Liver disease is one of the most common diseases of the digestive system, the steady increase of which is called “the second epidemic of our century.” A special place among them is occupied by various tumors and tumor-like lesions. In recent years, thanks to the introduction into clinical practice of more advanced diagnostic equipment and the fairly widespread use of various contrast agents in studies of the abdominal cavity using ultrasound, X-ray computed tomography and magnetic resonance imaging, the possibilities for correct diagnosis of various focal liver lesions have significantly increased. In addition, the sensitivity and specificity of various methods for diagnosing liver tumors reaches 88-97%.
According to many authors, benign tumors do not have clinical symptoms and manifest themselves mainly in the form of focal liver formations. In clinical practice, as focal liver formations are identified, the question of topical diagnosis and exclusion of malignancy of the process becomes acute.
Hemangioma
Hemangiomas are considered by many authors to be the most common benign vascular tumors of the liver of mesenchymal origin, occurring in various age groups. Capillary hemangioma consists of a plexus of a large number of branching capillary-type vessels with a narrow lumen and without directional or very slow blood flow; 90% of the area of the vascular bed is venous caverns. Cavernous hemangiomas are more common than capillary hemangiomas, and in some cases there is a mixed type. According to most authors, hemangiomas usually do not manifest clinically and are relatively more often detected in women.
On ultrasound, small (up to 3.0 cm) hemangiomas appear as homogeneous hyperechoic formations with clear contours. In some cases, the echogenicity of hemangiomas may be reduced, and the contours may appear blurred. In some hemangiomas, a pseudocapsule in the form of a hypoechoic rim can be clearly visualized, which makes their differential diagnosis with metastases difficult. Many researchers associate the prospect of improving diagnostics with the use of intravenous contrast with special echo contrast agents.
Capillary hemangioma of the liver is a homogeneous hyperechoic focus less than 3 cm with clear boundaries.
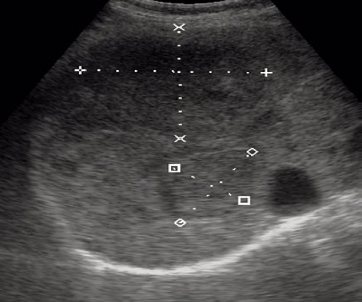
Two cavernous hemangiomas of the liver.
What does this represent?
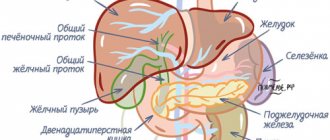
The correct anatomical structure of the gland implies the division of the organ into right and left lobes. In addition, the right one is further divided into two parts. The body of the liver consists of 8 segments, which have a separate blood supply, innervation and outflow of bile. The liver parenchyma in its normal anatomical form is granular. The degree of severity of this so-called granularity is the main criterion for determining the condition of the gland. Any changes in the structure of the liver are considered pathological abnormalities.
Normally, blood vessels and bile ducts do not show increased echogenicity during ultrasound examination.
Focal nodular hyperplasia (FNH)
Focal nodular hyperplasia (FNH) is considered the second most common benign liver tumor (after hemangiomas). According to a number of authors, FH occurs in 0.9-5% of the population, and in 5-20% of cases it can be combined with cysts and hemangiomas. According to the literature, FUH, without having any signs of a tumor, is included in the group of benign hepatocellular tumors of epithelial nature. This is a single, round, non-encapsulated formation with impaired hepatic architecture, separated by septa reaching the central scar. The average size of the lesion is 5.7 cm (from 1.5 to 12.0 cm). It has been established that FUH is not prone to hemorrhage and has no malignant potential. Usually the tumor is an incidental finding during diagnostic studies. Small nodules are usually asymptomatic. Large tumors can cause abdominal pain.
