Pelvic inflammatory disease is an ascending infection of the uterus, its appendages and the pelvic peritoneum.
These include:
- endometritis (inflammation of the lining of the uterus);
- metroendometritis (inflammation of the mucous and muscular lining of the uterus);
- parametritis (inflammation extends to the periuterine space);
- salpingoophoritis (inflammation of the uterine appendages - tubes and ovaries);
- pelvioperitonitis (common inflammation, including the pelvic peritoneum).
You can get information about the most common inflammatory diseases of the pelvic organs in this section.
Endometritis
Acute endometritis Most often occurs after abortion, childbirth or diagnostic curettage of the uterus. Clinical signs of acute endometritis usually appear 3-4 days after infection. The temperature rises, the pulse quickens, there is chilling, there are all signs of an inflammatory process in the body and according to a clinical examination. The discharge is serous-purulent, often sanguineous for a long time, which is associated with a delay in the regeneration of the mucous membrane. The acute stage lasts 8-10 days. With proper antibacterial treatment, the process ends and less often becomes subacute or chronic.
Chronic endometritis The frequency of chronic endometritis averages 14%. In recent years, there has been a tendency towards its increase, which is associated with the widespread use of intrauterine devices and the increase in the number of abortions.
As a rule, chronic endometritis occurs as a result of untreated acute postpartum or post-abortion endometritis; its development is often facilitated by repeated intrauterine interventions due to uterine bleeding.
The diagnosis can be indirectly made by ultrasound signs, but it can be 100% confirmed only by hysteroscopy and histological examination of the endometrium!!
Quite often, chronic endometritis is a uterine factor of infertility, and requires long-term and serious treatment after confirmation of the diagnosis.
When the infection spreads upward from the uterine cavity into the fallopian tubes, salpingoophoritis develops, i.e. inflammation of the uterine appendages.
General characteristics of non-gynecological tumors
We found that intraperitoneal tumors predominated over extraperitoneal tumors (84/92 (91.3%) vs. 8/92 (8.7%)). Among intraperitoneal tumors, 39/84 (46.3%) were located in the ovaries; the remaining 45 (53.7%) were located in the visceral peritoneum or in the appendix area outside the ovaries. Intraperitoneal tumors were more often unilateral (73/84 (87.0%)). A wide range of sizes was observed (largest diameter, range, 20-300 (average 120 mm).
Pathology located above the pelvis and determined transabdominally was observed in 23/92 (25.0%) tumors.
The tumors were mostly solid (49/92 (53.3%)) or multilocular-solid (38/92 (41.3%)). A small proportion of tumors were unilocular-solid (5/92 (5.4%)). There were no tumors without a solid component. If there were septa (in multilocular-solid tumors), they were always vascularized and of varying thickness. In the majority (35/38 (92.1%)), the septa were >5 mm wide. Papillary growths were rarely detected and were recorded only in the case of colorectal cancer metastases (10/32 (31.3%)).
The combination of gray scale and Doppler showed changes that suggested necrosis, which was observed in more than half (47/92 (51.1%)) of the tumors. A large amount of necrotic tissue was found in the solid part of the tumor (36/43 (83.7%) had a multilocular tumor with a solid component). In most cases, the solid component of a multilocular tumor was heterogeneous (ie, mixed echogenicity) (34/43; 79.2%).
Based on subjective assessment, tumor vascularity was given a mean score of 3. Both resistance index (RI) < index 0.4 and pulsatility index (PI) < 0.6 were recorded in 65/92 (70.6%) tumors. Peak systolic velocity (PSV) ranged from 7.7 to 30.9 (mean 15.1) cm/s.
When pressed with a vaginal probe, only 24/92 (26.1%) of the tumors were elastic, while the majority of them (68/92 (73.9%)) were firm. Twenty of 92 (22.5%) tumors were fixed, 38/92 (40.8%) were semi-fixed, and 34/92 (36.6%) were mobile.
Carcinomatosis was found in one quarter of tumors only in combination with ascites (21/92; 22.8%). Parenchymal metastases were observed in 31/92 (33.7%) tumors, with liver metastases in all cases. Ascites is present in 85.9% (79/92) of patients.
