Increasing values:
- chronic hepatitis;
- bile stagnation;
- autoimmune inflammation of the liver;
- acute hepatitis caused by infection;
- syphilis;
- rheumatoid arthritis;
- autoimmune damage to the salivary and lacrimal glands or Sjogren's syndrome;
- inflammation of the thyroid gland;
- generalized connective tissue fibrosis or scleroderma;
- oncological processes;
- Infectious mononucleosis;
- alcoholic liver damage.
A significant increase in the indicator occurs exclusively in biliary cirrhosis, also in the so-called CREST syndrome. This syndrome combines 5 diseases in Latin, in which tissue scarring occurs in different organs. These include calcinosis, Raynaud's disease, esophagitis and others.
ELISA blood test: when is it used?
Everyone knows that the treatment of any disease is preceded by diagnosis. The earlier and more accurately the diagnosis is made, the greater the chances of a successful and complete cure for the patient. Elena Gennadievna Koroleva, a pediatric infectious disease specialist at Clinic Expert Tula, talks about what an analysis such as ELISA is, to whom it is prescribed and how it “works”.
- Elena Gennadievna, ELISA blood test - what is it? Tell us about its principle.
— Using an enzyme-linked immunosorbent assay (abbreviated ELISA), specific antibodies, which are immunoglobulin molecules (often designated as Ig), are detected in the blood. Antibodies are produced by the body's immune system in response to the introduction of foreign agents into it - for example, viruses, bacteria. That is, this analysis shows the body’s response to an infection that a person has had or is currently present. This is called: ELISA test for antibodies. The pathogens themselves, their antigens, cannot be found using this type of analysis.
“What are the differences between viruses and bacteria, and what does this mean in the treatment of infectious diseases?” Quote from the material “Viruses and bacteria - what is the fundamental difference?”
There are several classes of immunoglobulins that are produced by the immune system. They are produced depending on the period of introduction of the pathogen into the body and are called differently. For example, the presence of immunoglobulin class M (IgM) indicates an acute phase of the infectious process - which means that the person is sick at that particular moment. But immunoglobulin G (IgG) begins to be produced after two weeks of the body’s fight against infection. If both types are present, this indicates that the infection has been going on for a relatively long time, but the acute phase has not yet ended. But in the case when there is a chronic infection, the appearance of IgM may indicate its exacerbation and the course of the acute phase against the background of a chronic process.
Want to learn more about the immune system? Read our article
— When is enzyme immunoassay prescribed? Is the method only used to diagnose infections?
— The ELISA method is prescribed if the doctor suspects an indirect, hidden infection in the patient, and it remains to be identified. This method also acts as a screening after vaccination: it is used when it is necessary to determine whether a person has protection, say, from measles or other infectious diseases - that is, the analysis shows whether there are antibodies to certain infections, this person must be vaccinated or not.
Read materials on the topic:
Are unvaccinated children the healthiest? Vaccinations: where is the truth and where is the lie? Who invented vaccinations?
— What can blood ELISA detect?
— If the laboratory has certain capabilities, enzyme immunoassay can detect absolutely any infection. For example, an ELISA blood test has been developed for parasites (including helminths), herpes, hepatitis and many other infectious pathogens. To perform the test you need appropriate equipment and screening programs. But there is one more significant point. Modern laboratory analyzers are designed in such a way that ELISA cannot be performed on one person, i.e. you need to wait until there is a certain number of patients who need to do the same analysis, only then will the laboratory take on this work. For example, to identify chickenpox, a laboratory needs at least 50 people. And this does not depend on the whim of its employees - the fact is that it is more cost-effective for the laboratory to do several analyzes at the same time. Therefore, in order to wait less, it is better to contact large laboratories with a high volume of patients.
— How sensitive is the enzyme immunoassay? Is there a possibility that it will not detect its “target” while it is in the body? And if so, why might this be?
— If by purpose we mean the virus itself, then, I repeat, ELISA does not do this; its task is to detect precisely the body’s response to infection, specific antibodies to the pathogen. If the target means antibodies, then, unfortunately, it also happens that ELISA does not detect them. The result may be either a false positive or a false negative. For example, pregnant women with a second blood group often receive a false-positive test for hepatitis C. That is. in fact, there are no antibodies to the hepatitis C virus in this woman’s body, and the analysis says the opposite. Unfortunately, modern medicine finds it difficult to explain this. Therefore, if a doctor observes obvious symptoms, sees that a person is sick, but the ELISA results are negative, he must go further and prescribe another, more specific test.
