- home
- Gynecology
- Incompetent scar on the uterus
Laparoscopic treatment of incompetent uterine scar
Currently, the number of cesarean sections is steadily increasing, which in turn increases the percentage of postoperative complications. One of these complications is the formation of an incompetent scar on the uterus . Most often, when signs of failure of the uterine scar after a cesarean section are detected, the patient is advised not to plan subsequent pregnancies in order to avoid a number of serious obstetric complications.
In a situation where the uterine scar is not fully formed, laparoscopic reconstructive metroplasty (excision of pathological tissue in the scar area with the formation of a new full-fledged suture) can be considered the only effective method of solving the problem, which allows restoring the reproductive potential in this group of patients.
Among the risk factors for the formation of an incompetent scar on the uterus, the development of postpartum endometritis (85%) and cesarean section for emergency indications (15%) play the greatest role.
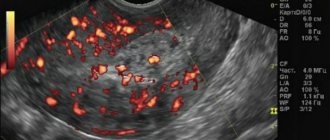
Diagnosis of an incompetent scar on the uterus is carried out using transvaginal ultrasound examination of the pelvic organs, hydrosonography and hysteroscopy. In the majority of patients (70%), the presence of a niche is determined in the scar area; in 30%, the thickness of the myometrium ranges from 1.5 to 2.5 mm. Also, endometrioid infiltrate can be detected in the scar area, which requires surgical removal.
To determine the depth of the lesion and the length of the incompetent scar, as well as to select the correct surgical treatment tactics, you must send me a complete description of the pelvic ultrasound, if possible, an MRI of the pelvis and hysteroscopy data, indicate your age and main complaints by email. Then I will be able to give a more accurate answer to your situation.
Treatment of an incompetent uterine scar
“Hand suture in endoscopic surgery”, K. V. Puchkov, D. S. Rodichenko
Patent. Method of laparoscopic myomectomy
To correct a defective scar on the uterus, women are offered open (laparotomy) surgery. This is due to the location of the altered scar in an “inconvenient” area for the surgeon under the bladder. Excision of the scar in this area is accompanied by severe bleeding due to the good blood supply to this area of the uterus. This complication often leads to blood transfusion during surgery.
For this reason, laparoscopic correction of a pathologically altered scar often involves greater blood loss than open surgery, lasts longer, and is associated with a fairly high risk of conversion—switching to open surgery. In such difficult conditions, during laparoscopy, the surgeon creates a less reliable suture on the wall of the uterus than during open surgery.
I was actively looking for ways to resolve this issue. As a result of 10 years of work, I developed an original method of laparoscopic surgery to correct incompetent uterine scars (metroplasty) , which, in our opinion, allows us to successfully solve all the problems described above. In this case, the operation to excise pathological tissues in the scar zone with the formation of a new full-fledged suture is performed laparoscopically without blood loss, with reliable suturing of the uterine wall, as well as the absence of adhesions in the pelvic area, which is very important for preserving the patient’s ability to conceive independently, the course of pregnancy and subsequent births.
The advantages of laparoscopic reconstructive metroplasty are obvious:
- reducing the invasiveness of the operation - instead of an incision in the anterior abdominal wall - 3 punctures of 5-10 mm;
- cosmetic effect;
- reducing the risk of adhesions;
- fast rehabilitation.
TREATMENT
PPP is a potentially life-threatening condition. Its treatment requires the efforts of a coordinated multidisciplinary team. Complications include: massive bleeding, genitourinary trauma, amniotic fluid embolism, consumption coagulopathy, blood transfusion complications, acute respiratory distress syndrome, postoperative thromboembolism, sepsis and multiple organ failure. Delivery is performed surgically. However, the optimal surgical approach has not yet been established. It is generally recommended to avoid attempting to separate the placenta as this can cause massive bleeding. The severity of this condition underscores the importance of accurate prenatal diagnosis, as it has a profound impact on patient management and outcomes.
The essence of the method is as follows:
At the first stage, I perform laparoscopy and, after isolating the uterine vessels, use soft vascular atraumatic clamps to temporarily block the blood flow in them (RF Patent for invention No. 2407467).
After opening the vesicouterine fold of the peritoneum and lowering the urinary tract, I excise the pathologically altered scar tissue using a monopolar “needle” electrode. To do this, I use a device for dosed electrothermal tissue ligation “LigaSure” (USA). I perform this stage under hysteroscopy control. The surgical field in such conditions is absolutely “dry”; I can clearly see the border between the pathological scar and healthy tissue, as well as all the layers of the uterine wall.