With native ultrasound, in most cases, FUGs are difficult to visualize, appearing as a rounded area with clear contours, an isoechoic or slightly hypo- or hyperechoic structure. According to some authors, in diagnosing FEG, contrast ultrasound is more informative in contrast to other diagnostic methods. The emergence of second-generation echo contrast agents has significantly expanded the capabilities of the method. This makes it possible to differentiate different types of tumors, taking into account their nature of vascularization, which is important in the differential diagnosis of focal liver formations. Increased vascularization of the tumor in combination with the characteristic “wheel with spokes” pattern is a pathognomonic sign of FAG (71.4%). In this case, the detection rate of the “feeding” artery of the tumor increases to 98%. The sensitivity and specificity of ultrasound using intravenous contrast in diagnosing FUG reaches 83 and 98%, respectively.

Hypoechoic formation in the liver is benign focal nodular hyperplasia. The literature describes that it is characterized by a central scar (white arrow).
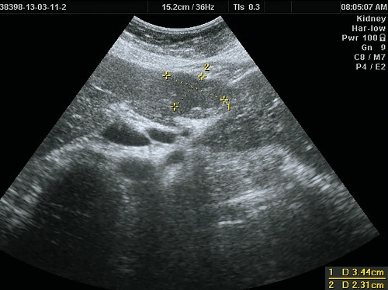
B-mode. In the IV segment of the liver, reaching the contour of the liver, deforming it, a tissue density hypoechoic formation, somewhat heterogeneous in echostructure, measuring 50 x 40 mm, irregular in shape, with clear, even contours, is visualized.
Introduction
According to the definition of pathologists, focal nodular hyperplasia of the liver is a benign formation related to hamartomas, which is manifested by focal hyperplasia of liver cells forming parenchymal nodules surrounded by fibrous layers [1]. According to the International Classification of Diseases (ICD-10), this disease is included in the heading “Other specified liver diseases”, K 76.8. In the international histogenetic classification of tumors of the liver and intrahepatic bile ducts, it appears as “focal nodular hyperplasia.” In the literature there are synonyms for the name of this disease: “fibronodular hyperplasia” and “focal cirrhosis of the liver.” In our opinion, the terms “focal nodular hyperplasia” and “focal cirrhosis” are not entirely appropriate. The phrase “focal nodular” is essentially a tautology, since it practically means the same thing (from the Latin focus - hearth, nodulus - node). The term “focal cirrhosis” accurately reflects the morphological essence of the disease, but in the minds of most clinicians, cirrhosis is strongly associated with diffuse liver damage. From our point of view, it is “fibronodular hyperplasia” (FNH) that is a completely acceptable term from a semantic point of view, since it most clearly corresponds to the morphological substrate of the disease - a node of hepatocyte hyperplasia with fibrosis.
Until relatively recently, FNH was classified as a rare (3%) space-occupying liver lesion (LLI) [2, 5, 6]. Currently, due to the active use of modern liver imaging methods, the number of identified patients with FNH (as well as focal liver diseases in general) has increased [3, 12]. According to the literature, FNH in the structure of focal liver diseases ranks third among benign AKIs after hemangioma and adenoma [4, 8]. The etiology and pathogenesis of FNH remain unclear [11]. The theory about the participation of hormonal contraceptives in the development of FNH has not been confirmed, and currently most researchers believe that FNH is the result of the progression of congenital or acquired vascular malformations, leading to hepatocyte hyperplasia [8, 9, 14]. Macroscopically, FNH is most often defined as a well-demarcated soft-elastic formation from the liver tissue, sometimes dense, yellow, cherry, whitish, light brown or pinkish in color, a lobulated structure with the presence of fibrous layers, usually extending from a centrally located scar.
FNH is a formation that is visually and palpably often indistinguishable from a malignant tumor. The macroscopic picture is determined by the ratio of parenchymal, fibrous and vascular components, which can be different, therefore, with full confidence, the diagnosis of FNH can only be established after a histological examination of the entire removed specimen. FNH can be observed in the form of one or multiple foci.
The microscopic picture is similar to that of true large-nodular cirrhosis of the liver. There is hyperplasia of the liver parenchyma, divided into nodes by fibrous layers; the latter form star-shaped scars. Hepatocytes contain excess amounts of glycogen and fat. In the fibrous layers there are small bile ducts, sometimes inflammatory infiltration is detected. Abnormal vessels with thickened walls are observed. The process is focal in nature, the liver tissue outside the focus appears unchanged [8, 11].
