Symptoms of endometriosis
- Pain in the lower abdomen. The pain intensifies with the onset of critical days.
- Pain during sexual intercourse.
- Discomfort during bowel movements and urination.
- Bloody discharge between periods.
- Increased intensity of discharge during menstrual periods.
- Infertility.
- General weakness and nausea.
Indications for MRI of the pelvis in women and men
MRI of the pelvis is usually performed as prescribed by the specialist treating the patient. The method is used in gynecology, gastroenterology, urology, oncology if patients have the following symptoms:
congenital malformations of the pelvic organs;- signs of diseases of the digestive system - the final sections of the colon, appendix;
- symptoms of diseases of the genitourinary system - painful urination, colic, blood in the urine;
- bleeding independent of the menstrual cycle, with an unknown cause;
- pain in the lower abdomen, sacrum, thigh;
- injuries, prolapse of the pelvic organs, dysfunction of the pelvic floor muscles;
- suspicion or clarification of the diagnosis of cancer;
- infertility;
- acute conditions requiring surgical intervention.
The pelvic MRI method is used in cases where data from visual examination, palpation, laboratory tests and ultrasound are not enough to make an accurate diagnosis.
The structure of the endometrium
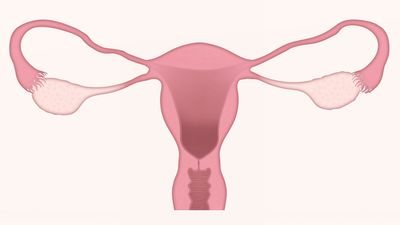
The endometrium is the inner layer of the uterine lining. Its first layer is called basal, the second, which comes out along with the blood during the menstrual period, is called functional. If pregnancy occurs, the fertilized egg attaches to the functional layer of the endometrium and rejection does not occur.
In addition to the vagina, a small amount of menstrual fluid enters the fallopian tubes, ending up in the peritoneal cavity. There, special protective cells destroy secretions.
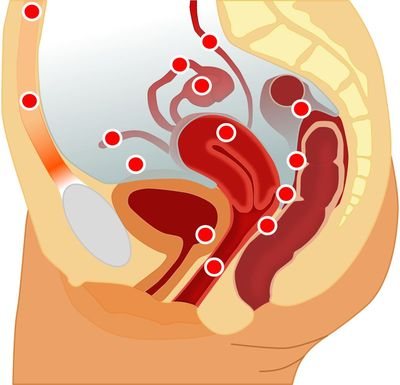
But there are cases when menstrual flow is not completely destroyed. Endometrial cells, once in the pelvic cavity, attach to the internal organs and begin to grow. This is how endometrioid tissue appears. It disrupts a woman's reproductive system.
The most common areas affected by endometrioid tissue are the uterus, ovaries, rectum and bladder.
There are 4 degrees of the disease:
- 1st degree - single superficial lesions.
- Grade 2 - several deeper lesions.
- Grade 3 - many deep foci of endometriosis, small cysts, thin peritoneal adhesions.
- Grade 4 - many deep lesions, large bilateral ovarian cysts, dense adhesions of organs, invasion of the vagina or rectum.
Endometriosis, bladder, MRI
Marina, St. Petersburg
1073 views
July 22, 2019
Good afternoon. 3 years ago, a laparoscopy was performed, during which foci of endometriosis were identified in the uterosacral ligaments, ovaries, and also an endometrial polyp. A polyp and adhesions in the tubes were removed, a biopsy was taken from the uterosacral ligament and the left ovary, the diagnosis of endometriosis was confirmed. Hormone therapy with Lucrin Depot 3 injections was carried out. After therapy there was temporary relief in terms of pain, but gradually the symptoms returned. In the last cycle it suddenly became very bad. In addition to acute pain in the abdomen on the left (but it has been present for a long time), dizziness began, which lasted 2-3 days. I did an MRI of the pelvic organs. According to the doctor, he doesn’t see anything major, but read everything in the conclusion. But the description and conclusion are not very clear to me. I quote: Along the lower contour of the bladder on the left there is an area of decreased MR signal on T2 VI, on T1 VI at this level there is an area of hyperintense MR signal measuring 7.5 * 4 * 4 mm, a focus of endometriosis cannot be excluded. Other: In the uterorectal cavity, an accumulation of fluid is detected, spreading into the mesorectal space, with a total size of up to 59 * 23 * 30 mm. And in conclusion: it is impossible to exclude a focus of endometriosis along the lower wall of the bladder on the left. Accumulation of fluid in the uterovesical cavity with distribution into the mesorectal tissue. Dilatation of the veins of the parametrium." As for the rest, there are minor things: a paraovular cyst on the right (but it was there a long time ago), plus small Nabothian cysts. Everything else seems fine. I personally don’t understand this focus of endometriosis, if it exists: is it in the wall of the bladder or could it just be somewhere nearby? It seems to me that the question is fundamentally important: if the outbreak is just somewhere in the abdominal cavity outside, then one thing, but if it is in the bladder, then some kind of intervention will probably be required. And who should I contact? According to one doctor, cystoscopy is required if bladder endometriosis is suspected. On the other hand, given such an inaccurate conclusion (it cannot be ruled out), I didn’t really want to do such a procedure. Moreover, if the endometriosis is outside the wall (has not sprouted), or just somewhere nearby, then cystoscopy will not show anything. I would like to hear opinions on what is better to do and whether to do something? Laparoscopy, which will allow removal at the same time if the lesion really exists, or cystoscopy, which may not show anything at all, or can simply carry out hormonal therapy again in the hope that everything will die off on its own, or do nothing at all, wait and observe the symptoms? Among other symptoms, but for a very long time: I have to go to the toilet often, I cannot tolerate even a slight fullness of the bladder, but according to general tests, they have never found any anomalies: such as blood in the urine or on ultrasound and the same MRI anomalies of the kidneys.
