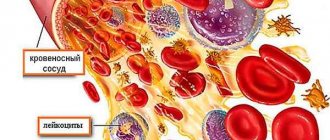
Large blood cells from the group of leukocytes are called monocytes. They protect the body from pathogenic microorganisms.
They are called agranulocytic because they do not have granules in the cytoplasm. In addition, they belong to active phagocytes, as they absorb foreign microorganisms and dissolve them.
In addition to destroying viruses, bacteria and fungi, monocytes absorb blood clots, preventing blood clots, and they also have an antitumor effect and accelerate regeneration processes. A decrease in monocytes may indicate the development of anemia, and an increase in their level may indicate infectious diseases.
In the section you will learn everything about monocytes in the blood and about the analysis for them (mon), transcript.
Basic information about monocytes
Monocytes are active white large cells; they live not only in the blood, but also in tissues and organs (liver, bone marrow, spleen, etc.).
Monocytes are formed in the bone marrow, and after 2–3 days they penetrate into the blood. Immature cells actively absorb foreign agents. Monocytes live in the blood for several days, and then move into the surrounding tissues, where they transform into histiocytes. The intensity of production depends on the concentration of glucocorticoids in the blood.
Monocytes perform the following functions:
- Eliminate pathogenic and foreign agents. White blood cells absorb microorganisms completely or their fragments. Unlike neutrophils, monocytes absorb large objects and in large quantities.
- Provide a surface for T-lymphocytes (helpers that enhance the immune response to foreign agents).
- They produce cytokines - information molecules through which leukocytes and other blood cells interact.
- Eliminate dead and destroyed cells, bacteria, and immune complexes from the body.
- Promote tissue restoration due to damage, inflammation or tumor damage.
- They have a cytotoxic effect on cancer cells, protozoa and plasmodia (the causative agent of malaria).
They are able to absorb pathogens even in highly acidic environments. Monocytes, together with leukocytes, provide complete protection of the body from viruses and bacteria.
What are monocytes in the human body and what are they responsible for?
Monocytes enter the peripheral blood and remain in it for 40–72 hours. They then migrate to organs and tissues for further maturation, where they are transformed into tissue macrophages.
To understand in what cases an increase or decrease in monocytes is observed, and whether this is a pathology, you need to understand what monocytes are and what function they perform.
A combination of monocytes and macrophages with reticular and endothelial cells form the reticuloendothelial system. This system carries out barrier, phagocytic and metabolic functions.
Depending on where macrophages are located, they acquire certain properties. The following types of such cells are distinguished:
- Kupffer's, formed as a result of the migration of macrophages to the liver;
- littoral, located in the lymph nodes and spleen;
- bone marrow;
- microglial, lining nervous tissue;
- peritoneal, located in pathological exudate (fluid entering the tissue when the permeability of the vascular wall increases);
- alveolar, located in lung tissue;
- osteoclasts, located in the bones;
- histiocytes are connective tissue cells.
First of all, you need to understand what monocytes are responsible for and what their content in the blood depends on. The main function of these cells is protective. They participate in the process of phagocytosis (intracellular digestion). First, the phagocyte purposefully moves towards the virus, bacteria or damaged cell.
Blood cells - monocytes
Then adhesion (sticking) of the foreign agent occurs on the surface of the macrophage. This is accomplished due to special receptors located on the phagocyte or through nonspecific adsorption (absorption). After this, special lysosomal enzymes are activated, which neutralize or destroy the pathogenic microorganism located inside the macrophage.
Monocytes take part in the formation of the immune response. Macrophages recognize a foreign antigen that has entered the body and absorb it. This antigen is then cleaved by lysosomes located in the cytoplasm of monocytes. Fragments of the split antigen form a special complex that releases special substances (interleukins). As a result, T and B lymphocytes are activated and antibodies specific to these antigens are formed.
