Differential diagnosis of endometritis in women: identification of direct and indirect signs.
Is it possible to see endometritis on an ultrasound? The method helps to detect direct symptoms of acute endometritis in 30-40% of patients. Indirect signs of chronic endometritis are found more often. However, they also occur in other diseases of the reproductive organ. It is impossible to draw an unambiguous conclusion from them.
Cost of endometritis treatment
| Procedures and operations | ||
| Initial consultation with a gynecologist | from 2300 rub | Select priceWe will select the most advantageous offer for you and provide it to you immediatelyBy clicking on the button, you consent to the processing of your personal data |
| Ultrasound gynecological expert | from 2800 rub | Select priceWe will select the most advantageous offer for you and provide it to you immediatelyBy clicking on the button, you consent to the processing of your personal data |
| Endometrial biopsy | from 3500 rub. | Select priceWe will select the most advantageous offer for you and provide it to you immediatelyBy clicking on the button, you consent to the processing of your personal data |
| Hysteroscopy of the uterus | from 20500 rub. | Select priceWe will select the most advantageous offer for you and provide it to you immediatelyBy clicking on the button, you consent to the processing of your personal data |
| Hysterosalpingoscopy | from 7000 rub | Select priceWe will select the most advantageous offer for you and provide it to you immediatelyBy clicking on the button, you consent to the processing of your personal data |
| Cytology smear | from 800 rub | Select priceWe will select the most advantageous offer for you and provide it to you immediatelyBy clicking on the button, you consent to the processing of your personal data |
| Ureaplasma parvum (PCR) | from 450 rub | Select priceWe will select the most advantageous offer for you and provide it to you immediatelyBy clicking on the button, you consent to the processing of your personal data |
| Ureaplasma spp (PCR) | from 450 rub | Select priceWe will select the most advantageous offer for you and provide it to you immediatelyBy clicking on the button, you consent to the processing of your personal data |
How to diagnose chronic endometritis?
To clarify the diagnosis, additional examination methods are used. They allow a comprehensive assessment of the patient’s condition. The parameters obtained by ultrasound and test results are sufficient to make a reliable diagnosis.
Diagnosis of acute endometritis is based on determining the symptoms of the infectious and inflammatory process. They, in combination with the clinical picture of the disease and risk factors, help to make the correct conclusion.
Dr. Matthew Lukis says endometritis refers to inflammation or infection in the endometrium. Endometritis can be acute or chronic and can occur after obstetric and gynecological procedures, for example, after childbirth or miscarriage, or in non-sterile conditions through inflammatory diseases of the pelvic organs.
An ultrasound examination does not reveal the inflammation itself, but the consequences that have arisen against its background. The ultrasound photo of endometritis shows the structural and anatomical transformations of the genital organ. When diagnosing, risk factors must be clarified. They differentiate echo signs.
Risk factors
- The disease is provoked by:
- abortions;
- intrauterine device;
- childbirth;
- diagnostic and gynecological instrumental interventions;
- miscarriages;
- C-section.
Consultation with a doctor The coordinator will answer all your questions and make an appointment at a time convenient for you.
By clicking on the button, you consent to the processing of your personal data
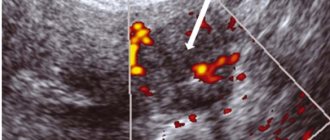
In case of inflammation that occurs after an abortion or injury, an ultrasound scan reveals symptoms of infection. In this case, the doctor notes the appearance of an echo-negative segment, which corresponds to a pathogenic infiltrate with swelling. In the echo-positive segment, blood clots and a significant expansion of the uterine cavity are observed.
Expert opinion In case of endometritis that has developed after an abortion or any other traumatic impact, signs of an inflammatory process can be detected, which manifest themselves as an echo-negative zone corresponding to an inflammatory infiltrate with perifocal edema, an echo-positive zone of varying density, which corresponds to blood clots in the uterine cavity, and also a significant expansion of the uterine cavity.
Litvinov Vladimir Valentinovich Reproductologist, obstetrician-gynecologist Experience 36 years
Ask a clarifying question
Endometritis that occurs due to the installation of an intrauterine device gives characteristic echo signs during ultrasound examination. They, together with the clinical picture that appears 3-5 days after gynecological intervention, make it possible to make a reliable diagnosis.
How is ultrasound performed? When treating a disease, ultrasound is performed dynamically. The woman is examined more than once in 3-5 days. Thanks to the study, the patient’s condition and the dynamics of the therapy are determined. The decline in inflammation with endometritis is visible on ultrasound. If no positive changes are observed, auxiliary studies are performed and the treatment algorithm is adjusted.
The ultrasound method is an approximate diagnosis of endometritis and allows it to be differentiated from other types of pathologies.
Chronic endometritis on ultrasound
According to Dr. L. Savelli, the diagnosis of endometritis is often challenging because signs and symptoms are nonspecific and sonographic findings vary, including thickening and irregularity of the endometrium and fluid or other fluid accumulated in the endometrial cavity. There are cases when the diagnosis was suggested by transvaginal ultrasound by demonstrating gas in the endometrial cavity.
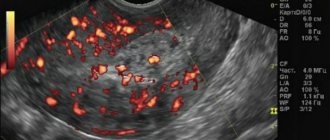
In chronic endometritis, inflammation is sluggish. It cannot be detected by ultrasound examination of the intrauterine cavity. But it leaves marks on the mucous layer. The structure of the endometrium and uterus is modified. In this case, endometritis on ultrasound looks like pathological transformations.
