Find out more about diseases starting with the letter “N”: Sleep disturbance; Narcolepsy; Hereditary cerebellar ataxia of Pierre-Marie; Spinal circulatory disorders; Trigeminal neuralgia; Neuralgia of the submandibular and sublingual nodes; Neuralgia of the glossopharyngeal node; Neuralgia of the ear ganglion; Neurasthenia; Neural amyotrophy of Charcot-Marie-Tooth; Acoustic neuroma; Neuroma; Optic neuritis; Pharyngeal neuritis; Neuritis of the facial nerve; Neuritis; Obsessive-compulsive neurosis; Pharyngeal neurosis; Neuroses; Neurosis-like stuttering; Femoral nerve neuropathy.
Description of the disease
The pathological condition is characterized by damage to the nerve branch of the facial part. Most often one side is affected. A feature of the disease is characteristic pain, which has a certain periodicity. Soreness is replaced by a long attenuation of the syndrome. The first mentions of the disease date back to the second half of the 17th century. And in the middle of the 18th century, the disease was identified as a separate category. The pathology was studied in detail in 1773 by the British medical officer Fotheringle. Initially, the disease received the name of this scientist, then “trigeminal neuralgia” became a more common scientific name appearing in the literature. The number of people suffering from this disorder is 3-4 people per 10,000 population. The disease occurs in various age categories, however, people who have crossed the age threshold of 50 years are most often susceptible to it. Female neuralgia occurs many times more often than among the male population.
Prevention
Prevention measures:
- balanced diet;
- limiting alcohol consumption, quitting smoking, reducing factors that lead to intoxication of the body;
- active sports;
- do not overcool;
- increase stress resistance;
- avoid injury;
- timely treatment of respiratory and infectious diseases;
- preventive examination at the dentist several times a year, dental treatment;
- timely contact a neurologist if pain occurs.
Sources of pathology
Many primary causal factors causing the disease in question have been described. The main one is compression of the nerve column located in the neural branch of the facial part. Such compression can be caused by the following factors:
- Disturbances in the vascular network. As a result of the expansion of vascular canals, their pathological curvature, and the development of aneurysms, they constantly come into contact with adjacent nerve branches, which leads to compression and the appearance of pain in this area.
- Tumor, cystic formations. Pathological growth of soft and bone tissues of the skull affects nearby nerves. As the volume of the formation increases, the neural channels are gradually compressed.
- Deformation of the skull. As a result of external traumatic injury, chronic inflammation in the sinuses and pathways, these pathways become narrowed, which also affects the correct location of neural branches. Dental problems associated with malocclusion and orthodontic problems also lead to such degeneration.

Rarely, there is also an infectious lesion associated with the activity of the herpes virus, bacterial infection as a result of a violation of the integrity of the soft tissues of the oral cavity and nasopharynx.
Common factors that provoke a neurological disorder are:
- sudden, systematic hypothermia of the body;
- unsuccessful instrumental intervention during dental procedures;
- intensive chewing, increased load on the jaws;
- loss of immune defense as a result of past illnesses.
To subsequently get rid of the pathology and prescribe the correct treatment, it is important to differentiate trigeminal neuralgia. In the medical literature, it is customary to divide the anomaly into two main categories:
- Idiopathic neuralgia. It is a primary category caused by compression of the nerve root in the area of the intracerebral trunk. The most common source of this pathology is the incorrect relationship between nearby vessels and nerve fibers.
- Symptomatic neuralgia. It acts as a secondary category, caused by complications due to the growth of tumors, inflammatory processes, and deformation of bone structures.
Where is the trigeminal nerve located on the face?
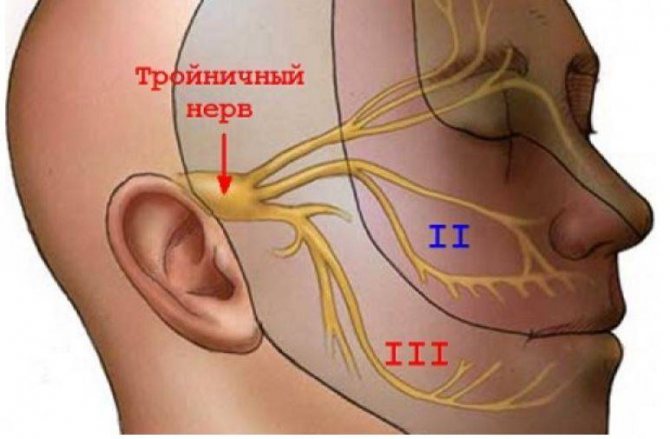
Scheme of location and division into branches of the trigeminal nerve
The structure under discussion is a pair and is localized on both sides of the head. The trigeminal nerve nuclei are located in the brainstem. Protruding from the latter, the sensitive and motor portions of the tract enter the Gasserian node, after which they are divided into three large branches:
I - Ocular. Responsible for sensitivity:
- skin of the forehead, parietal, temporal areas, dorsum of the nose;
- conjunctiva (mucous membrane of the eyeball);
- lacrimal gland;
- mucous membrane of the nasal cavity and paranasal sinuses (partially).