Answering the question of what monocytes are in a blood test, it should be said that they are the only cells that produce tissue thromboplastin. This is one of the blood clotting factors that helps stop bleeding.
An equally important function of macrophages is their ability to secrete active substances: prostaglandins, pyrogens, lysozyme, properdin, interferon. Thus, they participate in antibacterial and antiviral defense, regulate cellular and humoral immunity.
Norm of monocytes in adults and children
A blood test can help determine your monocyte level. Concentration is calculated in absolute value per 1 liter of blood. Since monocytes are representatives of the group of leukocytes, their percentage is then determined in relation to all leukocyte cells.
The norm of monocytes for men and women is the same and does not change with age. The blood of an adult healthy person contains approximately 0.07 × 109/l. This value ranges from 0 to 0.08×109/l.
After determining the proportion of monocytes in the total number of leukocytes, this value is as follows: from 3 to 11%. In medical test results, the monocyte level is recorded as “Mon#” or “Mon: count/l”.
In a newborn, the concentration of mon in the blood is higher than in an adult. This is explained by the need of the immature child’s body for protection from pathogenic microorganisms.
Normal mon level as a percentage in children of different ages:
- From 0 to 14 days – from 3 to 12%;
- 15 days – from 5 to 15%;
- Up to 12 months – from 4 to 10%;
- From 12 months to 2 years – from 3 to 10%;
- From 2 to 16 years – from 3 to 9%.
Monocyte concentration in absolute units (monocytes x 109/l) for boys and girls of different ages:
- 15 days – from 0.19 to 2.4;
- Up to 12 months – from 0.18 to 1.85;
- From 1 to 3 years – from 0.15 to 1.75;
- From 3 to 7 years – from 0.12 to 1.5;
- From 8 to 10 years – from 0.10 to 1.25;
- From 11 to 16 years – from 0.09 to 1.15.
In adolescents over 16 years of age, the monocyte rate is the same as in adults.
If this indicator is normal, it means that monocytes promptly absorb and remove dead cells, and there are no pathogens in the body.
Monocyte test
To determine the concentration of mon, a complete blood count (CBC) with a leukocyte formula is prescribed. Capillary or venous blood is used for research. Doctors recommend performing this test at every visit to the clinic or hospital.
Analysis is prescribed in the following cases:
- Diseases of viral or bacterial origin;
- Oncological formations;
- Autoimmune diseases (eg, lupus, rheumatoid arthritis);
- Diseases of the hematopoietic system (for example, leukemia);
- Anemia;
- Worm infestations;
- Inflammatory diseases of the digestive tract.
In order for the results of the study to be as reliable as possible, you need to properly prepare for it. The analysis is recommended to be carried out in the morning on an empty stomach, which means that the last meal should occur no later than 4 hours before the procedure.
It is prohibited to consume fatty and fried foods or alcoholic beverages the day before the test. Avoid stress and excessive physical activity before the test.
The role of monocytes in the diagnosis of diseases
Monocytes are important components of the leukocyte formula that allow the doctor to assess the state of a person’s health. If the concentration of blood cells is increased or decreased, this indicates a disorder within the body.
This indicator is especially important during gestation. This is explained by the fact that the immune system of a pregnant woman devotes all its strength to protecting the fetus from pathogens.
Monocytes are a kind of “janitors” of the body, as doctors call them.
And all because blood cells cleanse the blood of parasites and harmful microorganisms, absorb dead cells and have a beneficial effect on the circulatory system.
Sometimes the number of white cells in the body decreases or increases due to stress, excessive physical activity, or after taking certain medications. Therefore, before testing the blood for monocyte levels, the doctor asks questions that must be answered as honestly as possible.
Increased monocyte concentration
Monocytosis is a condition characterized by an increase in the number of monocytes. Monocytosis can be relative (the percentage of cells is above 11%, and the total content is within normal limits) or absolute (the total content of monocytes is above 0.70 × 109/l).