The disease is often asymptomatic and is an incidental finding during an ultrasound of the liver performed for another reason. Clinical manifestations (discomfort, feeling of heaviness) are caused by the “mass effect” and differ little from those with other AKI. There are no specific laboratory symptoms. FNH does not become malignant and extremely rarely causes complications such as intra-abdominal bleeding [13]. Cases of tumor regression up to its complete disappearance have been described [10]. When the diagnosis of FNH is confirmed and there are no complications, a number of authors recommend dynamic observation, although such tactics are debatable [7, 9, 10]. Therapeutic tactics for FNH remain controversial and, in addition, in the available literature we have not found any reports of attempts to trace the “natural” course of the disease when surgery is refused. This prompted us to share our own experience in treating this disease.
The purpose of the study was to retrospectively analyze the frequency of FNH among AKI and the treatment and diagnostic tactics for FNH over two time periods: from 1996 to 2005 and from 2006 to the present.
Material and methods
Over the past 17 years, 1425 patients with AKI have been treated in the hospital. 53 patients with FNH were observed, which accounted for 3.6% of all patients with AKI and 11.06% of patients with benign tumors. The age of patients with FNH ranged from 12 to 77 years, women predominated - 44 (83.2%). 47% of patients presented with complaints characteristic of AKI at an early stage of development - a feeling of heaviness, abdominal discomfort, which were based on stretching of the Glissonian capsule of the liver by a growing tumor; in other cases, the formation was accidentally discovered during ultrasound, less often during CT (“incidentaloma”). The final diagnosis of FNH was the result of the application of a comprehensive diagnostic algorithm for the management of patients with AKI of a solid structure [6], including ultrasound as a method of primary detection and monitoring, SCT and MRI as methods of clarifying diagnosis, and, if indicated, laparoscopy, biopsy, angiography, and laparotomy as the final stage of diagnosis. In our observations, tumor nodes were more often single, and only one patient had two lesions in both lobes of the liver. The diameter of the formations in the greatest dimension varied from 3.5 to 20 cm. 40 of 53 patients with FNH were operated on. The extent of the operation was determined by the size and location of the tumor. Extended left-sided hemihepatectomy was performed in 1 case, left-side - in 2, right-side - in 1, bisegmentectomy - in 8, atypical liver resection - in 16, tumor enucleation - in 8 cases. Exploratory laparotomy was performed in 3 patients, laparoscopic cholecystectomy for calculous cholecystitis with a biopsy of the detected tumor was performed in 1 patient. There were no deaths or complications directly related to liver surgery. Patient U.
, 18 years old, with congenital diabetes mellitus, on the 10th day after left hemihepatectomy, decompensation of diabetes was noted with the subsequent development of multiple organ failure syndrome. In another 24-year-old patient, latent porphyria manifested itself on the 8th day after right hemihepatectomy with the development of severe polyneuropathy. Death was avoided in both patients, but long-term intensive treatment was required in the intensive care unit. 12 patients were not operated on and are under observation with regular ultrasound. The follow-up period for patients with FNH ranged from 1 year to 13 years.
Results and discussion
A retrospective analysis of case histories since 1996 made it possible to identify two periods during which tactical approaches to the management of patients with FNH underwent some changes. The period from 1996 to 2005 was characterized by the predominant use of ultrasound as the main means of diagnosing focal liver disease, with FNH listed as a “rare” liver disease. The echosemiotics of FNH was poorly developed; there were no “conscious” diagnostic and treatment tactics. Under these conditions, the very fact of detection of AKI of unknown etiology determined the indications for surgical treatment, and the exact morphological diagnosis of FNH was established after surgery. During this period, 22 patients were operated on, and in 3 cases exploratory laparotomy was performed. Indications for surgical treatment were set out quite widely, but they refrained from removing the tumor if its benign nature was confirmed in the event of a large-scale intervention. This made it possible to trace the “natural” course of FNH. It turned out that the thesis about the “harmlessness” of the course of FNH is doubtful. This is confirmed by two of our observations published in the journal Surgery in 2005 [7].
