The need to examine these organs for the presence of tumors and metastases is primarily explained by their structure. The thing is that it is the lymph nodes that are the first to be affected when metastases occur in the body, and their identification plays a very important prognostic role. Thanks to the examination of lymph nodes, it is possible to judge the stage of the disease, select treatment tactics, and also assess the volume of necessary surgical intervention.
How is an ultrasound of lymph nodes done?
As a rule, no special preparation is required for ultrasound examination of lymph nodes. The only exception is ultrasound of the retroperitoneal lymph nodes. In this case, for two to three days you should follow a diet without foods that cause gas formation. The day before the examination, dinner should be light.
A gel is applied to the area of the body under study (preliminarily freed from clothing) and a sensor is pressed against it, with the help of which the ultrasonic waves reflected by the organs are transmitted to the screen in the form of an image. The procedure is completely painless and lasts on average 10-15 minutes.
Ultrasound of axillary lymph nodes
Ultrasound of the axillary lymph nodes is prescribed for pathologies or suspected pathologies in the area of the mammary glands and lymph nodes in the armpits. Also after mastectomy or other surgical interventions. This type of examination is carried out as follows: the patient undresses to the waist, taking either a lying or sitting position. Then, using a special sensor, the doctor performs all the necessary manipulations to study the structure of the lymph nodes.
Ultrasound of submandibular lymph nodes
If leukemia or deformed jaw bone tissue is suspected, the doctor may prescribe an ultrasound of the submandibular lymph nodes. The procedure is carried out like an ultrasound of any other organs: the area under study is exposed, lubricated with gel, and examined using a sensor.
Ultrasound of lymph nodes in the groin area
Indications for prescribing ultrasound of lymph nodes in the groin area are diseases of the genitourinary system
, viral, bacterial, fungal diseases. The procedure is carried out the same way as always. The patient only needs to undress from the waist down and lie down on the couch.
Are additional tests needed?
The accuracy of the diagnosis depends on the completeness of the information received about the patient’s condition. In addition to ultrasound, the doctor must prescribe additional tests that will complement the clinical picture of the disease. Current research methods:
- general blood analysis;
- blood chemistry;
- tests for tuberculosis;
- blood test for HIV/AIDS;
- X-ray;
- MRI;
- CT scan.
The functionality of the tomograph in our clinic allows us to most accurately perform ultrasound, which eliminates the need for many additional tests.
Decoding the results

The results are given to the patient after the procedure. The protocol must reflect the following information about the lymph nodes:
- dimensions, length/width ratio, shape;
- structure of the lymph node, the presence of differentiation into the cortex and medulla;
- extent of lesion/enlargement;
- number of vessels;
- density;
- borders and contours.
Normally, the size of the lymph nodes should not be enlarged, the diameter is about 10 mm. The norm also includes smooth contours, a uniform structure, the absence of growths and any formations.
Survey methodology
The diagnostic room has a specialist workplace, and a couch for the patient is required.
Examinations of the cervical spine are performed while sitting. The area being diagnosed is exposed. The doctor applies a gel to the area, which promotes soft gliding and effective passage of ultrasound pulses towards the tissues and back. The information received is displayed on the monitor and recorded in the protocol.
An ultrasound of the lymph nodes, which shows the slightest deviation from the norm, can diagnose the disease at an early stage and prevent death in the future.
The procedure lasts from 10 minutes to half an hour, depending on the complexity of the placement of the nodes and the thoroughness of the diagnosis.
The diagnostician enters the results obtained on a form and gives them to the patient. A specialized doctor deciphers the data and makes a diagnosis.
What pathologies can be detected?
Ultrasound of lymph nodes
, a variety of pathologies can be detected. For example, inflammation of the lymph node, its benign enlargement.
Thanks to this type of examination, such as ultrasound of the lymph nodes, it is possible to detect or confirm cancer, metastases, and suspect sexually transmitted diseases (for example, AIDS or syphilis).
Is lymph node cancer visible on ultrasound?