Salpingo-oophoritis
Salpingoophoritis is the most common form of inflammatory diseases of the pelvic organs. Every fifth woman who has suffered inflammation of the uterine appendages faces infertility, which is associated with the development of adhesions in the pelvis!
It is known that the fallopian tubes are most often affected by bacterial infections. This is due to the characteristics of the blood supply and anatomical structure. However, the depth of damage to the tissue of the fallopian tubes depends on the pathogen that caused the inflammation and the duration of the process.
Characteristic signs of inflammation of the uterine appendages: increased body temperature, pain in the lower abdomen, pain during gynecological examination, characteristic ultrasound signs.
Currently, in half of the patients, inflammation of the appendages has a mild, or rather, almost asymptomatic course! This complicates diagnosis, delays the appointment of timely correct treatment, leads to the formation of adhesions in the pelvis and infertility.
Quite often, patients simply do not know that they have previously suffered inflammation of the uterine appendages, and only with a substantive interview is it possible to identify erased but characteristic complaints.
Evaluation of the data obtained
Our assessment was carried out retrospectively by reviewing surviving examination reports. In case of uncertainty or lack of clarity in the report, stored still images or video clips were used for clarification, without knowledge of the histological diagnosis.
Tumors with metastases in the ovaries were designated as ovarian cancer. If the tumor was limited to the ovarian surface only, with no ovarian stroma involved, it was classified as ovarian with carcinomatosis. Tumors that were attached to the pelvic wall and supplied by the external, internal, or common iliac artery or tumors located clearly beneath the parietal peritoneum were classified as retroperitoneal. Heterogeneous, avascular areas of mixed echogenicity with blurred boundaries adjacent to vascularized tissue were classified as areas of probable necrosis (Fig. 1).
Fig.1. Necrosis: A heterogeneous avascular area with irregular edges (arrow) surrounded by tissue that has a blood supply.
The elasticity of the tumors was assessed by pressure, which was performed using a vaginal sensor with simultaneous pressure on the abdominal wall during palpation (in order to avoid tumor movement), and was classified as elastic or rigid.
The mobility of tumors was assessed by their movement in relation to adjacent structures when the examiner's hand presses on the abdominal wall while scanning with a transvaginal or abdominal ultrasound probe. A tumor is considered mobile when it moves freely along its entire perimeter in relation to neighboring structures. Semi-fixed - if it is securely fixed to at least part of its perimeter or neighboring structures have not shown any slip. Fixed - if it was completely motionless.
Salpingitis (inflammation of the fallopian tubes)
Acute salpingitis begins with swelling of the mucous membrane of the tube, the cilia covering the inside of the fallopian tubes are affected, and inflammatory fluid accumulates in the tube. If untreated, the fallopian tube fills with pus, which flows from the fallopian tubes into the pelvis, which leads to inflammation of the peritoneum (peritonitis) and the formation of adhesions. Inflammation also leads to tissue destruction, which is accompanied by the formation of abscesses (demarcated cavities filled with pus, which also contain destroyed organs when they are involved).
The accumulation of fluid in the pipe leads to its stretching, which is called “hydrosalpinx (salpinx – pipe; hydro-liquid). When it suppurates, a “pyosalpinx” is formed, literally, pus in the tube (pyo-pus). In this situation, emergency surgical treatment is required to avoid the spread of purulent inflammation to other organs of the pelvis and abdominal cavity.

Figure 1. Dilated fallopian tube with fluid contents.
The figure shows an enlarged fallopian tube with liquid contents. The vascular pattern is pronounced. Laparoscopy was performed 6 hours after the onset of the disease. The inflammation has not yet reached the purulent stage. It is planned to perform plasty of the fallopian tube, washing the abdominal cavity and pelvis with solutions of antiseptics and antibiotics.
Chronic salpingitis is the predominant form of inflammatory diseases of the pelvic organs. The process may be a continuation of the acute one, however, it is possible that at the beginning of the disease there were no symptoms inherent in the acute stage. Most often, chronic salpingitis is the result of untreated acute salpingitis.
