The term “isoechoic formation” refers to a section of tissue or organ of the human body, which, during ultrasound examination, has a density similar to other tissues. This inclusion is detected only by the presence of symptoms of compression of nearby tissues or the presence of a capsule. Most often, this indicates the presence of a neoplasm, both benign and malignant.
During an ultrasound, two types of structures are revealed: hyperechoic (dense, with a high ability to reflect ultrasound, so they stand out in a light color on the screen) and hypoechoic (with a reduced density, also reflect ultrasound, but are highlighted in a dark color on the screen). Accordingly, areas that are not illuminated are isoechoic formations. Their density prevents ultrasonic waves from passing through them.
- The main symptoms of isoechoic formation
- Types of hypoechoic formations
- Effective treatments
- Isoechogenic formations of the ovaries
- Isoechogenic nodule in the thyroid gland
- Isoechogenic changes in the structure of the uterus
- Isoechogenic formation in the liver
- Isoechogenic formation in the mammary gland
- Carcinoma
The main symptoms of isoechoic formation
It is worth considering the fact that the neoplasm can have a malignant course, therefore, as it grows, symptoms such as compression of the esophagus, trachea, vocal cords, etc. may occur. Accordingly, the larger the node, the brighter the symptoms.
If you have such a pathology, you should pay attention to the following symptoms:
- Any difficulty breathing, symptoms may appear when changing body position.
- Hoarseness of voice.
- Difficulty swallowing.
- Feeling of a lump in the throat.
- The appearance of irregularities in the neck or a uniform increase in its size.
Any manifestations of the disease depend entirely on the location of the node and its size. If the formation is located on the outside of the organs, then there will be no symptoms of compression of the vessels, trachea and esophagus. Similar formations can be detected by palpation and ultrasound of the throat and larynx.
Completely different symptoms are observed when the node is located inside the gland. Also, the manifestation of other symptoms is possible when the organ begins to produce excessive amounts of hormones. As a rule, all signs of the development of thyrotoxicosis are noted:
- tachycardia;
- fast fatiguability;
- excessive sweating;
- significant weight loss;
- sudden change of mood;
- tremor of the upper extremities.
Isoechogenic formation - thyroid gland, liver, kidneys, uterus and mammary gland
The ultrasound method is based on the ability of tissue to absorb and reflect ultrasound radiation. Fabrics of different densities cope with this work differently.
Thanks to this, a heterogeneous pattern is obtained on the monitor screen, by studying which pathologies such as neoplasms, internal injuries, hematomas, etc. can be determined.
Normally, ultrasound can distinguish between 2 types of structures:
- Hyperechoic - when the area under study has a dense structure and has the highest ability to reflect ultrasound. On the screen it has an intensely light color.
- Hypoechoic - a tissue structure of low density and with a high ability to absorb ultrasound radiation, due to which it has a dark color on the screen.
- Isoechogenic structures deserve special attention, since these formations have the same acoustic ability as other surrounding tissues and are therefore difficult to detect on ultrasound.
Visual color interpretation of the echogenicity of the area under study in ultrasound diagnostics.
What it is
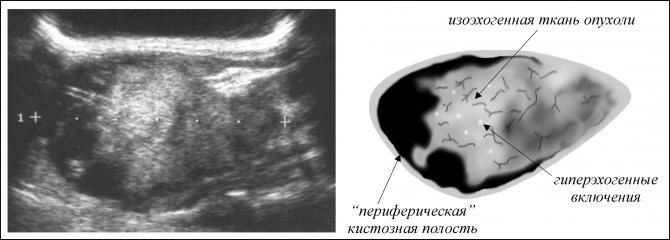
An isoechoic formation means an area that has exactly the same density as the entire surrounding tissue of the organ. This formation can be detected only if there is a shell (see photo) - a capsule, or if there are signs of compression of this segment.
Ultrasound image of an isoechoic formation.