In addition to the above, ultrasound also shows so-called lymph node cancer. This occurs when metastases enter the lymph nodes and lymphoma. First of all, it manifests itself in a change in shape. The more pronounced the roundness, the more likely the presence of a malignant formation. Also, with this disease, the structure of the lymph node changes; the contours may be unclear or completely blurred.
Inaccuracies and preliminary diagnoses based on ultrasound diagnostics
Correct diagnosis and interpretation of ultrasound results determines the further outcome of treatment. Conducting ultrasound examinations by inexperienced specialists or under conditions of turmoil and nervous tension in public health facilities shows low effectiveness. In stressful environments, human error may occur more often than usual.
For an error-free diagnosis, it is recommended to contact a private diagnostic and treatment institution, the Women’s and Men’s Health Clinic, which offers ultrasound of the neck lymph nodes at a low price. The center does not create queues outside the office door, accepts patients by appointment, and pays due attention to patients.
Ultrasound examination of lymph nodes

Ultrasound scanner HS60
Professional diagnostic tools.
Assessment of tissue elasticity, advanced 3D/4D/5D scanning capabilities, BI-RADS classifier, options for expert cardiological studies.
Assessing the state of regional lymphatic drainage zones when examining cancer patients is crucial in determining treatment tactics and prognosis of the course of the disease. Knowledge of the lymphatic drainage pathways allows for a targeted search for metastatically changed lymph nodes in patients with malignant neoplasms. Clarifying the location and number of identified altered lymph nodes makes it possible to clarify the stage of the tumor process.
Identification of lymph nodes during physical examination is not always possible. Thus, according to R. Chandawarkar and S. Shinde [1], J. Verbanck et al. [2], the sensitivity of palpation in identifying lymph nodes ranges from 50 to 88%. Deep-lying lymph nodes, for example, retromammary, intrapectoral, etc., are not available for clinical assessment by palpation. One of the leading methods for detecting pathology of lymph nodes is ultrasound examination (US). The accuracy of ultrasound in identifying lymph nodes varies; it largely depends on the location of the lymph nodes, the quality of the equipment, and the experience of the researcher. The specificity of ultrasound in the detection and differential diagnosis of lymph node involvement ranges from 30 to 100% [3-6]. The number of works devoted to ultrasound diagnosis of metastatic lesions of superficial lymph nodes is increasing [7, 8].
Peripheral lymph nodes are examined with linear sensors with an operating frequency of 5-12 MHz; linear and convex sensors with an operating frequency of 3-5 MHz can be used to examine large peripheral conglomerates.
Regional studies are often carried out on the affected side, sometimes on the contralateral side, and in cases of lymphogranulomatosis, non-Hodgkin's lymphomas, leukemia, etc. Ultrasound should be performed taking into account the possible damage to different groups of lymph nodes.
When performing an ultrasound, the location of the lymph nodes, their number, shape, size and structure should be determined.
Normally, lymph nodes are bean-shaped, oval or ribbon-shaped formations and are located in groups, often several nodes.
The size of the lymph nodes depends on the age of the subject, the characteristics of the constitution, etc. In clinically healthy people, lymph nodes can be found, the length of which reaches 3.5 cm. There is a difference in the size and shape of the lymph nodes of different regional groups and lymph nodes located in different areas in the same individual.
The shape of the lymph nodes largely depends on their topographic-anatomical relationship with adjacent organs; usually it is somewhat oblong and flattened, slightly convex on one side and with a small depression on the other, reminiscent of a bean. Sometimes the shape of a lymph node can be round. In the elderly and senile, ribbon-shaped forms of lymph nodes are often found, which can be considered as the result of the fusion of smaller nodes. In areas limited by fascia (for example, in the occipital region), the nodes are more elongated in length than those located in loose tissue (for example, axillary) (Fig. 1, 2).