Video from the operating room: Correction of an incompetent scar on the uterus
If it is necessary to remove an endometrioid lesion from the uterine wall, then I use modern ultrasonic scissors, which minimally injures the surrounding healthy tissue of the uterine wall and improves the healing processes in the intervention area.
Next, I perform suturing of the uterine wall with a synthetic absorbable thread “V-lock 180” 0 (Covidien, Switzerland) or “Monocril” 0 in two rows with its peritonization, comparing all muscle layers layer by layer. Good visualization of the surgical field allows this to be done easily and reliably.
The next step is to use modern anti-adhesive barriers, which several times reduce the risk of adhesions in the pelvic area, preserving fertility and the possibility of subsequent births.
At the final stage, I remove the soft clamps from the arteries and completely restore blood flow in the uterus.
The advantages of the new “bloodless” reconstructive metroplasty technique are as follows:
- The operation is performed without blood loss, which allows the pathological scar to be isolated and excised with minimal trauma to surrounding tissue.
- The method allows for reliable suturing of the uterine wound, which is necessary for subsequent pregnancy and childbirth.
The technique is especially indicated for patients:
- Those planning pregnancy;
- With the presence of a niche in the scar zone and the thickness of the myometrium from 1.5 to 2.5 mm;
- With the presence of endometrioid infiltrate in the scar area;
- With concomitant uterine fibroids.
Watch a video of operations performed by Professor K.V. Puchkov. You can visit the website “Video of operations of the best surgeons in the world.”
After laparoscopy, three incisions 5-10 mm long are left on the skin of the abdomen. From the first day, patients begin to get out of bed and eat. Discharge from the hospital occurs on the 2-3rd day.
After surgery, we usually prescribe hormonal therapy for 3-6 months to optimize regenerative processes in the uterus. Dynamic observation by a gynecologist is necessary - examination, ultrasound after 1, 3 and 6 months. Pregnancy after laparoscopic reconstructive metroplasty is possible after 6-8 months. It is advisable to first perform hysterosalpingography - an x-ray assessment of the patency of the fallopian tubes and the condition of the uterine cavity. Depending on the size of the suture on the uterus, childbirth is possible either through the natural birth canal or by caesarean section.
Upon completion of the operation, I make sure to use modern anti-adhesive barriers to reduce the risk of adhesions in the pelvic area.
I have experience of about 3,700 minimally invasive surgical interventions on the uterus, including the correction of incompetent scar on the uterus after cesarean section, the results of which are summarized in the monograph “Laparoscopic operations in gynecology”, as well as in more than 50 scientific publications in various professional peer-reviewed scientific publications in Russia and abroad.
Every year, my team of medical specialists and I conduct up to 40 master classes and seminars on modern aspects of high-tech laparoscopic surgery in Russia, the CIS countries and Western Europe. My seminars on laparoscopic treatment of diseases of the uterus and other diseases are attended by medical specialists from large scientific centers, republican, regional and regional hospitals, and students of postgraduate education faculties.
RISK FACTORS
A history of cesarean section and placenta previa are the two most important predisposing factors for the development of PPP. The risk of placenta accreta in the presence of placenta previa in a patient with three previous cesarean sections is up to 40%, compared with less than 1% in the absence of placenta previa. Therefore, the presence of placenta previa in a patient with a cesarean scar serves as a “red flag” for possible placenta accreta. Other risk factors include advanced maternal age, multiple pregnancies, previous uterine surgery, endometrial ablation, Asherman's syndrome, uterine leiomyomas, uterine anomalies, hypertension during pregnancy, and smoking.
The exact pathogenetic basis of PPP remains a mystery. This condition is thought to be associated with pathological decidualization and excessive trophoblastic proliferation at the scar site.
Questions asked by patients with an incompetent uterine scar
Why does an incompetent uterine scar occur?
Most often, failure of the uterine scar occurs after a cesarean section. Among the risk factors for scar formation, the greatest role is played by the development of postpartum endometritis (85%) and the performance of cesarean section for emergency reasons (15%).
How should I prepare for surgery to treat a failing scar?