The presence of an isoechoic formation indicates the development of a neoplasm, which may not manifest itself clinically and may not bother the patient. Basically, this pathology can be detected by chance during a routine examination or when diagnosing other problems.
Isoechogenic formation in the thyroid gland
Isoechogenic formations of the thyroid gland (isoechoic node) are called neoplasms similar in density to the rest of the parenchyma of the organ.
On ultrasound, an isoechoic thyroid nodule can be visualized by the presence of boundaries. The borders appear around the node as a rim (see photo above).
These formations are discovered completely by accident, since the development of these elements can occur in a hidden form, without manifesting itself at all.
It must be said that the echogenicity of the node can be different - increased, average, decreased and sharply decreased.
Echogenicity of thyroid nodules on ultrasound images.
- If the echogenicity of the neoplasm corresponds to the echogenicity of the unchanged gland tissue, then it is considered isoechoic.
- If the echogenicity is reduced in comparison with the rest of the unchanged gland tissue, then it is considered hypoechoic.
- When echogenicity increases in comparison with the rest of the unchanged parenchyma of the gland, then it is considered a hyperechoic node.
Hypoechoic rim (halo) can occur with both benign and malignant neoplasms. Presumably, the halo is a zone that does not reflect ultrasound waves, at the border between the thyroid parenchyma and the node.
Halo bezel is described as - thin, fuzzy, wide, uneven.
Node boundaries—represented in the description as two groups: clear and fuzzy. In addition, the boundaries can be intermittent, microlobular, etc.
The doctor is able to palpate large neoplasms; in this case, the patient is referred for a more detailed examination to an endocrinologist.
Type of nodule in the thyroid gland.
Ultrasound allows you to conduct a more detailed examination of a suspicious element and identify its density, which is usually determined by echogenicity, or, more precisely, by the reaction of the examined tissues to the effects of ultrasound radiation sent by the device. As a rule, the density of the node depends on the stage of the disease. Initially, absolutely all formations in the thyroid gland are exclusively isoechoic. (see How to do an ultrasound of the thyroid gland).
This segment has dilated blood vessels along its periphery, which nourish it well and are diagnosed as a capsule on the ultrasound monitor. This pathological segment does not change or affect the functioning of the organ in any way, therefore it is clinically considered harmless until the neoplasm moves to the next stage.
Stages of development of deviation in the thyroid gland
There comes a point when the follicles located inside the affected area begin to die, leaving behind fluid and/or daughter cysts.
A cyst forms.
On ultrasound, this structure is defined as hypo- or anechoic and can be clinically manifested by choking, voice changes, a feeling of a lump in the throat, or again may occur unnoticed by the patient.
After a long time, the cyst can resolve, overgrown with connective tissue and leaving behind a scar. This is a favorable outcome of the disease that does not require surgical intervention.
Symptoms
It is worth considering the fact that the neoplasm can have a malignant course, therefore, as it grows, symptoms such as compression of the esophagus, trachea, ligaments, etc. may occur. Accordingly, the larger the node, the brighter the symptoms.
If you have such a pathology, you should pay attention to the following symptoms:
- Any difficulty breathing, symptoms may appear when changing body position.
- Hoarseness of voice.
- Difficulty swallowing.
- Feeling of a lump in the throat.
- The appearance of irregularities in the neck or a uniform increase in its size.
Any manifestations of the disease depend entirely on the location of the node and its size. If the formation is located on the outside of the organs, then there will be no symptoms of compression of the vessels, trachea and esophagus. Similar formations can be detected by palpation and ultrasound of the throat and larynx.
Palpation (palpation) of the thyroid gland.
Completely different symptoms are observed when the node is located inside the gland. The manifestation of other symptoms is also possible when the organ begins to produce excessive amounts of hormones. As a rule, all signs of the development of thyrotoxicosis are noted:
- tachycardia;
- fast fatiguability;
- excessive sweating;
- significant weight loss;
- sudden change of mood;
- tremor of the upper extremities.