Ultrasound signs of uterine endometritis.
In the chronic form of the disease, characteristic echo signs of endometritis are detected:
- Reducing the thickness of the mucous layer. With prolonged inflammation, the endometrium becomes significantly thinner. Healthy mucous membranes are replaced by connective tissue structures.
- Increased thickness of the mucous layer. Bioactive compounds present in the affected area cause endometrial hyperplasia. As a result, the mucous layer thickens.
- Is endometritis visible on ultrasound? The doctor observes the marks left by inflammation. Cavities form on the mucous layer, which are clearly visible on the computer monitor. Pathological formations appear with cysts and are formed due to the activity of microbes.
- The size of the uterus changes. The uterine body increases in size due to the accumulation of exudate in its cavity. The echo sign appears during the proliferative period of the menstrual cycle.
- The antinomic position of the reproductive organ has been changed. Adhesions that form in the uterine cavity can change the correct position of the organ body. Sometimes this leads to pelvic pain and infertility.
- Adhesions in the uterine cavity. Prolonged development of the disease leads to the formation of adhesions on the endometrium. They are easily detected by ultrasound.
Entire discussions are taking place on forums about whether endometritis can be determined by ultrasound or not. Some women write that they were diagnosed after an ultrasound examination. Others categorically state that this cannot happen; endometritis is determined by test results.
Why do you need to do an ultrasound? Doctors consider ultrasound to be an approximate way to detect endometritis. It is important not only to see the signs of the disease, they must be compared with other studies and test results, and the correct conclusions must be drawn.
Expert opinion Regardless of the type of procedure, it is possible to diagnose signs of endometritis on ultrasound only from the second stage of the disease. Experts advise undergoing an ultrasound examination to identify this pathology in the second half of the menstrual cycle, a few days before the onset of bleeding. For example, if the cycle is 30 days, then you can go for an ultrasound examination for endometritis on the 26th-28th.
Litvinov Vladimir Valentinovich Reproductologist, obstetrician-gynecologist Experience 36 years
Ask a clarifying question
Patients sometimes confuse two different techniques: ultrasound cavitation and ultrasound. Ultrasound cavitation of the uterine cavity is not an ultrasound, but a hardware method for treating endometritis. In Moscow, ultrasound cavitation of endometritis is carried out professionally.
Standard questions
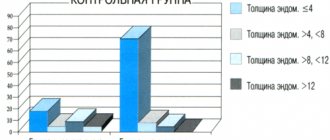
With postmenopausal women, everything is simple. Their endometrium is considered normal if its thickness is at least 6 mm and it has an even structure. And in women of reproductive age, the normal endometrium at different stages of the monthly cycle has different characteristics:
- Beginning of the cycle – stage 1. The endometrium is heterogeneous. Its thickness is 5-9 mm. The sound travels great. There is no separation into layers.
- The middle of the cycle is stage 2. The endometrium thickens. Echogenicity decreases, although sound conductivity remains very high.
- End of the cycle – 3rd period. There is a pronounced separation into layers and superechogenicity. Size – 9-10 mm. This stage is the most important, since the most favorable environment for the attachment of the egg is formed.
In some women, the development of the endometrium does not coincide with the phases of the menstrual cycle. This is primarily due to the following factors:
- possible hormonal imbalance;
- injury that occurred during curettage;
- insufficient development of the uterus;
- poor blood circulation in the uterus or pelvic organs.
When is an ultrasound performed?
If endometritis is suspected, what day of the cycle is an ultrasound done? The examination is performed in phase 2 of the menstrual cycle, before the onset of bleeding. With a 30-day cycle, diagnosis is scheduled on days 26-28.
This is due to the fact that pathological changes are more pronounced during menstruation. Symptoms of the disease are easier to detect during this time period. In some cases, ultrasound is performed in phase 1 of the cycle, 5-7 days after the bleeding has stopped.
Ultrasound allows you to make a tentative diagnosis. To definitively confirm endometritis, a detailed examination is carried out using a biopsy or hysteroscopy.
If adequate treatment for endometritis is not undertaken in a timely manner, the infection can gradually affect the fallopian tubes and also affect the deep uterine layers.
What determines the success of implantation?
The success of IVF depends 90% on the quality of the embryos.
The highest pregnancy rate is observed when transferring embryos on the 5th day of development - blastocysts. Whether or not the embryo takes root after transfer to the uterus depends on many factors, the main one of which is the correspondence of the stages of development of the embryo and endometrium. The embryo must enter the uterus at a strictly defined moment when the “implantation window is open.” If this does not happen, pregnancy will not occur. The implantation window exists for several days during the luteal phase of the menstrual cycle and is the result of the influence of many factors on the endometrium that provide the conditions for embryo implantation.
Every month, the endometrium is completely renewed - during menstruation, its cells are rejected and in their place, under the influence of sex hormones - estrogens - new ones begin to grow. The endometrium reaches its maximum thickness after ovulation. On the surface of endometrial cells, under the influence of progesterone, pinopodia are formed, which act as a link between the embryo and the wall of the uterine cavity (photo of pinopodia). If this process is disrupted, pregnancy will not occur.
The doctor assesses the condition of the endometrium by the thickness of the endometrium and its structure during ultrasound. Insufficient or excessive endometrial thickness (thin or too thick endometrium) can disrupt the implantation process. The optimal thickness of the endometrium on the day of embryo transfer is 8-12 mm. This does not mean that pregnancy is impossible with less or greater thickness of the endometrium, however, the likelihood of pregnancy is much lower.