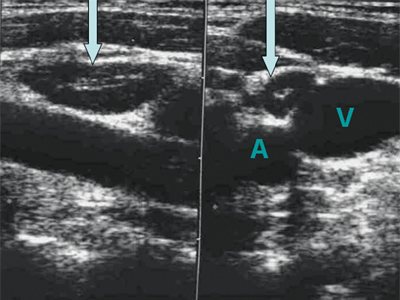
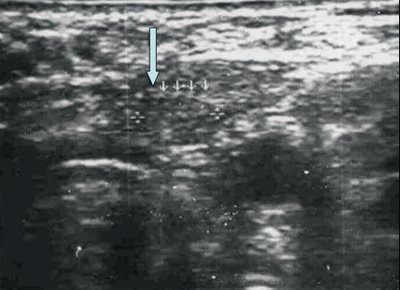
Rice. 1.
Lymph node in the upper third of the neck along the vascular bundle (longitudinal and cross sections). A - left common carotid artery; V - left jugular vein.
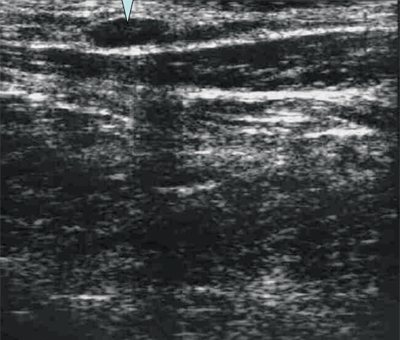
Rice. 2.
Oval superficial lymph node - ln. occipitalis superficialis.
The echogenicity of the lymph nodes is assessed in relation to the surrounding tissues (usually fiber) and is described as high, medium and low (hyper- or hypoechoic, iso- or anechoic lymph nodes) (Fig. 3, 4).
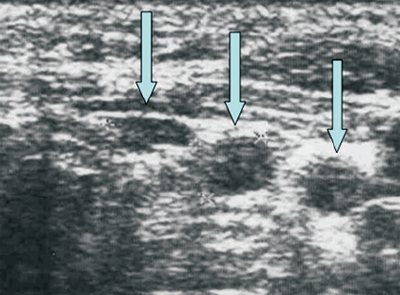
Rice. 3.
Metastases to the lymph nodes (LN) of the neck (Ln. Pretrachealis and Lnn. laterotracheales sinistri). Hypoechoic round homogeneous lymph nodes.
Rice. 4.
Condition after thyroidectomy. Isoechogenic pretracheal lymph node (left).
The lymph node is covered with a connective tissue capsule, which is represented by a hyperechoic rim with smooth contours (a wavy contour is often found, depending on the structure of the capsule). The capsule, surrounding the lymph node on all sides, usually thickens in the area of the gate of the node, and connective tissue partitions - trabeculae - are directed from its inner surface deep into the node (Fig. 5).
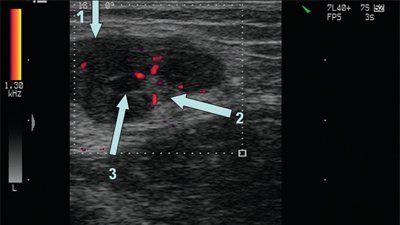
Rice. 5.
Hyperplastic inguinal lymph node. 1 - capsule; 2 - gate; 3 - trabeculae.
The number of gates in the lymph nodes varies. Thus, in the deep cervical nodes, as a rule, there are 2 gates, in the central axillary nodes - 1-2, in the superficial inguinal nodes - 1. In the gates of the lymph nodes, one artery and two veins are most often located. The artery enters the lymph node in the hilum area, passes in trabeculae, branches (fan-shaped) towards the capsule, forming circumflex branches along the inner surface of the capsule. Veins emerge from the node through the gate. Detection of vessels in the node depends on the capabilities of the device; normally, it is most often possible to see vessels in the gate of the node.
The parenchyma of the lymph node is divided into the cortex, located closer to the capsule, and the medullary (brain) part, which occupies the central sections of the node, located closer to the gate of the organ. The ratio of cortex and medulla varies depending on the location of the lymph nodes.