As experience accumulated during the second period, from 2006 to 2013, it became apparent that FNH was more common than expected. In the diagnosis of FNH, the main place was occupied by SCT and MRI. Indications for dynamic monitoring of patients with FNH have become more frequent (with confidence in the absence of a malignant tumor). We have experience in observing the “natural” course of FNH, which did not require surgical treatment, in 12 patients. Moreover, in 11 cases, the diagnosis of FNH was established according to non-invasive diagnostic methods (ultrasound, SCT, MRI), in 1 - after laparoscopic cholecystectomy with tumor biopsy. The size of the formation in these patients was small (up to 5 cm in diameter), and there were no clinical symptoms. Monitoring with regular ultrasound over a period of 1 to 7 years revealed a slight increase in formation in only 3 patients, which so far excluded the need for surgery. In addition, analysis of the course of the disease in patients undergoing radical surgery in both periods made it possible to verify that after surgical treatment, during a control examination that included ultrasound, SCT, no signs of relapse of FNH were detected in any observation. In this regard, the main task of the second period (from 2006 to the present) is to determine clear indications for both surgical treatment and dynamic monitoring of people with FNH. An example of successful active treatment tactics is the following observation.
Patient L.
, 18 years old, ultrasound and MRI revealed a space-occupying formation with a diameter of up to 15 cm in the IV and V segments of the liver. There were no specific complaints, however, given the young age of the patient, the size of the formation, the impossibility of excluding its malignant nature, also the previous “negative” observation experience, we decided to operate.
On 08/12/10 the patient was operated on. Upon inspection in the IV (anterior sector) and V segments of the liver, there is a large tuberous formation with a diameter of 15 cm, protruding above the diaphragmatic and visceral surfaces, soft-elastic consistency, dark cherry color, with whitish veins, spreading to the bed of the gallbladder, most of the tumor is located in left lobe (Fig. 1)
.

Fibronodular hyperplasia of the IV, V segments of the liver. a — diaphragmatic surface of the liver; b — visceral surface of the liver. A left-side extended hemihepatectomy and cholecystectomy were performed. Histological conclusion: fibronodular hyperplasia of the liver (Fig. 2)
.
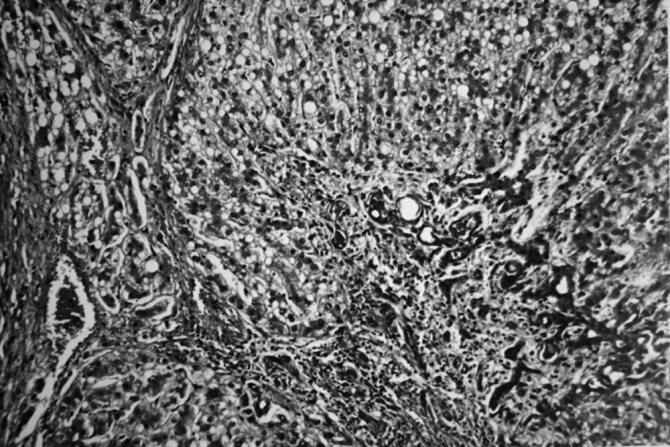
Fibrinodular hyperplasia. Hematoxylin and eosin staining. Uv. 100. The postoperative period was without complications. During a 3-year follow-up, there were no signs of disease recurrence. Full social adaptation. In the practice of hepatological surgeons, FNH is not so rare. It should be noted that surgeons of other specialties, as well as “visualization” doctors, are not well acquainted with this disease. At the stage of outpatient examination, the diagnosis of FNH was established only in 16 (30.7%) cases, which reflects both the lack of awareness of visualization doctors about this disease and the objective difficulties of diagnosis caused by the variability in the ratio of stromal, parenchymal and vascular components in the node . Most often, a formation in the liver at the preoperative stage was interpreted as a hemangioma, liver cancer, or “massive liver lesion of unknown origin.” It is not always possible to exclude the malignant nature of a pathological focus without surgery, therefore the advisability of laparotomy as the final stage of diagnosis in a number of cases is beyond doubt. The advisability of performing preoperative puncture biopsy under ultrasound or CT guidance in all patients seems controversial. It is often necessary to differentiate FNH from a malignant liver tumor, in particular hepatocellular cancer. A puncture biopsy of a lesion is not always informative (the biopsy sample is representative) and the finality of the histological conclusion in such situations is questionable. In addition, a biopsy for cancer is fraught with the risk of dissemination or implantation metastasis. We agree with the opinion of the authors who call not to perform a preoperative biopsy if cancer is suspected, since this factor worsens the prognosis of the disease [15]. If a hemangioma is suspected, such manipulation is in principle contraindicated due to the risk of intra-abdominal bleeding.