It has been established that the chronic stage is characterized by the presence of infiltrates, loss of physiological functions of the mucous and muscular membranes of the fallopian tube, development of connective tissue; with a long course, obstruction of the fallopian tubes often occurs with or without the formation of hydrosalpincos, with the formation of adhesions around the ovaries. Formed adhesions prevent the capture of the egg, which is also one of the causes of infertility.
The clinical manifestations of chronic salpingoophoritis are varied; some symptoms are associated primarily not with changes in the uterine appendages, but with neurosis, which is often observed with a long course and frequent relapses.
The main complaint is dull, aching pain, aggravated by cold, colds or during menstruation. “Referred” pain is also characteristic, which is usually felt in the groin areas, in the sacral area or in the vagina. In half of the patients, menstrual dysfunction is recorded, since chronic inflammation also leads to disruption of the ovaries (decreased function, lack of ovulation).
Anatomical and functional changes in the fallopian tubes and disruption of the ovaries during chronic inflammation are the cause of infertility, and also lead to pathological outcomes during pregnancy (spontaneous miscarriages, ectopic pregnancy)!!!
Interpretation of ultrasound results
Only an experienced doctor can correctly decipher the results of an ultrasound examination.
Pelvic ultrasound makes it possible to detect:
- Congenital developmental anomalies: Ultrasound, especially 3-dimensional, allows you to diagnose developmental anomalies of the uterus (bicornuate, unicornuate, saddle-shaped, duplex uterus).
- Endometriosis is a pathological process characterized by the spread of the endometrium beyond the uterine cavity (ovaries, uterine walls, peritoneum, etc.). Ultrasound can reveal internal endometriosis or adenomyosis (growth of the endometrium into the wall of the uterus), as well as endometriotic ovarian cysts. Diagnosis of endometriosis is of greater importance for predicting the possibility of pregnancy and its bearing, since endometriosis can cause infertility.
- Congenital developmental anomalies. The presence of such anomalies can cause infertility, increase the risk of premature birth, intrauterine fetal death, and disruption of labor.
- Diagnosis of pregnancy: Ultrasound allows you to diagnose pregnancy starting from 3 to 4 weeks. Note that short periods of pregnancy are determined only with the help of a transvaginal sensor, a device with good resolution. Different types of ectopic pregnancy are diagnosed (tubal - when the fertilized egg is attached to the fallopian tube; ovarian - when it is attached to the ovary; cervical - when it is attached to the cervix). This allows the woman to remain healthy.
- Uterine fibroids are a benign tumor of the female reproductive system. During an ultrasound, the presence, location, number and size of myomatous nodes are determined. In addition, this method allows you to monitor their growth rate over time, so the examination is done several times a year. Diagnosis of fibroids is important when preparing for conception, since its presence can affect the course of pregnancy.
You can also detect hyperplastic processes of the endometrium (hyperplasia, malignant endometrial tumors, polyps) and ovarian mass formations.
Diagnostics
The ultrasound method is not sufficiently informative in diagnosing salpingoophoritis. It allows you to identify only space-occupying formations in the pelvis. Those. With ultrasound, it is possible to see the fallopian tubes, which are filled with fluid (with hydro- or pyosalpinx), as well as with the formation of abscesses (with purulent melting of the fallopian tubes and ovaries). Therefore, the diagnosis of acute inflammatory diseases of the uterine appendages is mainly based on clinical data and gynecological examination data.
How is a pelvic ultrasound performed?
The patient lies down on the couch, having laid out a diaper in advance, with his head towards the doctor (ultrasound machine), exposing his stomach, as well as his lower abdomen. The doctor lubricates the ultrasound sensor with gel (during transvaginal ultrasound, he puts a condom on the sensor and lubricates it with gel), and then begins to move the sensor over the patient, occasionally pressing in order to view certain pelvic organs from a different angle.
The procedure itself is painless, with the exception of diagnostics in cases of acute inflammatory processes of the pelvic organs. An ultrasound lasts about 10-20 minutes, depending on the purpose of the study.
Treatment
Treatment of patients with acute salpingoophoritis should be carried out in a hospital setting.
The main place in treatment belongs to antibiotics, the effectiveness of which is determined by the properties of the pathogen and its sensitivity.