Is it worth treating isoechoic changes in the thyroid gland?
If the formation does not have a negative effect on the patient’s hormonal background and does not cause any negative sensations, then such a node does not need treatment. The patient is advised to monitor the dynamics of the node, this will allow him to keep the condition of the defect under constant control and, if the situation worsens, take all necessary measures to eliminate the negative consequences.
But it should also be noted that if such a node was found in the thyroid gland, this could mean the following:
Benign formation
When monitoring the problematic isoechoic segment, no progression symptoms are detected. Most often, such formations occur in the following pathologies:
- nodular goiter;
- follicular adenoma;
- in nodes of adenomatous type.
The prognosis is unfavorable.
Isoechogenic inclusions in the kidneys
Isoechogenic formations in the kidneys on ultrasound do not differ in density from the rest of the unchanged parenchyma of the organ. On an ultrasound, the formation is clearly visible on the device screen. Isoechogenicity in the kidneys is characteristic of various defects or cancerous tumors. On ultrasound, isoechoic inclusions look like a heterogeneous spot with uneven edges.
conclusions
Thus, the presence of an isoechoic formation in almost all cases means that a tumor disease of a malignant or benign nature has been detected in the body.
An isoechoic formation is not necessarily cancer.
In any case, ultrasound is only a screening method of examination, and to establish a more accurate diagnosis, many other additional laboratory or instrumental techniques are used.
Source: https://UziKab.ru/pro-uzi/izoehogennoe-obrazovanie.html
Types of hypoechoic formations
Isoechogenic formations can form in various tissues of the human body. But most often they are found on the thyroid gland, liver, uterus, mammary glands and ovaries. Such segments on the thyroid gland form in the form of nodes that encircle it, which can cause coughing, a feeling of suffocation, and the tumor constantly increases in size. In fifty percent of cases, such nodes are heralds of the development of cancerous tumors. Areas that have an acoustic density similar to the surrounding tissues are also found in the uterus, ovaries, and liver.
An isoechoic area of tissue is considered dangerous and malignant if:
- it has an irregular and uneven shape
- node boundaries are unclear
- there are hyperechoic inclusions, which indicates calcification
- the structure of the vessels surrounding the segment is convoluted
- psammotous bodies were detected inside the segments
In these cases, the prognosis is unfavorable; the neoplasm most likely requires surgical intervention.
Don’t be afraid, because such segments can be benign and can be treated without consequences for the body. The most important thing is to detect them in time.
The concept of a neoplasm
Isoechogenic formation is understood as a certain area of tissue or internal organ, which during ultrasound examination has a density similar to other tissues. Education - a tumor of a benign or malignant nature. Also, such an area can appear after internal injuries and hematomas.
There are 2 types of structures identified by ultrasound. Each type is described in the table.
| Hyperechoic formation | The fabric has a dense structure. It is displayed on the screen with an intense light color. |
| Hypoechoic formation | The fabric has a low density. Can be recognized on the monitor by its dark color. |
Isoechogenic formation differs from those listed in that it is quite difficult to recognize the disorder. The density of the formation completely coincides with the surrounding tissues. With intensive growth, the tumor begins to compress neighboring tissues.
An isoechoic nodule has a rim. It consists of capillaries that gradually increase in size. Gradually, cell death may begin. This leads to the development of hypoechoic formation.
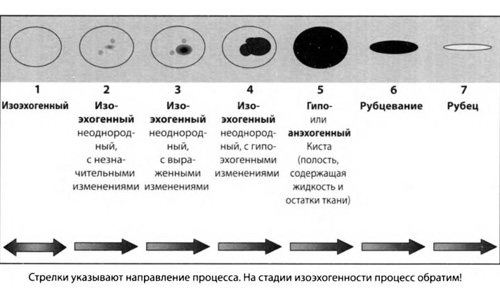
The isoechoic node has a different shape at different stages
In the initial stages, the changed area does not affect the surrounding tissue in any way. There are no pathological symptoms. Clinical signs appear over time.