By the way, a false positive result for hepatitis C can also occur if the person drank red wine the day before the test. In such cases, a lot depends on the experience of the doctor, and it is up to him to decide whether to believe the results of the analysis or continue research.
Read more about hepatitis C in our article
— There is another modern analysis known as PCR - polymerase chain reaction. Can't it replace enzyme immunoassay? If not, why not?
— You know, for an infectious disease specialist these are links in one chain, one process. Unlike ELISA, PCR directly detects the DNA or RNA of the virus or bacteria itself. But there is one peculiarity here. You need to take the secretion directly from the lesion - from where this virus or bacteria multiplies. For example, hepatitis or HIV - yes, they can be detected using PCR by taking blood from a patient. But if a person has pneumonia caused by some exotic fungus, a blood test will show a negative result, and sputum must be taken directly from the lungs through bronchoscopy. If we are talking about other organs - say, the liver - a biopsy is performed.
In addition, PCR may show a false positive result, reacting to some “fragments” of virus molecules - despite the fact that the virus itself, the infection as such, may no longer exist in the body. That is, these two diagnostic methods cannot be opposed. ELISA and PCR are inextricably linked and complement each other, minimizing the risk of making an incorrect diagnosis.
Interviewed by Igor Chichinov
The editors recommend:
Diagnosis of infections using PCR: what is it? Microbe, open your “face”! How dangerous are TORCH infections?
For reference
Koroleva Elena Gennadievna
In 1992 she graduated from the pediatric faculty of the Kyrgyz State Medical Institute.
From 1992 to 1993 - internship in pediatric infections.
She worked at the Republican Infectious Diseases Hospital (Bishkek) as a pediatric infectious disease specialist. Then - a resuscitator in the intensive care unit for infectious patients. In Tula, she worked at the regional children's hospital for more than 10 years, and headed the intensive care unit for 7 years.
Currently, he is a doctor, pediatric infectious disease specialist, pediatric anesthesiologist and resuscitator at the Expert Clinic, Tula. Receives at the address: Tula, st. Boldina, 74.
Tumor Marker 2 (TM 2) – pyruvate kinase
Tumor Marker 2 (TM 2) is a dimer of the isoform of the glycolytic enzyme pyruvate kinase, which is produced by tumor cells and is used as a tumor marker for the early diagnosis of precancerous diseases and colon cancer.
Synonyms Russian
TM-2-pyruvate kinase.
English synonyms
Tumor M2-Pyruvate kinase, tumor M2-PK, Pyruvate kinase type M2.
Research method
Enzyme-linked immunosorbent assay (ELISA).
Units
U/ml (unit per milliliter).
What biomaterial can be used for research?
Cal.
How to properly prepare for research?
Avoid taking laxatives, administering rectal suppositories, oils, limit taking medications that affect intestinal motility (belladonna, pilocarpine, etc.) and the color of stool (iron, bismuth, barium sulfate) for 72 hours before stool collection.
General information about the study
Tumor Marker 2 (TM 2) is a dimer of one of the isoforms of the pyruvate kinase enzyme involved in the glycolysis reaction. In normal cells it is present as a monomer in small quantities, while in tumor cells significant concentrations of the enzyme are produced in the form of a dimer (TM-2). A high concentration of the glycolysis enzyme provides energy expenditure for actively proliferating tumor cells. During the development of precancerous diseases and colon cancer, TM-2 can be detected in stool, which makes it possible to use it as a tumor marker.
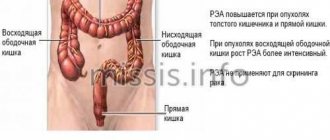
Colon cancer ranks third in prevalence and mortality among all malignant neoplasms. People over 50 are more susceptible to it, however, with some genetic syndromes (adenomatous colon polyposis, Lynch syndrome, etc.), the disease manifests itself at 35-45 years of age.
The “gold standard” for early diagnosis of colon cancer is colonoscopy. However, given its invasiveness and associated risks, it cannot be used as a screening test, unlike the stool TM-2 test, which is a non-invasive method.