The question is closed
What factors can trigger the disease?
- infectious and inflammatory processes of the reproductive system organs
- surgical interventions in the uterine cavity
- difficult childbirth
- anemia, decreased immunity
- disturbance of hormonal balance, endocrine system
- irregular menstrual cycle
- long-term contraception with intrauterine devices
- presence of malignant tumors
- consumption of alcohol, as well as substances containing nicotine, caffeine
Types of endometriosis:
- Endometriosis of the uterus. The disease is accompanied by heavy discharge during menstruation, uterine bleeding with a subsequent risk of developing anemia and severe pain. If a pathology is detected, treatment with hormonal drugs is prescribed.
- Endometriosis of the cervix. Bloody discharge occurs in the middle of the cycle, increased pain during menstruation. When the diagnosis is confirmed, the doctor prescribes treatment with hormonal drugs and cauterization of foci of endometrial growth.
- Ovarian endometriosis. The disease is characterized by sharp cutting pain in the lower abdomen, especially during or after sexual intercourse. Cysts appear that interfere with the reproductive process - the release of the egg from the follicle.
- Vaginal endometriosis. It can move from the body of the uterus to the walls of the vagina, which is especially likely if there are wounds and inflammatory processes on the mucous membrane. It manifests itself as spotting and pain during sexual intercourse.
- Enzhometriosis of the abdominal cavity. The causes of the disease may be the entry of endometrial cells into the peritoneum during retrograde menstruation, or in the case of disorders that developed during the period of intrauterine development of the fetus. Stitching pain appears during menstruation or sexual intercourse.
Diagnosis of uterine endometriosis

If you notice alarming symptoms of endometriosis, you should consult a gynecologist. It is possible to make a diagnosis only after collecting anamnestic data and a comprehensive examination of the patient.
- Examination in a gynecological chair. During the examination, the doctor gets an idea of the current state of the uterus, palpates the nodes and tuberosity.
- Ultrasound of all pelvic organs allows you to determine the localization of foci of endometriosis.
- Magnetic resonance imaging.
- Laparoscopy. The procedure is performed through a puncture in the lower abdomen. A special device - a laparoscope - gives a clear picture of the condition of the organs of the reproductive system and is capable of cauterizing the affected tissues.
- Hysterosalpingography.
- Colposcopy. Examination of the vagina and cervix using a special device - a colposcope.
Diagnostic laparoscopy and hysteroscopy involve a biopsy of material from internal organs affected by endometriosis. The resulting tissue sample is sent for histological examination. This analysis is carried out to determine malignant forms of formations.
Preparation and progress of the procedure
In order to clearly see the foci of endometriosis and the amount of overgrown tissue, it is necessary to take into account the day of the menstrual cycle.
The procedure is prescribed between days 6 and 12 of the cycle - at this time, tissue inclusions will be most accurately visible.
On the day of the procedure you need to prepare:
- give an enema if you have problems with bowel movements;
- take medications for flatulence and cramps if necessary;
- remove jewelry, watches, leave a mobile phone outside the diagnostic room.

The intestines need to be emptied so that the tomograph detects endometrial inclusions, especially if the gynecologist suspects the appearance of foci of endometriosis in the intestines.
The patient is placed on a special couch, which rises and slides into the device. During the procedure, the sounds of its operation are heard - these are vibrations of the coils.