Isoechoic neoplasms are divided into types depending on size:
- small with a diameter of up to 12 mm;
- medium with a diameter of 20–30 mm;
- large with a size of 45 mm.
Changes can be either significant or minor. Negative factors can provoke the formation. The most common root causes include:
- hereditary predisposition;
- bad environment;
- lack of iodine in the body;

Smoking and alcohol can provoke the development of the process
- bad habits;
- inflammatory processes in the body;
- prolonged exposure to a stressful situation;
- poor nutrition.
These factors significantly increase the risk of an isoechoic neoplasm. The greatest danger is posed by malignant formations.
Effective treatments
Treatment of affected tissues aims to prevent their growth and development. It is important to constantly monitor the dynamics of their development. Therefore, if they do not change in size, they often do not require treatment.
An important role is played by diagnostics and constant monitoring of the condition. If the affected area constantly increases in size and unpleasant symptoms interfere with the patient’s normal life, it requires treatment. Therapy, depending on the degree of malignancy, is carried out in two forms: medication and surgical intervention. Surgery is a last resort when the cancerous nature of the tumor is confirmed.
Diagnostic methods
The main diagnostic method for suspected isoechoicity is ultrasound. The procedure is painless and does not cause any discomfort. You can undergo examination even during pregnancy and under the age of 18 years.
Every organ and tissue has echogenicity. It is thanks to this that ultrasound transmits the image to the screen and makes it possible to recognize the pathological process.
Only after ultrasound and confirmation of isoechoicity are the patients referred for further examinations. They are selected individually and directly depend on the location of the lesion.
Isoechogenic formations of the ovaries
Formed as a result of the accumulation of secretory fluid. They look like a bubble with liquid inside it. The constant presence of fluid leads to the development of a cyst and its corresponding growth. If the cyst does not grow or develops slowly, this condition only requires being under the supervision of a gynecologist. But the continuous enlargement of the cyst leads to the fact that the ovaries begin to interfere with the functioning of other organs, so in this situation, surgical intervention is inevitable and must be carried out as quickly as possible to prevent disruption of healthy parts of the body.

Causes and risk factors for the development of uterine fibroids
To date, no obvious causes of this disease have been identified. Probable causes include hormonal imbalance in the body towards the predominance of estrogen over progesterone. This happens in the following cases:
- Early menarche
– increases the number of cell divisions, which increases the risk of mutations in genes that control myometrial proliferation. - Reproductive dysfunction (absence of childbirth)
. Anovulation - with infertility, there is a continuous exposure of estrogens to the myometrium, while pregnancy reduces the time of free exposure of estrogens to the myometrium. - Obesity leads to insulin resistance of body cells
- the fraction of free estrogens increases. At the same time, the conversion of androgens to estrogens in adipose tissue increases - this mechanism is more important in postmenopause.
The growth of nodes (fibroids) is stimulated by such physical factors as insolation, physiotherapeutic procedures in the pelvic area, massages, that is, everything that increases blood circulation in this area. Hereditary predisposition plays a certain role (the presence of fibroids in a mother, sister, grandmother, etc.). There is also an immune theory of the occurrence of these formations: rapid growth of fibroids is observed with severe immune disorders, which contribute to increased cell growth, angiogenesis and inflammation. Various growth factors play an important role. Damage to the structure of the uterus: curettage, inflammation, mutations - lead to the expression of growth factors and increase the risk of uterine fibroids and endometrial pathology. Uterine fibroids can occur for a long time without significant clinical manifestations.
Isoechogenic nodule in the thyroid gland
An isoechoic thyroid nodule may indicate various disorders. This gland is a very sensitive organ; it tends to react sensitively to all adverse environmental influences, as well as to everything that happens inside the human body. It is for this reason that nodes may appear in this organ.
