Types of myelocytes
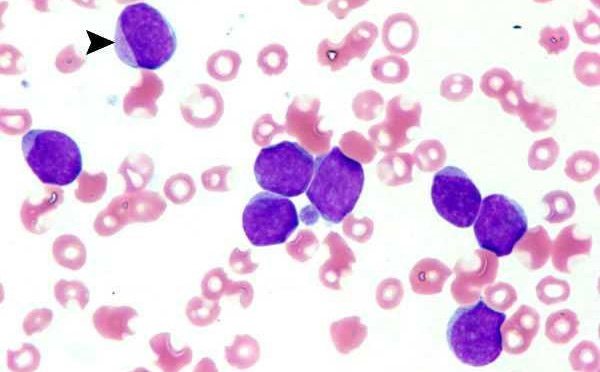
Myelocyte in peripheral blood smear
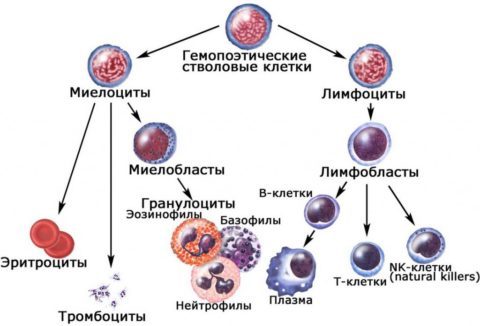
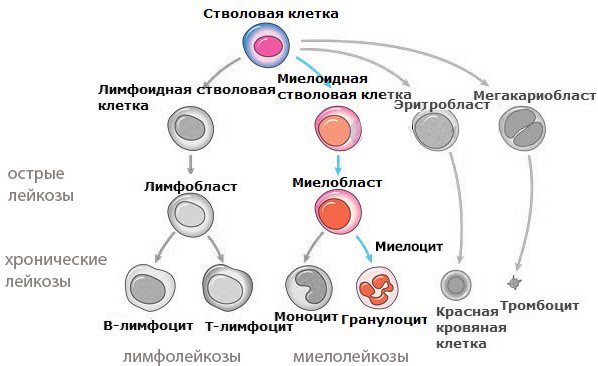
Myelocytes are the precursor cells of mature granulocytes, a type of white blood cell.
The formation of myelocytes is an intermediate stage of granulocytopoiesis, which begins with the mitotic division of a stem cell.
In order to fully understand what myelocytes are and what place they occupy in hematopoiesis, it is necessary to indicate all the forms of cells of the granulocytic lineage of hematopoiesis:
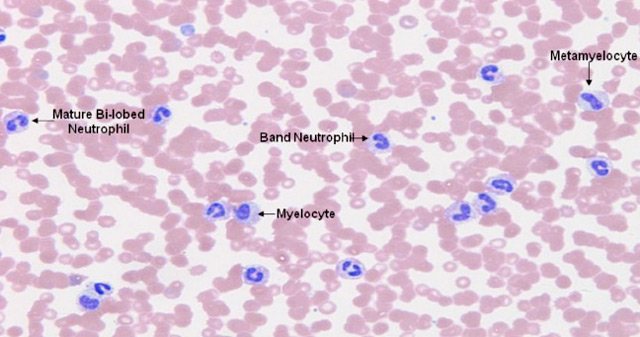
- Myeloblasts are cells that arise from the division of a colony-forming stem cell. Myeloblasts lose pluripotency - the ability to differentiate into any other types of cells. Their main task is to ensure normal maturation of granulocytes.
- Promyelocytes are the largest cells in all stages of granulocyte formation. Already at this stage of maturation, primary granules appear in the cells, which divide promyelocytes into eosinophilic, basophilic and neutrophilic.
- Myelocytes - are formed after the third division of promyelocytes. At this stage of maturation, the granularity of the cells (inclusions) becomes strictly specific (secondary), which makes it possible to clearly distinguish future neutrophils, basophils and eosinophils. Myelocytes are actively dividing cells. The physiological activity and functionality of granulocytes depends on the completeness of myelocyte maturation.