In general, surgery using my method requires preliminary preparation, like any laparoscopic operation. And this operation has its own characteristics. If you are planning surgical treatment using the method of excision of pathological tissue in the scar area with the formation of a new full-fledged suture, please carefully study the preparation for surgery section. An obligatory component of my surgical technique is the prevention of thrombosis and thromboembolism.
If, in addition to an incompetent scar, I have other diseases, can they be cured during one operation?
The answer to this question is: yes, but the terms need to be clarified. Several operations can be performed, sometimes by three or four or even five surgeons, but there will be only one general anesthesia, and you will be hospitalized in the clinic only once. These types of operations performed simultaneously are called simultaneous.
In many patients, an incompetent uterine scar is combined with other gynecological (fibroids, endometriosis, etc.) and non-gynecological diseases requiring surgical treatment. For example, nodular changes in the thyroid gland, hiatal hernia, nodes in the mammary glands, hernia, hemorrhoids, varicose veins of the legs and a number of others. The minimally invasive surgery techniques I use make it possible to perform two and sometimes three operations simultaneously during one anesthesia by a team of several surgeons.
The issue of simultaneous operations for incompetent sutures on the uterus and other conditions is discussed in detail in a special section of the site.
What anesthesia is used during laparoscopy on the uterus?
The operation is performed only under general combined anesthesia. We use additional preparation (premedication) carried out in the ward to eliminate any form of psychological stress in patients awaiting surgery. If you would like to learn in more detail about the methods of pain relief used during uterine surgery, please read carefully the information specifically posted on the website.
What awaits me after the operation?
Laparoscopic reconstructive metroplasty, performed according to the original method of our clinic, is usually easily tolerated by patients, since trauma to the anterior abdominal wall and blood loss are minimal. The patient remains in the hospital for up to 3 days after the operation, receives antibacterial, anti-inflammatory treatment and drugs that contract the uterus.
Bloody discharge from the genital tract can continue for 7-10 days; as a rule, it is more abundant for 1-2 days, then scanty. The temperature can rise within 5-7 days, on the first day - up to 38 C, then up to 37.3 - 37.5 C. The staff monitors body temperature and the amount of discharge from the genital tract. Upon discharge, patients are given detailed recommendations on how to behave at home and how to take medications. The entire period of postoperative rehabilitation is monitored by the operating doctors by telephone and during repeated consultations, with the involvement of an ultrasound diagnostic specialist to monitor the condition of the uterine scar.
You can take a shower after the stitches are removed (5-7 days after surgery), until this point it is recommended not to wet the stickers.
The next day after the operation, we allow the intake of broth, kefir, and yoghurt; on the 2nd day you can add soup, steamed chicken cutlet, cottage cheese; After the appearance of stool, it is recommended to gradually expand the diet to the usual.
Patients are advised to abstain from sexual activity for one month after surgery.
When should I have an ultrasound performed after laparoscopic reconstructive metroplasty?
An ultrasound examination is performed on the 5-7th day after surgery. Subsequent studies are prescribed by the operating surgeon individually, approximately 1, 3 and 6 months after surgery. If pregnancy occurs, it is imperative to strictly monitor the condition of the uterine scar.
How long after surgery can I return to physical activity and sports?
Three weeks after surgery, patients are allowed to visit the pool, and after 1.5-2 months - return to normal physical activity.
Do I need to take medications after metroplasty surgery?
Yes, in order to improve reparative processes in the area of the postoperative scar on the uterus, normalize hormonal status and prevent exacerbation of inflammatory processes in the pelvic area, as a rule, patients are prescribed oral contraceptives for 4 - 6 months.
How long after laparoscopic metroplasty can I plan a pregnancy?
Pregnancy is permitted 6-8 months after surgery, upon receipt of convincing ultrasound data about the maturation of the uterine scar. You can be observed in the clinic until conception and subsequent pregnancy management for up to 12 weeks. Next, we recommend a medical facility and a doctor who has experience in caring for pregnant patients and delivering births with a uterine scar.
Where do you perform metroplasty operations?
I constantly operate a lot (up to 1100-1200 operations per year), conduct demonstration operations and master classes in several clinics in Russia, the CIS countries and Western Europe. I conduct the initial consultation in Moscow at the Swiss University Clinic. Learn in more detail about the main clinical sites in Moscow and Switzerland.
— Is it possible to communicate with your patients who have already undergone surgery if I have not yet made a decision?
