cyst walls, with a developed vascular network;
- Intracystic septa larger than 3 mm, with abundant blood flow;
- Inside the cyst, huge formations with blood flow are determined;
- Ascites, lymphadenopathy and metastases.
Ultrasound of the ovaries, inflammation of cysts and formations
Ovarian examination
Author: rasurgut from 05/30/2015, 01:37, views: 7,050 19 The ovaries
(ovaria) are a paired female reproductive gland located in the pelvic cavity.
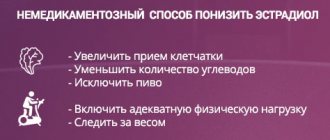
An egg matures in the ovary, which is released into the abdominal cavity at the time of ovulation, and then descends through the fallopian tube into the uterine cavity and hormones are synthesized that enter directly into the blood. Generative function The ovaries are the place where female germ cells - oocytes - develop and mature. Hormonal function The main hormones of the ovary are estrogens, progesterone and androgens. From androgens (testosterone and androstenedione) estrogens (estradiol and estrone, respectively) are formed in the cells of the dominant follicle. Progesterone is produced in the cells of the corpus luteum. Estrogens have a wide range of biological effects: they promote the growth and development of the external and internal genital organs, during puberty they stimulate the growth of mammary glands, the growth and maturation of bones, ensure the formation of the skeleton and the redistribution of adipose tissue according to the female type. Androgens promote bone growth and maturation, pubic and armpit hair growth. Estrogens and progesterone cause cyclic changes in the mucous membrane of the uterus and vagina, and the epithelium of the mammary glands. Progesterone plays a decisive role in preparing the uterus and mammary glands for pregnancy, childbirth and lactation. Secretion of estrogen and progesterone in the first 6-8 weeks. pregnancy in the ovary increases sharply, then decreases, and hormonal “provision” of pregnancy from 12-14 weeks. carried out by the placenta. In addition to sex hormones, inhibin, relaxin, oxytocin, and prostaglandins are produced in the ovary. The most common reason for referral to ultrasound is the detection during a gynecological examination of a tumor-like formation in the area of the appendages of an inflammatory or non-inflammatory nature. Inflammation of the ovary (oophoritis), which can be combined with inflammation of the fallopian tube (salpingo-oophoritis) and is accompanied by the formation of a tumor-like conglomerate - tubo-ovarian formation, accompanied by poor circulation and pain. In some cases, a picture of an acute abdomen develops. Cysts and other tumor-like processes of the ovaries are often combined with menstrual irregularities, amenorrhea, dysfunctional uterine bleeding, infertility, excessive hair growth (hirsutism), obesity, as well as sweating, hot flashes to the head and upper half of the body, palpitations and other signs characteristic of menopausal syndrome . Disorders of puberty and infertility, ovarian hyperinhibition syndromes due to hormonal contraceptive medications. Suspicion of ovarian cancer. Ultrasound assessment of the ovaries Location
The ovaries are determined in the immediate vicinity of the uterus in the form of small, oval-shaped, echo-dense (light) formations of medium intensity with characteristic structureless inclusions, representing an echographic image of the follicular apparatus.
The right and left ovaries are most often located asymmetrically with respect to the uterus, usually 20 - 40 mm from its corners. Often one of the ovaries is adjacent to the lateral surface of the uterus or is located behind it. This situation can be considered as a sign of an inflammatory process, but it also occurs in healthy women. form
is an elongated oval (ellipsoidal) shape of the ovaries; changes in shape indicate difficulties with visualization or pathological processes.
Contours
The contours are clear, even, caused by the tunica albuginea (capsule) of the ovary.
It should be noted that in healthy women this capsule is not visualized; thickening of the capsule has important diagnostic value in some diseases and infertility. Dimensions
The ovary of an adult woman is 2.5-3.5 cm long, 1.5-2.5 cm wide, 1-1.5 cm thick, weighs 5-8 g. The right ovary is always larger than the left.