- Metamyelocytes (young leukocytes) - such cells have a low ability to divide. Thanks to them, the final stage of granulocyte maturation occurs. The nucleus of metamyelocytes undergoes changes, dividing the cells into two large groups - segmented and band.
- Granulocytes are the result of granulocytopoiesis. Such cells are called polymorphonuclear, since the cell type depends on their granularity.
Thus, myelocytes are the cells that determine the full growth of mature granulocytes. They belong to granular leukocytes and differentiate into three main types of white blood cells:
- neutrophils,
- eosinophils,
- basophils.
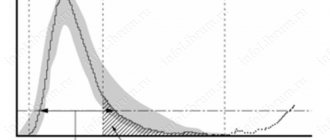
Norms of myelocytes in the bone marrow
Blood cell maturation
Since immature forms of leukocytes must undergo all stages of maturation in the bone marrow, they should normally be present only in the bone marrow puncture.
If a person is healthy, then there is no reason for immature forms of blood cells to enter the systemic circulation.
To assess the consistency of granulocytopoiesis and all hematopoiesis in general, a research method such as bone marrow puncture (sternal puncture, trephine biopsy) is used.
Normally, the granulocytic (myelocytic) lineage of hematopoiesis will give the following indicators when assessing the myelogram:
| Cellular composition of the bone marrow (granulocytopoiesis) | Quantity, % |
| Undifferentiated blast cells | 0,1-1,1 |
| Myeloblasts | 0,2-1,7 |
| Promyelocytes | 1,0-4,1 |
| Myelocytes | 6,9-12,2 |
| Metamyelocytes | 8,0-14,9 |
| Rod | 12,8-23,7 |
| Segmented | 13,1-24,1 |
| Neutrophil Maturation Index | 0,5-0,9 |
| All eosinophils | 0,5-5,8 |
| Basophils | 0-0,5 |
Bone marrow assessment
Obviously, the word “normal” can only be applied to the bone marrow, since myelocytes a priori cannot be present in the blood. And they are elevated there only for certain reasons, and not just like that. Therefore, further we will talk about the place of myelocytes in the bone marrow.
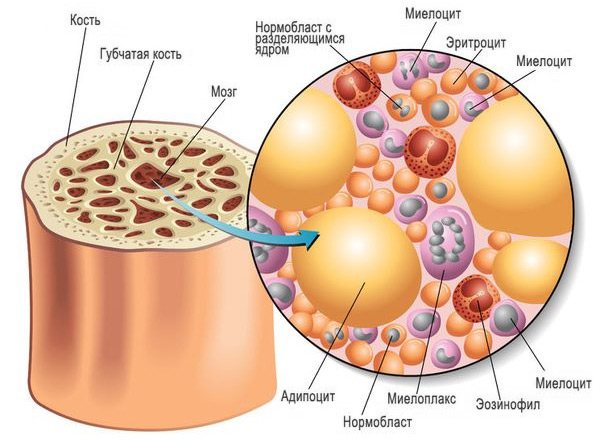
Currently, a bone marrow biopsy and its examination (cytological analysis) is a mandatory procedure if the development of hematological pathology is suspected. Morphological characteristics of the bone marrow after testing are compared with peripheral blood parameters.
It should be noted that when examining the bone marrow (myelogram), doctors consider both generations of myelocytes together, without dividing them into daughter and maternal, since such a division has absolutely no meaning for either normality or pathology.
The norm of myelocytes in the bone marrow ranges from 7 to 12.2%. The table below will help tell you about the norms of other participants in hematopoiesis, which originated from a white sprout.