In the formation of purulent inflammation of the uterine appendages, the only effective method for 100% diagnosis, treatment and preservation of fertility is laparoscopy!!!
Chronic diseases of the uterine appendages are accompanied by the formation of adhesions in the pelvis, which disrupts the patency of the fallopian tubes, leads to infertility and also requires planned surgical treatment (laparoscopy).
Colorectal cancer metastases
Typical signs of colorectal cancer metastases were: the round shape of the caudal part of the tumor, the presence of papillary growths and the presence of necrosis of the solid part. The tumors were predominantly with hyperechoic septa, mainly with hypoechoic or heterogeneous solid parts. Existing papillary growths, from isoechoic to hyperechoic, growing from thin septa and being specific for colorectal cancer metastases, were observed in 5/32 (15.6%) tumors (Fig. 2).
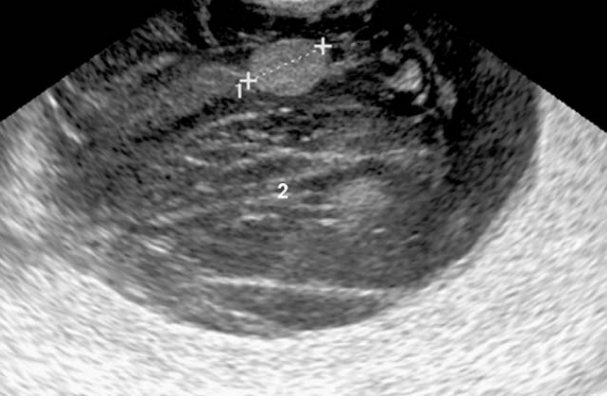
Fig.2. Metastases of colorectal cancer: multilocular solid tumor with a typical round shape (2) with papillary growths from the septa (1).
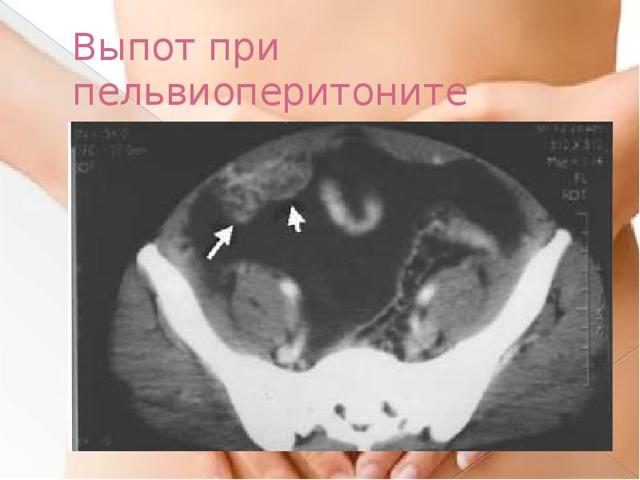
Pelvioperitonitis
Pelvioperitonitis (inflammation of the pelvic peritoneum) is one of the most dangerous complications of inflammatory diseases of the pelvic organs and already poses a threat to a woman’s life!
This complication occurs secondary to the penetration of microorganisms from the fallopian tube. The primary focus of infection can be not only in the fallopian tubes, but also in the ovaries, uterus, pelvic tissue, appendix and other organs.
If treated incorrectly, the development of pelvioperitonitis is accompanied by septic shock, which is one of the causes of death in patients.
With the development of this complication, immediate surgical treatment in an adequate volume is required, aimed primarily at removing the source of purulent infection!!!
Traditional methods
Today, therapy based on alternative medicine recipes offers a wide variety of medicinal plants and agents that have a high level of antibacterial action and anti-inflammatory properties:
- These can be herbs such as elecampane, sage and St. John's wort.
- Field chamomile flowers are in every medicine cabinet, and they promote a speedy recovery by eliminating pain and inflammation.
- The herb hogweed or red brush helps restore the menstrual cycle after a course of treatment or surgery.
Additional traditional medicine allows the use of infusions, decoctions for douching and herbal tampons.
But it is worth understanding that the use of herbal remedies cannot be the main treatment; they are used only as additional therapy. Each recipe, despite its simplicity, has some contraindications, so even herbal medicine should be discussed with a doctor.