Based on our experience, we are currently cautious about long-term follow-up of patients, even with an established and histologically confirmed diagnosis of FNH. Mandatory conditions for this should be the possibility of regular ultrasound monitoring (once every 6-8 months) and sufficient compliance on the part of the patient. As with most AKI, “exit” of the lesion beyond the limits of easy operability is fraught with intraoperative problems and a severe course of the postoperative period [6].
Thus, FNH is a disease with unclear etiopathogenesis, uncontrolled course and a very uncertain individual prognosis. Tumor growth can lead to fatal complications. At present, the following tactics seem to be optimal for this disease: surgical intervention is indicated for “symptomatic” and rapidly growing FNH, the size of the lesion is over 5 cm, and it is impossible to exclude its malignant nature during a full examination. Dynamic observation is advisable if there is confidence in the diagnosis, small (less than 5 cm) size of the lesion, as well as well-known surgical risk factors (age, concomitant diseases), since the danger of the operation should not exceed the danger of the disease itself.
Comment from the editorial board
The widespread and availability of modern non-invasive diagnostic methods (CT, MRI), as well as an increase in their resolution, have led to an increase in the frequency of detection of asymptomatic focal liver tumors. The vast majority of them are benign, however, the doctor is often faced with the question of tactics for managing such patients. An article devoted to focal nodular hyperplasia, one of the most common benign liver tumors, will certainly be of interest to hepatologist surgeons, especially since Russian-language publications on this topic are rare.
First you need to decide on the terminology. At the beginning of the article, the authors suggest using the term “fibronodular hyperplasia.” You can agree with this or not, but in order to avoid confusion and misunderstanding, it is better to adhere to the international terminology proposed by the research group in 1995 (Terminology of Nodular Hepatocellular Lesions. International Working Party. Hepatology, 1995), in which this formation is defined as focal nodular hyperplasia and proposed criteria by which it can be distinguished from other regenerative formations.
Non-invasive methods play a dominant role in the diagnosis of FNH. MRI and CT have high sensitivity and specificity, however, in some patients the diagnosis may remain questionable, in which case a biopsy is justified, especially since “major” and “minor” criteria have been proposed for interpreting the material obtained from a biopsy (A. Fabre and al., 2002). The authors are wary of biopsy, fearing complications and implantation metastasis in the case of a malignant tumor, however, we believe that to establish a diagnosis it is necessary to use the entire arsenal of available means, and only if doubts remain, resort to laparotomy and resection of the formation. We consider the risks of a biopsy, if a number of rules are followed, to be exaggerated.
We adhere to a restrained tactics for managing FNH, since the prognosis is favorable: no cases of malignancy have been recorded, complications are rare (only a few cases of tumor rupture with bleeding have been described), most tumors are asymptomatic, and their sizes remain stable for long periods.
In this regard, we support the indications for surgical treatment given in the article: symptomatic tumor, its growth, the inability to exclude malignancy after a comprehensive examination. It is also important to note that the symptoms of FNH are nonspecific, so the exclusion of concomitant pathology of the abdominal organs, which may cause the clinical picture, is necessary. As for the recommendation to remove formations whose size exceeds 5 cm, one may disagree with this, since the presence of symptoms is influenced not only by the size of the formation, but also by its location and the proximity of surrounding organs. In addition, the size of the patient and his organs matters. For example, an FNH measuring 10 cm in a large person, located intraparenchymal, may not manifest itself in any way, and therefore the need for liver resection in him will be doubtful.