Table: normal cellular composition of bone marrow (white lineage of hematopoiesis)
| Bone marrow elements | Limits of normal values,% | Average values,% |
| Reticular cells (reticular stroma cells) | 0,1 – 1,6 | 0,9 |
| Blasts | 0,1 – 1,1 | 0,6 |
| Myeloblasts | 0,2 – 1,7 | 1,0 |
| Neutrophils: - promyelocytes - myelocytes - metamyelocytes - band - segmented | 1,0 – 4,1 7,0 – 12,2 8,0 – 15,0 12,8 – 23,7 13,1 – 24,1 | 2,5 9,6 11,5 18,2 18,6 |
| All neutrophil elements | 52,7 – 68, 9 | 60,8 |
| Neutrophil Maturation Index | 0,5 – 0,9 | — |
| Eosinophils (all generations) | 0,5 – 5,8 | 3,2 |
| Basophils | 0 – 0,5 | 0,2 |
| Lymphocytes | 4,3 – 13,7 | 9,0 |
| Monocytes | 0,7 – 3,1 | 1,9 |
| Plasma cells | 0,1 – 1,8 | 0,9 |
Basophilic and eosinophilic myeloblasts in healthy bone marrow, as a rule, are not detected (they are difficult to recognize), but they become quite noticeable with a high eosinophilic reaction or chronic myeloid leukemia. Approximately the same thing happens with promyelocytes - the young cells that strive to become neutrophils show themselves the most.
As for myelocytes (eosinophilic, basophilic and neutrophilic), the situation here changes somewhat if there are no complaints about the main hematopoietic organ. The eosinophilic myelocyte, although the nucleus is similar to the neutrophil, is distinguished by a dense granularity that fills the entire cytoplasm; the basophilic myelocyte is also easily recognized; it is the first to acquire a specific granularity that sparsely covers the cytoplasm. When a pathological process arises in the bone marrow, representatives of 3 generations of myelocytes are difficult to distinguish from each other and all resemble neutrophils.
At the metamyelocyte stage, the cells have already “decided” in their “profession”, so it is not difficult for a specialist who knows their characteristics and main features to understand “who is who”. Meanwhile, a description of the nucleus, cytoplasm and other characteristics is unlikely to interest the reader; it is difficult to understand all this, especially if there is no microscope nearby and the cell cannot be seen with one’s own eyes. Therefore, you should not waste time; it would be more useful to talk about those situations that can really worry a person, for example, about the appearance of myelocytes in a child or their presence during pregnancy in a woman.
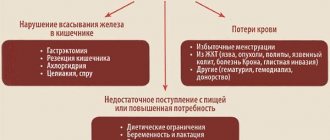
Causes of appearance in the blood

Severe infection may lead to the appearance of myelocytes
In a healthy person, there should be no myelocytes or other immature cells of the myelocytic lineage of hematopoiesis in the blood test. Even minor concentrations of dividing and maturing cells are considered a variant of the pathological condition.
The detection of juvenile forms of granulocytes indicates that the body is at risk and is struggling with one of the following diseases or pathological processes:
- acute bacterial and viral infections, most often complicated by purulent inflammation. These may be purulent tonsillitis, other severe infections of the ENT organs, acute pyelonephritis, pneumonia, cholera, sepsis, scarlet fever, tuberculosis, typhoid fever, brucellosis, paratyphoid fever, measles, mumps, rubella, etc.
- conditions after severe infectious and inflammatory processes;
- appendicitis and other acute surgical pathology;
- gangrene;
- severe burn disease;
- strokes, heart attacks;
- acute blood loss of any origin;
- metastasis to the bone marrow;
- tumor collapse syndrome;
- consequences of chemotherapy, radiation treatment;
- long-term use of cytostatic, immunosuppressive medications;
- lead poisoning;
- alcoholism;
- all types of coma;
- acidosis;
- shock;
- heavy and constant physical activity;
- many types of anemia;
- leukemia;
- myeloid leukemia;
- deficiency of cyanocobalamin and/or folic acid.