Alternative treatment methods help prevent an increase in fluid in the free space of the pelvic organs.
Lymphoma (non-Hodgkin's lymphomas only)
As a rule, non-Hodgkin lymphoma was located extraperitoneally in the pelvis, had a dense structure and heterogeneous content in the form of hyperechoic and hypoechoic areas (Fig. 4). Doppler sonography showed hypervascularization of the tumor.
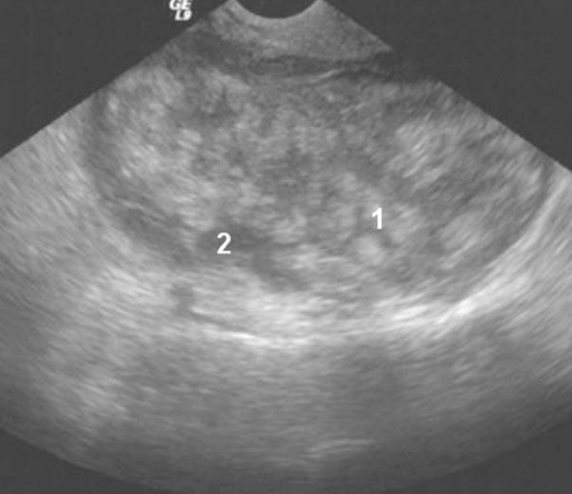
Fig.4. Metastatic lymphoma: a well-defined heterogeneous tumor with multiple hyperechoic inclusions (1) and hypoechoic areas (2).
Symptoms and photos
Varicose veins in the pelvis have specific symptoms. Frequent signs of vasodilation in women are:
- Irregularities in the menstrual cycle also indicate varicose thickening of the veins of the female pelvic organs.
- Increased sensitivity of the skin in the perineum, sensitivity of the vaginal mucosa.
- Severe intermittent or constant pain. It often becomes more intense during menopause or after ovulation.
- Vaginal discharge: colorless or slightly white.
- Pain in the last stage of pregnancy, during sex or towards the end of the day.
- In the presence of varicose veins, there is a slight swelling of the vagina and vulva.
- Heaviness, pressure on the pelvic area is another possible symptom of varicose veins.
The photo below shows how the disease manifests itself in women.
Semiquantitative ultrasound assessment of amniotic fluid volume
There are two main semi-quantitative systems for measuring AF volume in clinical use: AFI and MVK (also known as deepest (maximum) vertical pocket). It was first proposed to use this parameter in the 1998 academic year. Moore and Brace. Since then, there have been several studies evaluating the relationship between AF volume (both AFI and/or MVK) and dye-detected AF volume.
Disappointingly, sonographic estimates of normal AF volume do not agree well with direct or dye-determined methods (sensitivity, 71%-98%). For oligohydramnios, when detected by ultrasound methods compared to dye detection or directly measured volumes, the sensitivity is low, ranging from 6.7% to 27%.
AFI is determined by summing the four vertical quadrants with the sensor placed at a sagittal location perpendicular to the floor. This parameter was first introduced by Phelan and colleagues in 1987 for full-term pregnancies. This measurement system was subsequently expanded to include second and third trimester pregnancies (16–42 weeks of gestation) and pregnancy-specific normal ranges were developed
AFI. The MVK technique is also widely used with the 2-cm cut being most widely accepted clinically as distinguishing normal from low AF. The ultrasound threshold for low AF volume is generally accepted as an AFI of 5 cm or less or an MVP of 2 cm or less because these values have been associated with an increased risk of adverse perinatal outcomes. Interestingly, the upper limit of AFI for defining polyhydramnios is less well defined, but is typically greater than 24 cm (or MVP >8 cm).
Assessment of amniotic fluid in multiple pregnancies
In multiple pregnancies, there is an initial increase in adverse perinatal outcomes compared to single pregnancies. Having a twin pregnancy adds another layer of complexity to assessing the extent of AF in terms of assessment methods, cause of AF deviation, and management of the condition.