An increase in mon levels indicates an inflammatory process during the height of the disease:
- Infectious diseases of viral and bacterial origin (mumps, influenza, monocytic tonsillitis, tuberculosis);
- Mycoses (diseases of fungal origin);
- Inflammation of the small or large intestine;
- Peptic ulcer;
- Endocarditis of infectious origin (inflammation of the heart membrane);
- Rheumatism (inflammation of connective tissue);
- Sepsis (blood poisoning);
- Postoperative period (after removal of the appendix, surgery on the pelvic organs);
- Autoimmune diseases (lupus erythematosus, sarcoidosis);
- Malignant tumor;
- Diseases of the hematopoietic system (leukemia, polycythemia, benign thrombocytopenia).
Often the concentration of monocytes increases along with lymphocytes.
A slight increase in monocytes is observed during the period of recovery from various diseases.
Monocytes in a child’s blood increase in the following cases:
- Measles;
- Diphtheria;
- Rubella;
- Piggy.
You can find out more about elevated monocyte levels in a child here.
Mon levels are of particular importance after recent acute tonsillitis.
Mon blood test
When studying the results of studies of a general blood test, many paid attention to the column “monocytes” (mon%), but not many know why these same monocytes are in the blood, what function they perform and what indicator in the blood is considered normal.
What are monocytes?
Monocytes are white blood cells produced in the bone marrow. Monocytes belong to the group of leukocytes, only much larger. They are found in greatest concentration in the liver, spleen, lymph nodes and bone marrow.
What function do monocytes perform?
The main purpose of white blood cells is the destruction and disposal of foreign cells and microorganisms. In addition, monocytes prevent the formation of blood clots in blood vessels and prevent the development of cancer cells. Due to their large size, monocytes easily cope with many pathogenic cells that are not able to destroy leukocytes and neutrophils. Monocytes contribute to the restoration of tissues damaged during inflammatory and oncological diseases. White blood cells participate in the formation of the body's defense system, thereby protecting a person from viral and bacterial infections.
The norm of monocytes in the blood of women
For an adult healthy person, regardless of gender and age, the concentration of monocytes in the blood remains almost unchanged and varies from 2 to 11% of the total number of cells that make up the blood. In the form with the analysis result, the indicator looks like this: Mon#***x 109 / l. It is very important to know the concentration of monocytes in the blood; any deviation from the norm will allow timely diagnosis of the disease and initiation of drug treatment.
Why is the concentration of monocytes in the blood determined?
White blood cells are one of the most important components of the leukocyte formula, the main components of which give the doctor a general idea of the patient’s health status. Too high or, conversely, too low a MON index in the blood may indicate the development of some kind of internal disorder.
You may be interested in: Testing for torch infections during pregnancy
Indications for donating blood for monocytes
To determine the concentration of monocytes in the blood, it is enough to simply donate blood from a finger; this procedure does not require any special preparation. Based on the quantitative content of MON in the blood and the detailed leukocyte formula, the doctor will be able to confirm or deny the presence of a particular disease.
Blood testing for monocytes must be donated in the following cases:
- the presence of neoplasms, both benign and malignant;
- viral or bacterial infection;
- autoimmune diseases;
- leukemia;
- anemia;
- suspicion of infection with helminthic infestations.
In addition to the above situations, the doctor may prescribe a blood test for monocytes in other cases, based on the existing circumstances.
Why is the MON index in the blood elevated?
An increase in the level of monocytes in the blood is called monocytosis. Often, monocytosis develops due to the penetration of viral or fungal pathogens into the human body. In addition, an increase in the number of monocytes in the blood is observed:
- for infectious diseases of viral and bacterial origin (monocytic tonsillitis, mumps, influenza, tuberculosis);
- sepsis;
- rheumatism;
- during the rehabilitation period after removal of the appendix;
- surgical operations on the pelvic organs;
- venereal diseases;
- tuberculosis;
- malignant neoplasms.