The rest of the time you need to lie still so that the resulting image is clear.
The procedure lasts 15-45 minutes, depending on the tomograph. The doctor maintains contact with the patient using a sound system. The patient holds the communication button. If you get scared, you can press this button and the study will stop.
It is better to lie inside the tomograph with your eyes closed, relaxed. The calmer and deeper the patient breathes, the better the quality of the recording.
Being in the narrow space of the device is safe, but can be disturbing even for those who do not suffer from claustrophobia.
How to treat endometriosis during pregnancy?
If a woman's genitals are susceptible to the development of endometriosis, this does not mean that it is impossible to get pregnant. Often pregnancy has a beneficial effect on the course of the disease.
While carrying a baby, a state of prolonged anovulation occurs, there is no menstruation, and the body is under the influence of progesterone for 9 months. This promotes regression of the disease.
Endometriosis does not directly affect the child, so there is no need to worry about the baby’s health. But you need to keep in mind that the baby in the womb may not receive enough nutrients and oxygen due to a malfunction of the placenta.
How to treat endometriosis?

There are several types of treatment:
- therapeutic – using medications
- surgical organ-preserving – involves removing foci of endometriosis while preserving organs
- surgical radical with removal of the uterus and ovaries
- combined
The choice of treatment is made by a doctor and depends on many factors: the patient’s age, desire and ability to preserve reproductive function, the severity of the disease and concomitant pathologies.
Treatment of endometriosis in women over 40 years of age involves an integrated approach, using drugs from different groups and vitamin complexes for reduced immunity. Before the onset of menopause, the hormonal status and immune defense of the female body change. The menstrual cycle is disrupted, an increase in estrogen production contributes to pathological growth of the inner layer of the uterus
Drug treatment of endometriosis is indicated for women at a young age who have an asymptomatic course of the disease. Therapy includes taking hormonal drugs, as well as anti-inflammatory and symptomatic therapy. Side effects when taking medications may include decreased libido and weight gain.
In addition to the main treatment, anti-spasm and sedative medications may be prescribed for auxiliary therapy.
Surgical treatment of pathology involves laparoscopy (microsurgical intervention), and less commonly, in severe cases, laparotomy (dissection of the abdominal wall) is performed. Surgical treatment is indicated for:
- dysfunction of neighboring organs
- ineffectiveness of conservative therapy
- probable ovarian tumor
- in the presence of an endometrioid ovarian cyst
Surgical intervention is carried out using electrocoagulation or laser - foci of endometriosis are cauterized or removed. Typically, surgical treatment is combined with medication. First, the patient must take hormonal medications for 3-6 months, then the endometriosis is removed.
The rehabilitation period in most cases is favorable: reproductive function is restored, pain during menstruation is significantly reduced. After treatment, constant monitoring by a doctor, ultrasound monitoring (once every 3 months), and monitoring of the CA-125 marker in the blood are recommended.
Uterine endometriosis is a recurrent chronic disease. Relapses after treatment occur in 20% of cases. With combined treatment, a longer lasting effect is observed, but exacerbations are still inevitable.
Why does endometriosis develop and its classification?
Despite the many studies conducted to identify the reliable causes of the development of endometriosis, a consensus in the scientific community has not yet been achieved. There are many genetic, immune and other less common theories. The following is considered the most reliable.
There are two main forms of endometriosis, different in their causes and manifestations:
- Genital. Affects the internal genital organs: uterus, fallopian tubes, ovaries, vagina. Due to the presence of a chronic inflammatory process (endometritis of any nature), abortion, injury, the presence of an intrauterine device, or spontaneously, endometrial cells begin to grow into the muscular layer of the uterus. There are also two subspecies:
- External genital. It affects only the ovaries and peritoneum of the small pelvis.
- Internal genital (adenomyosis or endometriosis of the uterus). Grows into the muscle layer, leading to an increase in the body of the uterus. Often combined with fibroids.
There are known cases of a combination of genital and extragenital endometriosis.
There are 4 stages of development of this pathology, based on the prevalence and depth of the lesions:
- Stage I - Lesions of small size, superficial (affect only the uterine mucosa) - minimal endometriosis.
- Stage II - Some lesions penetrate the muscular layer - mild endometriosis.
- Stage III - deep, transmural (through the entire wall of the uterus) foci of endometriosis appear. Small endometriotic ovarian cysts develop.
- Stage IV - there are many deep foci, cysts reach significant sizes. Foci of endometriosis grow into neighboring organs (vagina, rectum, bladder), and adhesions develop in the pelvis - severe endometriosis.