The dividing membrane in diamniotic multiple pregnancies complicates the performance and reproducibility of ultrasound studies of AF. A recent systematic review assessing AF volume in twin pregnancies found that AFI and/or MVK were commonly used for ultrasound volume studies. AFI and MVK performed similarly when compared with dye dilution methods, but questions were raised about the reliability of AFI in multiple pregnancies.
It has been reported that there is no significant association between pregnancy and MVK in diamniotic twins, although a recent study of multiple pregnancies (uncomplicated monochorionic diamniotic) demonstrated that the condition does not apply to this subset.
Most centers have switched to using MVK for multiple pregnancies due to the ease of use, reliability, and more reliable performance characteristics of this option for oligohydramnios. As a rule^
- An MVK of less than 2 cm is used to define oligohydramnios;
- MVK greater than 8 cm to define polyhydramnios;
- For monochorionic twins, an MVK greater than 10 cm is used to define polyhydramnios after 20 weeks of gestation.
Conclusion
We described the ultrasound characteristics of the most common extragenital tumors identified in the pelvic region in the study population. Knowledge of specific ultrasound characteristics of non-gynecological tumors can change the focus of diagnostic efforts in cases of identifying tumors in which pelvic metastases are only the first sign of a tumor with a different primary location, which helps determine the optimal tactics for patient management. A portable ultrasound machine is suitable for conducting research, but we recommend using a device from GE Voluson E8 .
Krukenberg tumor (metastatic gastric cancer only)
Krukenberg's cancer was characterized as an ovarian tumor of heterogeneous echostructure, with predominantly isoechoic and hypoechoic areas, as well as the potential appearance of necrosis (Fig. 5) with an uneven internal contour, but with a smooth surface. Vascularization of Krukenberg tumors (outside the area of potential necrosis) was assessed as hypervascularized.
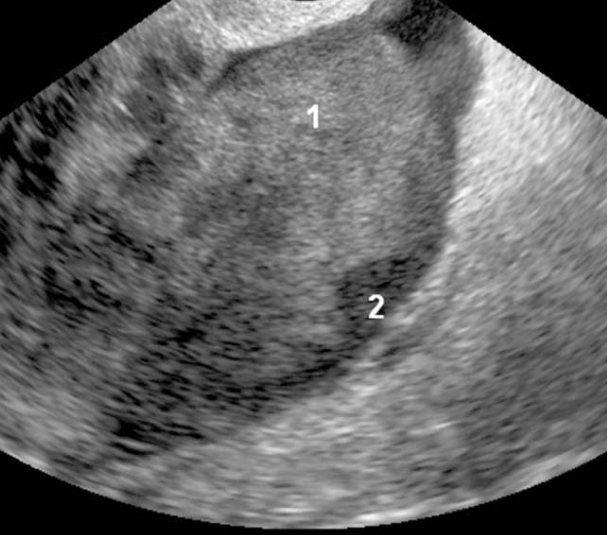
Fig.5. Krukenberg tumor (gastric cancer metastases): a hard (solid), with an uneven internal surface and a smooth surface, heterogeneous tumor that is mainly isoechoic, but hyperechoic (1) and hypoechoic (2) areas are visualized.
Preparation for an MRI study of the pelvis in men:
- The day before the study, stop drinking carbonated drinks, foods rich in fiber (cabbage, raw vegetables and fruits, legumes, black bread), and fermented milk products;
- On the eve of the study, cleanse the intestines (microenemas or naturally);
- On the day of the study, take activated charcoal, and in case of severe gas formation, take 1-2 capsules of espumizan. 30 minutes before the test, take 2 tablets of no-shpa;
- When examining the urinary system, an average filling of the bladder is necessary.
What does fluid in the pelvis mean?
The accumulation of free fluid in the pelvis (effusion) means that a dangerous pathological process is developing in the body.
At the first stage, the clinical picture of the accumulation of free fluid in the pelvis does not appear in any way. Very rarely (no more than 10% of patients) the pathological process of effusion occurs against a background of discomfort, burning sensation and atypical vaginal discharge.
The only way to accurately determine fluid accumulation is by ultrasound. Based on the results of the examination, the doctor determines the degree of development of the pathology, the need and regimen of treatment therapy.