II - Maxillary. Innervates:
- part of the dura mater of the brain;
- lower eyelid;
- outer corner of the eye;
- the anterior part of the temple area;
- top of cheek;
- wing of the nose;
- mucous membrane and skin of the upper lip;
- sky;
- teeth on the upper jaw.
III - Mandibular. Controls sensitivity:
- dura mater of the brain (partially);
- the lower half of the skin and mucous membrane of the cheek;
- chin area;
- lower lip;
- auricle;
- external auditory canal;
- partially the outer surface of the eardrum;
- floor of the mouth;
- teeth on the lower jaw;
- anterior ⅔ of the tongue;
The mandibular part of the trigeminal nerve is responsible for muscle movement:
- maxillohyoid;
- chewable;
- eardrum;
- palatine curtain;
- digastric (anterior abdomen).
Symptoms of trigeminal neuralgia

The main symptom of the disease is severe, sharp pain that occurs on one of the peripheries of the face, moving towards the central part. The patient describes the syndrome as a sharp lumbago, an electric shock. The intensity of this pain is very strong. The attack is repeated many times over a period of 1-2 minutes, after which it passes just as suddenly. At the moment of paroxysm, patients behave in a similar way: they freeze in place, are afraid to make any movement. Despite severe pain, patients cannot scream during an attack, as they fear that the pain will increase. Next, the burning sensation “spreads” over the entire half of the face.
Provocateurs of paroxysm are factors such as a flow of cold air, leaving a warm room into the wind, washing with cool water, and exposure to a razor. A person suffering from a neurological disorder is afraid of adding additional stress to the facial muscles, so he rarely laughs, does not eat hard foods, tries to talk less, and opens his mouth only when necessary. The symptoms do not go away without a trace, and frequent relapses are observed. While the pathogenic influence of the root cause remains, a gradual decrease in the functionality of the trigeminal nerve occurs, which affects the kinetic sensitivity of the skin in the affected area.
If treatment is not started in time, a person’s quality of life decreases significantly, and concomitant diseases appear. Since there is a fear of recurrence of pain on the suffering side of the face, the patient is forced to chew food only on the opposite dentition. This fact leads to a gradual thickening of the gum tissue and muscles on only one side. Due to constant tension and discomfort, depressive syndrome develops and the ability to perform quality work and proper rest deteriorates.
Trigeminal nerve - structure, features and functions
The trigeminal nerve is a pair of the largest nerves connected to the brain, located symmetrically in the craniofacial area on both sides of the face.
The nerve consists of three branches emanating from the nerve ganglion in the temple area - the ophthalmic branch, the maxillary and mandibular, which stretch to the forehead, eyelids, cheeks, nasopharynx, jaw.
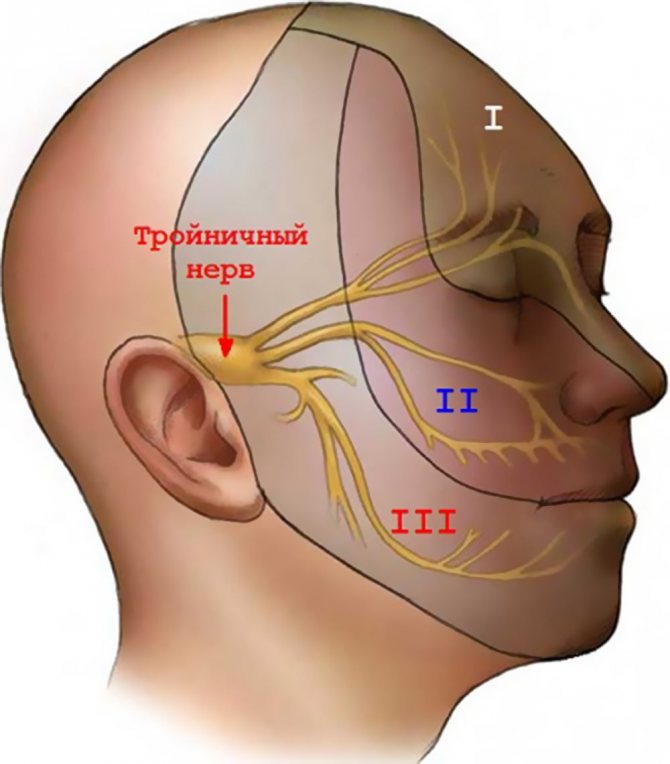
The branches control the motor activity of the muscles in the area of their action (chewing, swallowing), the functioning of the salivary glands, and provide sensitivity to the face, eyelids, tissues of the nasal cavity, mouth, pharynx, dura mater of the brain, soft tissues of the skull, teeth and jaws.