The cortex is represented by a weakly hypoechoic (almost isoechoic) homogeneous rim. The central sections (trabeculae, perihilar thickening, fatty inclusions, partly the medulla) are represented by a hyperechoic structure, the hilum is often represented by a homogeneous hypoechoic, mostly irregular (triangular) structure.
The structure of the lymph nodes changes depending on the stages of their location. Thus, when assessing the structure of the lymph nodes of the neck located next to the organ, it is clear that the lymph nodes closest to the organ (not constantly present) are relatively small in size, round or spindle-shaped, and the cortex is less pronounced in them. In lymph nodes located further from the organ, the cortex is better developed.
The relationship of the lymph node with surrounding tissues refers to the relative position of the node and surrounding tissues: lack of connection or preservation of the capsule of the lymph node and the presence of a layer of fiber (or connective tissue) between the lymph node and other structures; contact or adhesion to an organ (vessel, etc.) without violating its integrity; involvement in the tumor process.
In elderly people, reduction and sclerosis of the lymph nodes are detected, some of them grow together (in the elderly, large lymph nodes are more often detected). In this case, large areas of the node are replaced by adipose tissue. Fatty infiltration in old age destroys the capsule of the node. Lymph nodes overgrown with fat (usually peripheral) look like round and oval structures with a hyperechoic heterogeneous (sometimes reticular) central part and a relatively thin hypoechoic rim. The capsule of the node may be visible in fragments.
The localization of the lymph node is described in relation to the anatomical region, the neurovascular bundle, or the organ next to which the identified lymph node is located (in the middle third of the neck, outward from the neurovascular bundle).
For ease of diagnosis, banal (nonspecific) lymphadenitis is differentiated as follows:
- According to the course of the disease
: 1) acute; 2) subacute; 3) chronic (Fig. 6, 7). - By localization
: 1) isolated; 2) regional (group); 3) common; 4) generalized.

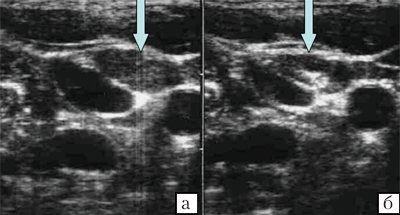
Rice. 6.
Acute lymphadenitis (lymph node in the middle third of the neck to the left outward from the vascular bundle in a patient with jugular vein thrombosis). The capsule is not clearly differentiated.
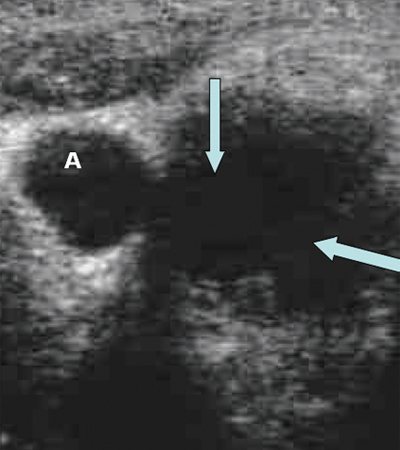
Rice. 7.
Acute lymphadenitis, destruction of the lymph node (shown by arrows). A - left common carotid artery.
Reactive changes that occur in response to various pathological processes in the body (inflammatory process, vaccination, etc.) contribute to an enlargement of the lymph node, tension of its capsule, increased vascular pattern, expansion of the cortical and pericortical zones, swelling and disintegration of the capsule, expansion of the sinuses, In the lymph node, single anechoic “cystic” structures may occur, and abscess formation may subsequently occur. It should be taken into account that changes in the lymph nodes located next to the tumor can be expressed in a nonspecific inflammatory reaction (Fig. 8).
Rice. 8.
Hyperplastic lymph nodes in a patient with psoriasis.
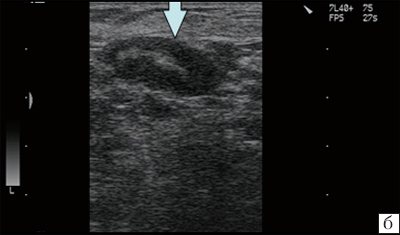
a, b)
Enlarged lymph node, thickened hypoechoic peripheral part, thickened capsule (shown by arrow).