Such a formation can be diagnosed by palpation only if it is large. Small nodules are usually discovered by chance. If its density does not differ from the rest of the gland, then we should talk about an isoechoic node. The isoegenicity of the nodes varies depending on the stage. In the initial stages, all nodular formations have an isoechoic structure.
Isoechogenic nodes can be: In the initial stage, nodular growth is detected only by the rim surrounding it, which is formed due to increased blood flow to this area (the number of capillaries increases). With a general isoechoic background of the node, different areas are possible.
- with minor changes in structure;
- with significantly altered tissues;
- with hypoechoic inclusions.
How does such an isoechogenic neoplasm develop? In the initial stages, the echogenic structure is normal, so the follicles of these nodes can still produce hormones. But as the degenerative process progresses, the follicles die. Initially destroyed, they have limited areas, as a result of which cavities are formed. This cavity appears as a hypoechoic area on ultrasound examination.
If there is no appropriate treatment, the pathology begins to worsen. The cavities enlarge and fluid appears in them. A cyst forms.
This cyst exists for some time, then the fluid contained in it resolves. After this, scarring occurs. This indicates the onset of the next stage, when connective tissue forms at the site of the cyst. This stage can drag on for several years. How quickly this process develops depends on the individual characteristics of the organism, on the size of the growth itself and on how much the organ itself can adapt.
Further diagnostics
If an isoechoic neoplasm is detected on ultrasound during an ultrasound examination of the thyroid gland, a more in-depth diagnosis of this organ should be carried out. First, using a puncture with a thin needle and a syringe, material for a biopsy is taken. This study helps to clarify the cytomorphological structure of this node.
To determine if there is a malfunction of the organ, scintigraphy is performed. During this study, radioactive isotopes are injected into the patient's body, which allows a two-dimensional image of the gland to be obtained.
Bronchoscopy and laryngoscopy are performed if there are symptoms of compression of the trachea and larynx. It is possible to determine whether a nodule is malignant or benign using computed tomography. It also helps to determine the boundaries of the node, whether it has grown into nearby tissues and whether the vascular network is disrupted.
Recently, MRI of the thyroid gland has been increasingly used, which can accurately determine how far the process has gone, whether there are structural changes in the organ, what its shape and size are, see possible pathological transformations of its tissues, and the presence of neoplasms. The study makes it possible to see a layer-by-layer image of the gland.
If symptoms appear indicating an enlarged thyroid gland, you must consult a specialist and undergo an ultrasound examination. Usually, with timely detection, almost all isoechoic nodes are benign. But even with a malignant process in the organ, most patients are cured. The prognosis is unfavorable only in advanced cases, that is, if metastases are detected in other tissues and organs.
What is an isoechoic formation, what does it look like and can it develop into cancer?
An isoechoic formation is difficult to detect on ultrasound. It can be benign or malignant. Additional examination methods are used to make a diagnosis.
What is isoechoicity
The main criterion for ultrasound examination is echogenicity. This is the ability of internal organs to reflect sound at different speeds. The property depends on the density of the fabric.
The denser the organ, the better it reflects. The image has a light gray or white color and is called hyperechoic. Soft organs and fluid do not reflect sound well and are shown by ultrasound as dark gray or black areas. The property is called hypoechogenicity.
Pathological formations are also assessed - stones, tumors, cysts. Neoplasms with isoechoicity are much less common. This means that they have the same density as the surrounding tissue. Their color corresponds to the color of the organ being examined.
Description in different organs
Due to the fact that isoechoic formations correspond in density to organs, it is difficult to see them on an ultrasound image. The presence of an isoechoic neoplasm can be suspected by tissue compression or the presence of a capsule.
Formations with an isoechoic structure are detected everywhere:
- kidneys;
- liver;
- thyroid;
- liver;
- breast;
- ovary.