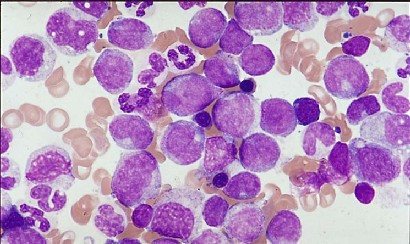
Blast crisis on blood smear
If the concentration of blast cells in the blood is increased slightly - up to 2% of the total leukocyte mass - then we are talking about chronic leukemia.
High values of blasts in the blood are a sign of severe disruptions in the activity of the bone marrow, which indicates acute leukemia.
An excess of the number of blast cells in the blood of more than 5% indicates the development of a blast crisis in patients with chronic myeloid leukemia, as well as the terminal stage in oncological pathology.
The detection of myelocytes, promyelocytes and metamyelocytes in the blood of no more than 5% does not indicate the presence of hematological diseases, but still indicates the presence of certain health difficulties.
But a significant increase from 10% and above is a very unfavorable indicator; it is a marker of myeloproliferative diseases - chronic leukemia, which originate from young cells of the myeloid lineage of hematopoiesis.
The most common reason for the detection of myelocytes and other maturing cells of leukocytopoiesis is chronic myeloid leukemia, the substrate of which is predominantly immature neutrophil myelocytes and other young forms.
At the initial stages of the disease, the growth of myelocytes is not pronounced. The progression of myeloid leukemia is accompanied by a significant increase in myelocytes in the blood, as well as mature eosinophils and basophils. A sharp increase in immature neutrophils, i.e., neutrophilic myelocytes, is an extremely unfavorable sign that worsens the course of leukemia and the prognosis.
“Illegal” penetration into peripheral blood
However, there are situations when cells that still need to “grow and develop” prematurely leave their “native homes”. And if normally the appearance of blast cells in the peripheral blood is out of the question - they are rare “guests” in the bloodstream, then under certain pathological conditions, contrary to natural prohibition, both of them still enter the bloodstream.
Blasts and myeloblasts are slightly increased (up to 2% of the total leukocyte population) in chronic forms of leukemia . And a huge number of blasts (blastemia) generally indicates serious changes in the hematopoietic organs and is one of the significant signs of acute leukemia, the form of which will subsequently be clarified by other methods.
Of particular concern is the number of blasts crossing the 5% limit in the blood of a patient suffering from chronic myeloid leukemia - this may indicate the onset of a blast crisis and the final stage of the tumor process.
myeloblasts in the blood
The presence of propromyelocytes, myelocytes and the closest to mature forms - metamyelocytes, although not such a terrible indicator of white blood, still indicate a serious pathology. An increase in the number of these cells to 5% is more often caused by non-hematological pathology:
- A severe infectious disease of any origin: both bacterial (mainly) and viral;
- Development of a septic condition;
- Various types of intoxication (bacterial, alcoholic, salts of heavy metals);
- Tumor (malignant) process;
- Chemotherapy and radiation therapy;
- Taking certain medications (analgesics, immunomodulators);
- Acute blood loss;
- Coma, shock;
- Violation of acid-base balance;
- Excessive physical activity.
presence of myelocytes and metamyelocytes in the blood
Meanwhile, a significant jump in myelocytes, pro- and meta- (up to 10–25%), is usually observed in the case of the formation of myeloproliferative diseases, which are the most basic reasons for the exit of maturing forms from the bone marrow and their free movement through the blood vessels.
“Young and early”...
The collective name “myeloproliferative tumors” refers to chronic leukemias that are formed at the level of the youngest precursors of myelopoiesis, all of whose offspring - granulocytes, monocytes, erythrokaryocytes, megakaryocytes (except lymphocytes) belong to the tumor clone.
Chronic myeloid leukemia, opening the list of myeloproliferative processes, acts as a typical representative of tumors that arise from early (very young) precursors that differentiate through myelopoiesis to a mature state.