Hyperplastic lymph nodes are often oval in shape, hyperechoic echostructure, with a thin hypoechoic rim occupying about 1/3 of the node; the size of the lymph nodes in the groin areas is usually no more than 3.5x1.5 cm, in other areas - 2.5x1 cm. The ratio of the length to the thickness of the lymph nodes with hyperplasia does not exceed 1:2. The contours of hyperplastic nodes are clear and even. In reactive processes, the node architecture is preserved. Hypoechoic nodes, oval or round in shape, with smooth, clear contours, small in size, sometimes with a hyperechoic center occupying less than 2/3 of the node, can be either hyperplastic or metastatic.
According to M. Choi et al. [9], the vessels in the inflamed lymph node are dilated in comparison with the vessels of the metastatic lymph node, which, on the contrary, can be compressed by tumor cells.
In normal and reactively changed lymph nodes due to inflammation, visible vessels are often located in the area of the hilum of the lymph nodes or are not detected at all. In a large hyperplastic lymph node, the vascular pattern in the peripheral parts is ordered, vessels (arteries) are defined along the capsule and radially from the hilum to the periphery.
With hyperplasia, in the case of a positive effect of treatment, the lymph nodes become less contrasting and their size decreases. In chronic lymphadenitis, thickening of the capsule and its adhesion to surrounding tissues are often observed.
Metastatic lesions with large size nodes, their irregular shape, uneven or unclear contours can be confidently spoken of in the presence of anechoic areas in the nodes and the identification of conglomerates of lymph nodes (Fig. 9, 10).
Rice. 9.
Lymph nodes of the neck (1 year after surgery for thyroid cancer).
A)
Metastasis to a lymph node.
b)
Hyperplastic lymph node (the central hyperechoic structure is preserved).
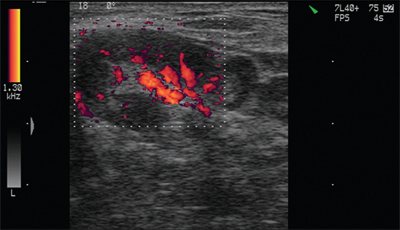
Rice. 10.
Vascular pattern of a peripheral hyperplastic lymph node (subacute lymphadenitis).
With metastatic damage to the lymph node, a change in its shape, size, echogenicity and structure occurs. The described phenomenon underlies the use of ultrasound for the diagnosis of metastatic lesions of the lymph nodes.
P. Vassallo et al. (1993) showed that tumor infiltration leads to a change in the shape of the lymph node (the ratio of the transverse and longitudinal dimensions or the long and short axes of the lymph node is less than 1.5): it becomes round, hypo- or anechoic, and expansion of the cortical layer is visible. Thus, the closer the shape of the lymph node is to round, the greater the likelihood of tumor damage to the lymph node. When infiltrating and growing into surrounding tissues, the capsule of the node is not clearly defined, the contour becomes blurred.
It is known that with metastatic damage to the lymph nodes, the fluid content in them increases. When performing ultrasound, erasure of the lymph node pattern is noted already at the initial stage (replacement with tumor cells) [9-11]. The capsule of the lymph node differentiates, but when it grows beyond the capsule, the contour of the node becomes blurred. With infiltration of the capsule, further (germination of surrounding tissues) spread beyond the lymph node and fusion of several nodes, the formation of conglomerates is observed.
Thus, the image of the structure of metastatically affected lymph nodes can be: hypoechoic up to anechoic, hyperechoic heterogeneous (polymorphic heterogeneous) due to the alternation of hyper- and hypoechoic areas and with the presence of local hypoechoic areas against the background of an unchanged or hyperplastic structure of the lymph nodes.