Physiological reasons for increased MON in the blood
Along with diseases, an increase in the monocyte index in the blood can be triggered by a number of physiological reasons. A slight increase in the concentration of monocytes in the blood is observed in the first two hours after eating, which is why doctors recommend testing for this indicator on an empty stomach.
Reasons for increased monocytes in women
High monocyte counts in women are often due to hormonal changes during the menstrual cycle.
- Period
During menstruation, some girls experience a slight increase in the concentration of monocytes in the blood. This is due to the fact that the endometrium is actively being rejected, and white blood cells are actively multiplying to dispose of the rejected blood clots. The highest level of MON in the blood of women is observed on days 2-5 of the cycle, that is, on days of heavy bleeding. At the end of menstruation, the number of monocytes in the blood decreases.
- Unstable psycho-emotional state
Women are less resistant to stress and more often susceptible to nervous disorders than men. If an unfavorable emotional situation persists for a long time, the concentration of monocytes in a woman’s blood may increase slightly.
You may be interested in: Blood test for fibrinogen
Why is the MON in the blood low?
A greatly reduced monocyte index is extremely rare and does not always indicate the presence of any pathology. Often MON≤ 2 occurs in pregnant women and for some time after childbirth, this is due to changes in the hormonal levels of the expectant mother.
In addition to pregnancy, the following factors can affect a decrease in the concentration of monocytes in the blood:
- genetic predisposition to anemia;
- taking hormonal medications;
- long-term and difficult to treat infectious diseases;
- recovery period after organ transplantation;
- decreased immunity due to sudden weight loss;
- stress.
The most dangerous situation for human health is when monocytes are completely absent. The absence of white blood cells in the blood indicates severe leukemia, when the bone marrow does not produce these cells at all and the body’s resistance to external factors is zero.
No less dangerous to human health is a disease such as sepsis, in which there are so few monocytes that they cannot cope with their function of purifying the blood. As a result, they themselves die from the toxic effects of the infection.
Decreased monocyte levels
Monocytopenia is a condition in which the concentration of monocytes decreases.
The main reasons for a decrease in the number of white cells in the blood:
- Panmyelophthisis (applastic anemia) – anemia due to folic acid deficiency;
- Infectious processes in acute form, in which the number of neutrophils decreases;
- Long-term treatment with glucocorticoid drugs;
- Pancytopenia (decrease in all blood components in the bloodstream);
- Hairy cell leukemia (a rare form of leukemia);
- Radiation sickness.
The complete absence of monocytes in the blood indicates a severe form of leukemia or blood poisoning.
A decrease in mon levels is typical for a patient who is severely malnourished or in shock. This condition is observed in women after childbirth or in the postoperative period. Monocytopenia is often caused by parasites.
Decrease level
A decrease in the level of monocytes below 1% indicates that there is a failure in the immune system or in the processes of hematopoiesis. This condition is called monocytopenia. It creates favorable conditions for the development of purulent inflammation, infection, and sepsis.
The main causes of monocytopenia are blood diseases: aplastic anemia, severe forms of leukemia. This often also happens when the immune system is suppressed due to radiation or chemotherapy, HIV infection, or taking glucocorticosteroids. But there are factors that can also lead to a decrease in monocyte levels:
- purulent pathologies – phlegmon, abscess, osteomyelitis;
- unbalanced diet, lack of B vitamins;
- multiple organ failure;
- poisoning;
- severe stress, shock;
- surgery, childbirth.
Note! A decrease in monocytes is often observed during pregnancy. This occurs due to decreased immunity, lack of vitamins, and anemia.
Monocyte levels are assessed with every blood test. This makes it possible to identify some serious pathologies at an early stage. If deviations from the normal amount are detected, their level can be normalized only by eliminating the cause. Therefore, the analysis should be deciphered by a specialist who will take into account all other indicators.