Diagnosis methods
Determining the presence of pathology is not difficult for a specialist - a neurologist during the initial examination. Palpation of the indicated points, causing discomfort and pain, indicates the presence of a disorder. Next, it is necessary to differentiate the anomaly and determine the cause. For this, the following diagnostic methods are used:

- Computer scan of the skull. Aimed at studying bone fibers, deformations of hard tissues, and narrowing of intracranial tracts.
- Magnetic resonance imaging of the head brain. Necessary to exclude developing tumor, cystic objects that can provoke intracerebral nerve compression.
- Magnetic resonance angiography. Looks for a connection between pathology and vascular changes.
Consultation with specialized specialists (dentist, ophthalmologist, otolaryngologist) may be required. This will exclude or confirm the presence of underlying diseases affecting the trigeminal branch.
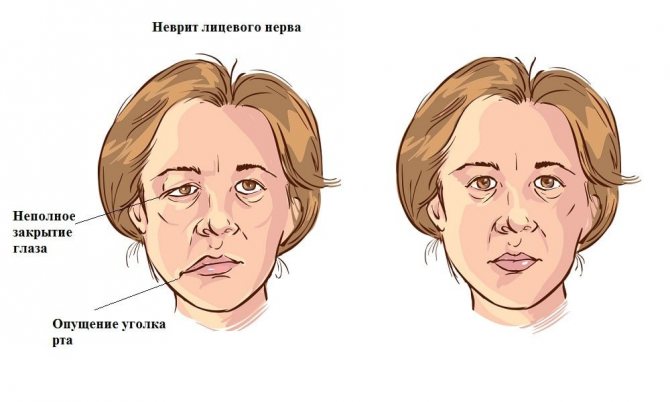
What causes secondary neuropathy?
The following causes of secondary neuritis are identified:
- infection entering the human body (as a rule, a person has previously suffered diseases such as measles or herpes);
- facial injuries;
- hypertension and atherosclerosis caused by disturbances in the functioning of blood vessels located in the spine;
- malignant tumors, the focus of which is at the base of the brain;
- consequences of an anesthetic injection given by a dentist.
To determine the factor that could provoke the appearance of neuritis, the doctor prescribes an MRI procedure for facial nerve neuropathy.
Remedial measures
Therapeutic assistance consists of long-term use of anticonvulsants. The dosage of such drugs is prescribed individually. Reception begins with small doses and gradually increases until the effective amount of the substance is determined. Treatment is carried out for several months, then a gradual reduction in dosage is prescribed.
As an accompanying, symptomatic therapy, antiallergic drugs are prescribed, indicated to reduce swelling. At the same time, antispasmodics are used to relieve pain. For intense attacks, therapeutic blockades with local administration of appropriate solutions are indicated. A good effect is achieved using physiotherapeutic methods.
If growing tissue objects compromising the trigeminal branches are detected, a decision is made to surgically remove the formations. The treatment is carried out by a neurosurgeon.
Forecast and preventive recommendations

The disease does not pose a threat to life, but it greatly affects the patient’s quality of life and well-being. If you seek medical help in a timely manner, the prognosis for recovery is favorable. With instrumental treatment, relapses occur only in 3-15% of cases.
Preventive measures are:
- complete relief from diseases of the jaw area, ear diseases, intracranial sinuses;
- regular monitoring by a neurologist;
- avoidance of negative external factors;
- prevention with anticonvulsants during acute respiratory viral infections and influenza.
In what cases is research carried out?
Damage to the trigeminal nerve due to hypothermia, infection, inflammation, traumatic influences and other damaging factors leads to a disorder of sensitivity and muscle movement in the corresponding areas, and often to acute, unbearably severe pain.
The patient is indicated for MRI diagnostics in the following abnormal conditions:
- the appearance of nagging or sudden intense pain in the temples, jaws, forehead, upper and lower lips on one side of the face (or both);
- pain when moving the muscles of the face and oropharynx - facial expressions, chewing, swallowing;
- pain when touching the skin of the face, head, mouth (applying makeup, shaving, brushing teeth);
- partial or complete loss of sensation (numbness) on one or both sides;
- the occurrence of sensations of heat or cold, goosebumps, tingling;
- paralysis, spasm or convulsive contractions of the muscles of the face, masticatory muscles, difficulty swallowing, eyelid tic, drooping corner of the mouth or eyelid;
- the appearance of asymmetry and swelling on the face;
- hearing disorders, pain inside the ear.
Similar manifestations occur when the trigeminal nerve is damaged, associated with its inflammation (neuritis), damage or spasm of the network of vessels supplying the nerve fiber (neuropathy).
The concept of neuralgia indicates acute pain along the branches. It is often combined with inflammation, but also occurs with mechanical damage - pinching, hypothermia, bruise.
Neuralgia is not characterized by changes in the structure of the affected nerve, motor disturbances and weakening of sensitivity.