In case of malignant processes in the lymph nodes, the hyperechoic central part is most often absent or its thinning is noted, which corresponds to diffuse or total replacement of the central parts with tumor tissue. In some cases, with metastatic damage to only the central part of the lymph node, it may appear unchanged, since the image of the portal is imitated by tumor tissue (more common in well-differentiated squamous cell carcinoma or other forms of cancer that are accompanied by coagulative necrosis, in the case of ischemic degeneration). Sometimes the lymph node can be observed as a completely hyperechoic formation. Although the latter is more typical for fatty infiltration, in these cases the tumor genesis of the changes cannot be completely excluded.
The structure of the lymph node when replaced by tumor tissue is often heterogeneous or hypoechoic. There are anechoic lymph nodes (for example, with melanoma) or iso- and hyperechoic (with papillary cancer). Sometimes hyperechoic inclusions (calcifications) can be visualized in a metastatic lymph node, and intranodal necrosis with a characteristic heterogeneous ultrasound picture can also be observed.
In metastatic lymph nodes, there is a diffuse increase in vascularization with a wide range of velocities and an atypical vascular pattern (chaotically located vessels with the presence of arteriovenous shunts). According to spectral analysis, there are low values of the resistance index with a simultaneous high diastolic component.
If there are several (groups) of enlarged lymph nodes located nearby, their shape may be irregular or polycyclic (when they grow beyond the capsule), and with lymphogranulomatosis, when enlarged lymph nodes are located nearby, but there is no germination of the capsule, the group of lymph nodes looks very characteristic - like “packs” of lymph nodes.
Extracapsular growth of metastases in the lymph nodes often leads to the union of several affected lymph nodes into a shapeless conglomerate and the involvement of surrounding tissues in the tumor process. A sign of infiltrative growth beyond the capsule of the node is the vagueness of its contours. The involvement of adjacent organs and structures in the tumor conglomerate should also be determined and the nature of this involvement should be described.
According to T. Arita et al. (1993), ultrasound is also effective in assessing changes in lymph nodes over time.
When assessing the condition of the lymph nodes, it should be remembered that the presence of an altered lymph node may indicate both hyperplasia of the node and its metastatic lesion, however, with multiple tumor lesions, metastases may belong to different tumors. So, N.I. Bogdanskaya (1978) described a case of simultaneous damage to the cervical lymph node by metastases of thyroid cancer and lymphosarcoma (Fig. 11).
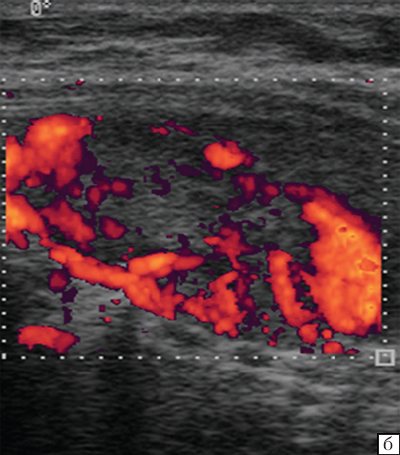
Rice. eleven.
LGM. Blood flow in the lymph nodes of the neck.
A fairly characteristic ultrasound picture of the lymph nodes is observed in lymphogranulomatosis. In most cases, several enlarged lymph nodes (one or more groups of lymph nodes) are visible. The node has an oval or round shape, a clearly visible capsule, a homogeneous, often weakly hypoechoic structure. A group of enlarged lymph nodes (“pack”) is represented by clearly demarcated lymph nodes that do not grow into the capsule and do not merge with each other (as in a metastatic lesion, in the form of a conglomerate) and can be localized in any one area (for example, supraclavicular on the right or left) or in several areas (enlarged lymph nodes of the mediastinum, supraclavicular and in the lower third of the neck on one or both sides, etc.).
Literature
- 1. Chandawarkar RY, Shinde SR Preoperative diagnosis of carcinoma of the breast: Is a “cost-cutter” algorithm tenable // J. Surg. Oncol. 1997. N2. R. 153-158.
- 2. Verbanck J., Vandewiele I., De Winter H. et al. Value of axillary ultrasonography and sonographically guided puncture of axillary nodes: a prospective study in 144 consecutive patients // J. Clin. Ultrasound. 1997. N2. R. 53-56.