This site has collected about 2,500 reviews from patients who have undergone surgery over the past 5-7 years. You can read the reviews of my patients, written both after discharge from the hospital and several months or years later, on the next page of the site - reviews of patients after operations on the uterus. On this page you can find the email addresses of those patients who agreed to respond to letters from other women interested in having surgery with me. You can use these contact details.
How is an ultrasound of the uterus done after a cesarean section and when?
An ultrasound of the uterus after cesarean section is done before discharge from the hospital, and then repeated a week later. To control the size of the body and the uterine cavity, the transabdominal method is used - the emitter of the device is placed on the anterior wall of the abdomen. If you need to assess the condition of the uterus or part of the suture, then the use of the vaginal examination method is also allowed.
The size of the uterus is normal
In order to assess the contractility of the uterus, its size and other parameters are examined over time (see table).
| Parameter | By the end of 4 days | To the end of the week | By day 10 |
| Body of the uterus length, cm | 13,5-14,5 | 11,5-12,5 | 9,4-11 |
| Body of the uterus width, cm | 13,4-13,8 | 11,1-11,9 | 9,6-10,6 |
| External anterior-posterior size, cm | 6,7-7,1 | 6,4-6,9 | 6,1-6,8 |
| Uterine cavity length, cm | 11,8-12,3 | 8,8-9,4 | 7-7,8 |
| Uterine cavity width, cm | 10,5-11,7 | 8-8,5 | 6,9-5,8 |
| Internal anterior-posterior size, cm | 5-7 | 3,8-4,5 | 2,8-3,7 |
| Form | Oval | Pear-shaped | Pear-shaped |
| Fundal height of the uterus | 4 cm below the navel | Midway between the navel and pubic bone | 2 cm above the pubis |
| Uterus weight, kg | 0,9-1 | 0,5-0,6 | 0,4-0,5 |
Complete return of the uterus to its previous state can be expected by 6-8 weeks after surgery.
If the cavity is expanded
If an ultrasound reveals an expansion of the uterine cavity, this is a sign of insufficient contraction. This condition is called uterine subinvolution and is often discovered after a cesarean section. The doctor may recommend the introduction of contraction drugs (for example, Oxytocin), since slow recovery is one of the causes of inflammation and bleeding.
If necessary, the doctor may prescribe hysteroscopy (examination of the uterine cavity with an endoscope) to identify the cause: blood clots, retention of parts of the placenta, remnants of the amniotic sac, endometritis, fibroids. If there is a lot of blood in the uterine cavity, then curettage may be necessary to accelerate contractility and prevent infectious and inflammatory complications.
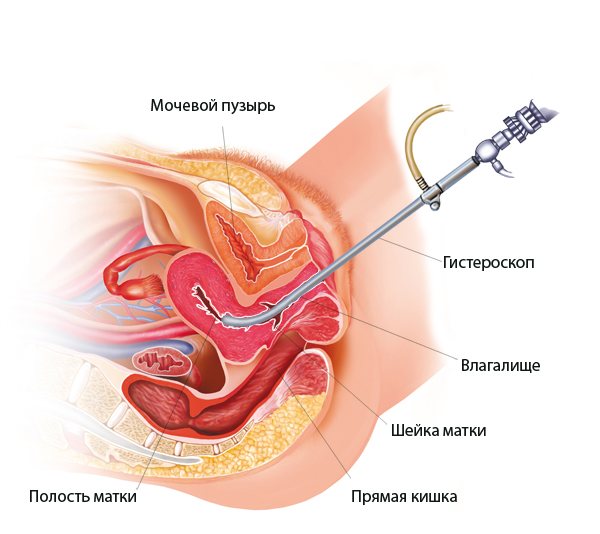
Hysteroscopy
Other possible deviations
Ultrasound can also reveal the causes of other deviations in the recovery period:
- bleeding – blood clots, polyp, suture dehiscence, bleeding placental site;
- increased body temperature and increased pain, discharge - endometritis (inflammation) due to infection, delayed contraction of the uterine cavity.
The earlier the diagnosis is made, the shorter the course of treatment will be, and if the ultrasound is not completed on time, then there is a risk of complications:
- endometriosis (endometrial particles grow into the cervix, bladder, ovary, fallopian tubes, intestines), which leads to severe pain and bleeding, infertility;
- blood poisoning (sepsis);
- inflammation of the peritoneum (peritonitis);
- inflammation of the uterine veins with blockage;
- heavy uterine bleeding.