The pyruvate kinase test has several advantages over other non-invasive methods. If the presence of heme is detected during a stool occult blood test, this test detects an enzyme specific to tumor cells, which makes it possible to detect both bleeding and non-bleeding neoplasms. This feature causes a higher sensitivity of the test (for comparison: the sensitivity of the TM-2 test is 92.3%, and the sensitivity of the fecal occult blood test is 20-35%). Unlike the stool occult blood test, the result of this test does not depend on diet and can be obtained with a single collection of biomaterial, which is much more convenient for the patient. In addition, the test result is not affected by the use of non-steroidal anti-inflammatory drugs and vitamin C, gastritis, peptic ulcers, intestinal diverticulosis and hemorrhoids, so false positive results are practically excluded.
A study on TM-2 is indicated for patients with symptoms of colon cancer, as well as with risk factors for its development (smoking, obesity, heredity, age over 50 years, alcohol abuse, sedentary lifestyle, ulcerative colitis). The concentration of TM-2 in feces increases in proportion to tumor growth. Therefore, TM-2 testing can be used to determine the stage and prognosis of the disease. Typically, TM-2 concentrations in feces return to normal after surgery for colon cancer. Receiving a positive test result again or an increase in TM-2 in the postoperative period may indicate a relapse of the disease.
A positive test result suggests the presence of intestinal cancer, but does not establish a final diagnosis. To confirm the diagnosis, patients with this result should be referred for additional laboratory and instrumental examinations.
What is the research used for?
- For early diagnosis of dysplastic polyps and adenocarcinoma of the colon.
- To determine the stage of colon adenocarcinoma and give a prognosis of the disease.
- To diagnose relapses of colon adenocarcinoma in the postoperative period.
When is the study scheduled?
- If the patient has factors that increase the risk of developing colon cancer: smoking, obesity, heredity, age over 50 years, alcohol abuse, sedentary lifestyle, ulcerative colitis.
- For symptoms of colon cancer: loss of weight and appetite, blood in the stool, iron deficiency anemia (for right-sided tumors), constipation or diarrhea (for left-sided tumors).
What do the results mean?
Reference values: 0 - 4 U/ml.
Reasons for increased pyruvate kinase levels:
- dysplastic polyp;
- cancer of the colon, sigmoid or rectum.
A decrease in pyruvate kinase levels is not diagnostically significant.
What can influence the result?
TM-2 levels are increased in patients who smoke and in patients with ulcerative colitis, Crohn's disease and colon abscess.
Important Notes
The result of the analysis should be interpreted taking into account the data of some other laboratory and instrumental studies.
Also recommended
- Complete blood count (without leukocyte formula and ESR)
- Leukocyte formula
- Erythrocyte sedimentation rate (ESR)
- C-reactive protein, quantitative
- Fecal occult blood test
- Coprogram
- Carcinoembryonic antigen (CEA)
- Predisposition to colorectal cancer
Who orders the study?
Oncologist, gastroenterologist, surgeon, general practitioner.
Literature
- Koss K, Maxton D, Jankowski JA. Faecal dimeric M2 pyruvate kinase in colorectal cancer and polyps correlates with tumor staging and surgical intervention. Colorectal Dis. 2008 Mar;10(3):244-8.
- Hathurusinghe HR, Goonetilleke KS, Siriwardena AK. Current status of tumor M2 pyruvate kinase (tumor M2-PK) as a biomarker of gastrointestinal malignancy. Ann Surg Oncol. 2007 Oct;14(10):2714-20.
- Haug U, Rothenbacher D, Wente MN, Seiler CM, Stegmaier C, Brenner H. Tumour M2-PK as a stool marker for colorectal cancer: comparative analysis in a large sample of unselected older adults vs colorectal cancer patients. Br J Cancer. 2007 May 7;96(9):1329-34.
- Tonus C, Neupert G, Sellinger M. Colorectal cancer screening by non-invasive metabolic biomarker fecal tumor M2-PK. World J Gastroenterol. 2006 Nov 21;12(43):7007-11.
- Young GP, Cole S. New stool screening tests for colorectal cancer. Digestion. 2007;76(1):26-33.