- 3. Carl M., Stroebel W., Rassner G., Garbe C. The difficulty of ultrasound diagnosis of lymph node metastases of malignant melanoma in protracted tumor growth //Hautarzt. 1997. N48 (4). R. 234-239.
- 4. Mobbs LM, Jannicky EAS, Weaver DL, Harvey SC The Accuracy of Sonography in Detecting Abnormal Axillary Lymph Nodes When Breast Cancer Is Present // J Diagnostic Medical Sonography. 2005. V. 21. N4. R. 297-303.
- 5. Willam C, Maurer J, Steinkamp HJ et al. Differential diagnosis of cervical lymph node enlargements: ultrasound and histomorphology of reactive lymph nodes // Bildgebung. 1996. N63 (2). R. 113-119.
- 6. Chissov V.I., Trofimova E.Yu. Ultrasound examination of lymph nodes in oncology / Practical guide. Publishing house Strom. M., 2003; 109 p.
- 7. Eggermont AM Reducing the Need for Sentinel Node Procedures by Ultrasound Examination of Regional Lymph Nodes // Annals of Surgical Oncology. 2005. N12. R. 3-5.
- 8. Esen G. Ultrasound of superficial lymph nodes // Eur J Radiology. 2006. V. 58. Issue 3. P. 345-359.
- 9. Choi MY, Lee JW, Jang KJ Distinction between benign and malignant causes of cervical, axillary, and inguinal lymphadenopathy: value of Doppler spectral waveform analysis // AJR. 1999. N4. R. 981-984.
- 10. Bjurstam NG The radiographic appearance of normal and metastatic axillary lymph nodes // Recent. Results. Cancer Res. 1984. N9. R. 49-54.
- 11. Chan JM, Shin LK, Jeffrey RB Ultrasonography of Abnormal Neck Lymph Nodes // Ultrasound Quarterly. 2007. N23 (1). R. 47-54.
Ultrasound scanner HS60
Professional diagnostic tools.
Assessment of tissue elasticity, advanced 3D/4D/5D scanning capabilities, BI-RADS classifier, options for expert cardiological studies.
When is it necessary to do an ultrasound of the abdominal cavity and retroperitoneal space?
An ultrasound of the abdominal organs and retroperitoneal space can be done on the direction of a doctor or on the patient’s own initiative when he has pain in the abdomen and lower back, bloating and an increase in volume. This procedure is often used as a screening method when it is necessary to determine:
- etiology of unclear pain;
- causes of abdominal cramps;
- causes of bloating and indigestion;
- consequences of traumatic injuries;
- problems with the kidneys and urinary system;
- chronic diseases of the liver, spleen, gall bladder, kidneys, pancreas;
- causes of hormonal imbalances in the adrenal glands.
Ultrasound of the abdominal cavity and retroperitoneal space - which organs are checked
Basic ultrasound of the abdominal cavity and retroperitoneum consists of two protocols: ultrasound of the abdominal cavity and ultrasound of the retroperitoneum and includes scanning of the following organs:
- liver;
- spleen;
- gallbladder;
- pancreas;
- bile ducts;
- kidneys;
- adrenal glands;
- upper part of the ureters;
- retroperitoneal lymph nodes;
- soft tissues of the abdomen.
Ultrasound of the abdominal cavity and retroperitoneal space poorly visualizes the intestine.
To examine it, you should use either colonoscopy, gastroscopy, or virtual CT colonography or MRI of the intestine. The stomach can also be assessed using ultrasound diagnostics as part of a separate examination - gastric ultrasound or endosonography. If a comprehensive program of examination of the obstructive system and urinary system is necessary, an ultrasound of the abdominal cavity, kidneys and bladder should be performed. It should be said that ultrasound of the abdominal cavity and ultrasound of the abdominal cavity and retroperitoneal space are not the same study. During an OBP ultrasound, the kidneys, adrenal glands and the upper part of the ureters will be left out of the scan.