The cellular substrate of myeloid leukemia originates from the white germ of hematopoiesis and is represented by transitional (maturing) forms of granulocytes, mainly neutrophils. This suggests that important cells such as neutrophils, which play such an important role in protecting the body, suffer the most, which makes it clear why this disease is so difficult to treat and ultimately fatal.
At the beginning of the disease, a shift to myelocytes and promyelocytes is noted in the blood, although their number at first is still insignificant. In addition to single promyelocytes and a slightly larger number of myelocytes, representatives of other cell populations can be found in the blood (erythrokaryocytes, counted in units, and high thrombocytosis).
The advanced stage of the disease gives a significant rejuvenation of the leukocyte formula and, at the same time, in addition to myelocytes, the absolute values and percentage of already mature forms of the granulocyte series in the blood are often increased: eosinophils or basophils (less often, both of them - “basophilic-eosinophilic association”). It should be noted that a sharp increase in the number of immature neutrophils is a very, very unfavorable sign that complicates the course of the disease and prognosis.
Myelocytes in children and pregnant women

Myelocytes can appear when the immune defense in children is reduced
The detection in the blood of any cell that has not completely completed its differentiation during granulocytopoiesis indicates that the bone marrow has become activated in response to some pathological transformation.
In a healthy child, myelocytes, like other young forms, should not be detected in the blood. The release of myelocytes into the blood, as well as other maturing granulocytes, is determined by the same factors as in adults. Also, the detection of immature cells in babies is often diagnosed with congenital heart defects, uncontrollable vomiting and dehydration. Very often, immature forms of granulocytes are found in children with weak immunity.
Severe physical stress will also lead to the appearance of a small number of myelocytes in the blood of healthy children.
As for pregnant women, fluctuations in the blood picture are allowed. The process of hematopoiesis during pregnancy is enhanced to maintain the vital functions of the entire body of the mother and baby. Additionally, the appearance of myelocytes and other young forms in the blood may be the result of an exacerbation of chronic diseases, for example, sinusitis, pyelonephritis, etc.
In expectant mothers, the concentration of myelocytes in the blood is allowed to be no more than 2-3%. But, in any case, this phenomenon requires further diagnosis in order not to miss the development of malignant pathology.
How to determine myelocyte level

A myelogram will show the exact level of myelocytes
Determination of the level of myelocytes, as well as other components of the bone marrow, is carried out by taking a bone marrow puncture. The resulting myelogram will show the exact cellular composition of the bone marrow.
Bone marrow samples are taken from:
- sternum,
- iliac crest,
- from the calcaneus (this is how puncture is performed in small children).
After receiving the punctate, the myelogram data must be compared with the data of the general clinical blood test.
How is the research conducted?
To test PD-L1 expression, you need a tissue sample that contains at least 100 tumor cells. It can be obtained during surgery or a biopsy. The material is examined by immunohistochemical method using special monoclonal antibodies. Depending on the level of PD-L1 expression, one of three results can be obtained:
- Negative - PD-L1<1%.
- Positive - PD-L1>1%.
- Highly positive - PD-L1>50%.
In modern oncology, a personalized approach to the selection of antitumor therapy is extremely important. This gives confidence that the patient has received the optimal treatment. Euroonco doctors follow this principle and use the most modern technologies. Cooperation with leading foreign oncology centers and specialized laboratories helps us with this. Contact us, we know how to help:
Book a consultation 24 hours a day
+7+7+78
Treatment

Elimination of the cause leads to normalization of the blood picture
Since myelocythemia is caused by the development of a disease, it is the root cause that requires treatment.
Only after the cause of the pathological change in blood composition has been clarified, treatment is prescribed.
There are many reasons for the penetration of immature blood cells, in particular myelocytes. The vast majority of such triggers, unfortunately, are dangerous diseases that can quickly claim a human life. At the slightest transformation in the composition of the blood, it is necessary to urgently consult a doctor, diagnose and prescribe the necessary treatment methods.