The volume of the ovary normally does not exceed 9 cm3. However, depending on the phase of the menstrual cycle, their sizes may vary. By the middle of the cycle they increase, after the cessation of menstruation the size of the ovaries decreases. The size of the ovaries in girls is of utmost importance; by the 10th year of life, the weight of the ovary reaches 2 g.
Mixed
echogenicity Structure
In the mature ovary, there are three clearly demarcated parts: the hilum, the cortex and the medulla.
In the cortical layer, which occupies most of the ovary, there are follicles (of varying degrees of maturity and atretic), yellow and whitish bodies. Therefore, the structure of the ovary is normally heterogeneous; the homogeneous structure of the ovary is characteristic of age-related (menopausal) changes and pathology. During menopause, the density of the ovary increases, and the structure becomes homogeneous; their size decreases accordingly, so images of the ovaries in women during this period cannot always be obtained, which is a variant of the norm. The epididymis (epophoron) and periovary (paroophoron) are not visualized on ultrasound. Normally, in some cases it is possible to obtain an image of the own ovarian ligaments, which are located between the angle of the uterus and the ovary in the form of a cylindrical structure of low echo density. Assessment of the presence of fluid in the retrouterine space, depending on the period of the cycle, is used to register completed ovulation. The follicular ultrasound apparatus
provides a unique opportunity to monitor the physiological changes occurring in the ovaries during the menstrual cycle - follicle maturation, ovulation, the emergence, development and regression of the corpus luteum.
Folliculometry, analysis of the dynamics of follicle maturation, registration of ovulation and qualitative assessment of the readiness of the endometrium (inner layer of the uterus) are of paramount importance in determining the factors of infertility. In the first days after menstruation, in the early phase of menstruation, from 10 to 20 follicles begin to develop. The bulk of them will soon undergo changes. From 8 to 12 days it is possible to identify the dominant follicle, the size of which exceeds 15 mm during this period. The development of the remaining follicles stops during this period. The dominant follicle continues to grow by an average of 2-3 mm per day and by the time of ovulation its diameter reaches 18-24 mm. During one menstrual cycle, only one follicle completes development; it is called dominant. Follicles that have not reached the preovulatory stage undergo reverse development (atresia). In place of the ovulated follicle, a corpus luteum is formed, the color of which is due to the luteinization of granulosa cells - the accumulation of lipid inclusions in them. If fertilization does not occur, the corpus luteum is replaced by connective tissue, resulting in the formation of a whitish body. In the reproductive period of life (16-45 years), the processes of growth, maturation of follicles and formation of the corpus luteum have a clear cyclical nature. Ovulation occurs in the middle of the menstrual cycle - in most cases on the 13-14th day from the beginning of the development of the dominant follicle. From the age of 40, the frequency of menstrual cycles without ovulation and cycles with the formation of an incomplete corpus luteum increases. In premenopause (at the age of 45-50 years), anovulatory menstrual cycles and cycles with the persistence of a non-ovulated follicle predominate; processes of follicular atresia intensify. In postmenopause, the size of the ovary decreases, its weight is about 3 g, the tunica albuginea shrinks, the cortex becomes thinner, interstitial cells are replaced by connective tissue. Due to the gradual decline of the hormonal function of the ovaries, the presence of single, small follicles during the first 5 years after the cessation of menstruation should not be regarded as a disorder. After 5 years of menopause, follicles are not detected, and their detection should cause some caution. Cysts and other tumor-like processes
Follicular ovarian cyst.