Thus, when choosing management tactics for a particular patient, one should focus on a set of factors, without exposing him to an unreasonable risk of surgical intervention, since mortality in the group of patients with benign liver tumors is unacceptable.
Hepatocellular adenoma (HCA)
Hepatocellular adenoma (HCA). HCA is considered a rare benign tumor originating from hepatocytes. There are suggestions about the influence of oral contraceptives, exogenous androgens, pregnancy and an imbalance of endogenous sex hormones on the development and growth of tumors. Conflicting data are provided on the size of adenomas - figures from 1 to 19 cm are indicated, with an average of 5.4 cm. In some cases, patients have multiple adenomas. The formations are well delineated. A number of authors note the characteristic distinctive features of adenomas - unlike hemangiomas, they are not located next to the hepatic vessels and do not occupy an entire lobe. The course of HCA is asymptomatic in most cases. When the tumor size is 5 cm or more or its subcapsular location, the risk of bleeding increases. The authors emphasize the practical importance of diagnosing adenoma due to the high risk of bleeding, rupture, malignancy and the need for surgical intervention.
On ultrasound, GCA usually looks like a solitary heterogeneous formation with clear contours of varying degrees of echogenicity: 20-40% of adenomas appear hypoechoic, 30% are hyperechoic, which is due to the presence of fatty inclusions in the tumor tissues. According to a number of authors, when using CDK, peripheral peri- and intratumoral vessels are identified in some cases.

Liver adenoma
Thus, ultrasound of the abdominal organs is currently a screening method for detecting tumors and tumor-like processes in the liver. Due to its fairly high information content and accessibility, ultrasound is performed at the first stage of diagnosis if a liver tumor is suspected. Ultrasound allows not only to detect a tumor in the liver, but also to judge its size, topography, and operability of the process. Intraoperative ultrasound is informative for the diagnosis of intrahepatic tumors, since other research methods are of little use during surgery.
Ultrasound in the “gray scale” mode allows you to identify various changes in the parenchyma. However, in some cases, it is not possible to make a differential diagnosis between diffuse diseases due to the similarity of echographic signs.
B-mode echography with Dopplerography of the vascular system of the liver with assessment of the hemodynamic state makes it possible to clarify the nature of the pathological process. However, despite the high specificity (97%), the sensitivity of the method in detecting liver tumors remains quite low (60%), which allows preference to be given to dynamic CT or MRI techniques. In addition, according to some researchers, the informativeness of the diagnostic conclusion of ultrasound, as a subjective research method, depends on the experience and qualifications of the ultrasound diagnostic doctor.
Bibliography
- S. V. Shakhidzhanova, T. S. Pustovitova, “Some aspects of the diagnosis of focal liver pathology,” journal “Clinical Imaging” N19, December 2001.
- A.Z. Guseinov, T.A. Guseinov, “Modern diagnosis of liver tumors”, Bulletin of new medical technologies, electronic journal – 2016 – N 4, Tula.
- Zh.N. Kyzhyrov, B.B. Baimakhanov, M.M. Sakhipov, A.T. Chormanov, N.N. Birzhanbekov, E. Serikul, “Diagnostics of focal liver diseases”, Bulletin No. 1, 2021, Kazan.
- S.N. Berdnikov, V.N. Sholokhov, Yu.I. Patyutko, M.S. Makhotina, E.S. Chuchuev, K.E. Abirov, “Complex elastography and elastometry in the differential diagnosis of hyperechoic liver formations,” Journal: SonoAce Ultrasound No. 25, Moscow.
- O.M. Kurzantseva, “Some aspects of the diagnosis of focal nodular hyperplasia of the liver (fibronodular hyperplasia)”, Journal: SonoAce Ultrasound No. 30, Kemerovo.