It is formed as a result of the accumulation of follicular fluid in an unovulated follicle, and is more often observed during puberty and in young women. It is a thin-walled single-chamber formation, the diameter of which rarely exceeds 8 cm. Small follicular cysts have moderate hormonal activity. A follicular cyst with a diameter of up to 4-6 cm often does not appear clinically and in most cases, its reverse development occurs within one and a half to two months. With hormonally active cysts, hyperestrogenism and resulting menstrual cycle disorders are possible: acyclic uterine bleeding in women of reproductive age or premature sexual development in girls in the first decade of life. When the diameter of the follicular cyst is 8 cm or more, torsion of the cyst pedicle may occur, accompanied by impaired circulation and necrosis of ovarian tissue, and (or) rupture of the cyst. In these cases, a picture of acute pain syndrome develops. Corpus luteum cyst Forms at the site of a non-regressed corpus luteum, in the center of which, as a result of circulatory disorders, fluid with a small admixture of blood accumulates. The diameter of the cyst usually does not exceed 6-8 cm. The corpus luteum cyst, as a rule, is asymptomatic and undergoes reverse development within 2-3 months. Complications include torsion of the cyst stalk and rupture of the cyst as a result of hemorrhage into its cavity, accompanied by a picture of an acute abdomen. Simple ovarian cyst Cystic formations, the inner surface of which is devoid of epithelial lining, can develop from follicular ovarian cysts and small cysts. The diameter of simple ovarian cysts usually does not exceed 6-10 cm. They do not manifest themselves clinically. Superficial epithelial inclusion cysts are tense, fluid formations from the epithelium covering the ovary, occurring in old age. Their sizes do not exceed 2-3 cm. These cysts do not appear clinically and do not require treatment. Ultrasound signs On ultrasound, all cysts are an anechoic /dark/, round formation with a thin wall and homogeneous content. Additional criteria for an ultrasound diagnosis of a “cyst”, as opposed to a “formation”, may be clear and even contours, correct shape, and a pseudo-enhancement effect. Sometimes a fine suspension (blood) is detected in the corpus luteum cyst and luteoma. The cyst has a clear connection with the body of the ovary. It is often not possible to determine the origin of the cyst by ultrasound examination and the true diagnosis is established only by histological examination. Therefore, regardless of the opinion of the ultrasound doctor, all cysts require dynamic observation, examination for tumor markers and mandatory monitoring. Criteria for ultrasound identification of ovarian cancer
Ultrasound signs in the presence of which a suspicion of malignancy arises are varied and controversial. Despite the fact that there is no single position on this issue, there are generally accepted changes characteristic of malignancy - “.. all types of cystic formations with a “homogeneous echo-negative or echo-positive” structure, “heterogeneous” structure reliably prevail among descriptions of malignant neoplasms, and the type “ heterogeneous undifferentiated structure" in most cases turns out to be advanced cancer." These include: a fuzzy, uneven and tuberous contour, the presence of a solid focus and tissue inclusions in the cavity of the cyst under study, mainly of the vegetation type with the presence of internal vessels, the heterogeneous structure and thickness of the wall of the space-occupying formation (pronounced fragmentary thickening of the walls and septa of the cystic formation, pronounced calcification or heterogeneous areas calcium deposits, wall sclerosis) asymmetrical enlargement (by more than 10%) of the contralateral ovary change from oval to spherical shape of the ovary the presence of free fluid (ascites) in the abdominal cavity Study of blood flow and scanning in the Color Doppler mode significantly “... expands the capabilities of ultrasound diagnostics, because before In total, CDK helps to differentiate vascular, hypo- and avascular structures": for the majority of malignant neoplasms of the ovaries it turned out to be characteristic: disordered central blood flow, the presence of blood flow in papillary growths, a decrease in peripheral resistance in the vessels of malignant neoplasms, high blood flow velocity
More details
- 60
Category: Ultrasound of ovaries
MRI of ovarian cyst
On MRI, Graafian follicles appear as hyperintense formations with thin walls, which are surrounded by ovarian stroma, which gives a not very intense signal.
Hemorrhagic cysts are characterized by high signal intensity; a component with high signal characteristics (fat, blood, etc.) is visualized. With fat suppression, the signal intensity does not decrease, which confirms the presence of hemorrhagic fluid.
The contents of an endometrioid cyst on MRI are manifested by increased signal intensity. Remains hyperintense, unlike teratomas.
Ovarian dermoid cyst is a cystic formation with hyperintense signal containing septa. In fat-suppressing mode, a decrease in signal intensity is determined.
Possible complications
The danger of a cyst lies in its complications. If the pathology is not treated, the anechoic formation in the ovary will grow, causing harm to the woman’s body.
The most serious complications requiring immediate medical attention and surgery are the following:
- torsion of the cyst stalk. Patients suffer from severe acute pain in the lower abdomen. Due to twisting, the tumor does not receive nutrients, which leads to the death of the tumor tissue, and then the appendages;
- education gap. During this process, the entire contents of the cyst are released into the ovarian cavity. This causes the development of peritonitis. Due to the fact that the fluid may contain blood inclusions, an inflammatory process may occur in the ovary;
- infertility or termination of pregnancy. Long-term absence of therapy for the tumor leads to disruption of the ovaries, which take a leading part in conceiving a child;
- neoplastic cancer. Not so often, but there are cases of a cyst transforming into oncology, which subsequently affects other organs.
These pathological conditions require urgent surgery.
Ovarian cyst or pregnancy
Most often, women confuse pregnancy with a follicular cyst or corpus luteum cyst. The signs of such cysts are very similar to the early symptoms of pregnancy. The hCG level increases with an ovarian cyst, as with pregnancy, so at the first sign you should consult a gynecologist.
The Oncology Clinic of the Yusupov Hospital offers a wide range of surgical interventions in the field of gynecology. Our gynecological oncologists are true professionals in their field, using in their practice only the latest treatment protocols that meet international standards.
Thanks to the qualified specialists of the Yusupov Hospital and modern European equipment, you will receive high-quality specialized advice. The medical staff guarantees an individual approach to each patient, as well as comfortable conditions of stay in the hospital. The clinic’s doctors will be happy to provide you with detailed information about ovarian cysts, treatment features, diagnostic ultrasound, as well as prices for services. You can make an appointment and consultation by phone.
Anechoic inclusion during pregnancy
Anechoic formations are also diagnosed in pregnant women. If ovulation has passed, and such an inclusion is detected on ultrasound, then this is most likely the corpus luteum. In cases where there is also a delay in menstruation, one can indirectly assume pregnancy.
If the pregnancy test has two stripes, there is an anechoic inclusion, but the fetus is not yet visible on ultrasound; this is the luteal body. It is needed to create the necessary conditions for the baby to grow and develop.
The luteal body will be active until 12-16 weeks of pregnancy, after which the placenta takes over all functions.
In rare cases, dermoid cysts and others are diagnosed during pregnancy. The uterus gradually grows, so it puts pressure on neighboring organs, displacing them. If the cyst has a leg, this is fraught with its torsion, respectively, necrosis or rupture of the membrane.
If a malignant formation or a tumor that is growing rapidly is diagnosed, a decision will most likely be made on surgical intervention. The choice of removing such a cyst will depend on its type, size, and gestational age. If the size does not exceed 10 cm and the period is up to 18 weeks, then the laparoscopic method is used. If the period is more than 18 weeks - laparotomy.
If endometrioma is diagnosed, its removal can be postponed until the birth of the child, provided that the cyst does not receive menstrual blood and does not grow. If a woman undergoes a caesarean section, both operations can be combined.
How is the treatment carried out?
Depending on the nature of the tumor, the patient is prescribed appropriate treatment.
Organic inclusions and paravarial tumors are often treated surgically followed by hormonal therapy.
It is important to establish the cause of these violations and eliminate its influence in the future.

floors
Functional cysts usually do not require treatment. If they begin to manifest themselves clinically, the patient is prescribed hormonal correction, which involves temporarily shutting down the ovaries.
Surgery for functional cysts is performed extremely rarely.
Traditional methods
Non-traditional treatment methods boil down to the use of herbal medicines to regulate hormonal levels.
Remedies such as hogweed, clary sage, red brush and rhodiola can affect natural hormonal levels.
Non-traditional treatment methods have success with functional cysts and sometimes help with parovarian formation. If we are talking about organic tumors, then no grandmother’s recipes will help.
Ask a question to an expert Doctors strongly do not recommend self-medication or taking any traditional medicines. Treatment of pathology must be carried out after establishing the cause of its occurrence and nature.