Most often they are benign in nature. Oncological pathology has distinctive features, which are confirmed by additional research methods.
Kidneys
Kidney formations that are isoechoic are most often malignant tumors. They are characterized by strong compression of surrounding tissues and uneven outlines. The tumor often grows into the ureter.
Cysts and kidney stones are never isoechoic. Cystic formations contain fluid and are therefore represented by black areas. The stones are very dense and look like white uneven inclusions.
Ovaries
An isoechoic nodule with a hypoechoic rim is an ovarian cyst. It is formed by a greatly enlarged follicle. Cysts are discovered before ovulation. In the image, the cyst is presented as a rounded gray spot with a white rim around it.
Irregular isoechoic areas are a sign of ovarian cancer. Compression of neighboring follicles and their deformation are noticeable. Cancer is characterized by rapid growth.
Thyroid
An isoechoic node is a sign of goiter against the background of preserved hormonal function of the gland. You can determine it by changing the direction of grain in the image. A compaction zone also appears around the node.
Oncological alertness should be shown if white areas appear inside such a formation. This is a sign of calcification, which often accompanies cancer.
How nodes and cysts look on an ultrasound can be seen in the video:
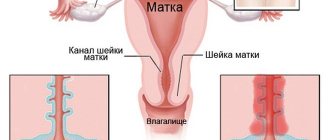
Uterus
Isoechogenic formations are myomatous nodes or polyps. Myoma is located inside the wall of the uterus or protrudes into the cavity. The image shows a spot of heterogeneous density. Its size can reach tens of centimeters.
Polyps always protrude into the uterine cavity. They look like small oblong gray spots on a dark background. If you do an ultrasound during different phases of the menstrual cycle, you may notice a change in the size of the polyp.
Myomas and polyps can become malignant tumors. Therefore, you need to do an ultrasound every six months to monitor the dynamics.
Liver
Isoechogenic formations in the liver are most often hemangiomas. They are represented by gray spots with increased blood flow. They have rounded outlines and do not compress surrounding tissues. Hemangiomas are tumors from overgrown vessels.
Isoechogenic spots may turn out to be lipomas. This is a growth of adipose tissue. Formed as a result of poor nutrition and alcohol abuse. They have a round shape and clear boundaries.
Malignant neoplasms are less likely to be isoechoic. They can be distinguished by blurry outlines and compression of the tissue around them.
Read more about formations in the liver here.
Breast
A spot with anechoic inclusions, that is, black dots, is a cystic adenoma of the mammary gland. This is a hormone-dependent neoplasm. It changes size depending on the phase of the menstrual cycle. A white capsule is clearly visible around the gray spot in the image.
Cystic adenoma is not dangerous to a woman’s health. But it can transform into cancer under certain conditions. Rapid growth of the adenoma and the appearance of discharge from the nipple are indications for surgical treatment.
Isoechogenic formations are a rare finding on ultrasound. Usually these are benign changes. Observational tactics are used against them. As long as the tumor does not grow and does not compress surrounding tissues, treatment is not necessary.
Leave comments on the article, share information with friends on social networks. All the best.
Source: https://uziman.ru/metodika/izoehkhogennoe-obrazovanie
Carcinoma
Carcinoma can be completely shapeless or, on the contrary, it can have completely clear contours. Such nodes occur in a quarter of all existing cases of cancer. Most often, such nodes have uneven outlines and fully correspond to papillary carcinoma.
Cancer is found in the capsule in almost 50% of cases, having completely normal echogenicity and clear, even boundaries. In this case, the picture on the ultrasound screen is as follows:
- Wrong form of education.
- Clearly preserved contour.
- Fuzzy near the boundaries of the node.
- The presence of any hyperechoic inclusions usually indicates calcification.
- The presence of psammotous bodies inside the node.
- The presence of a convoluted structure in the vessels surrounding this section.
The prognosis is unfavorable.
Complaints in the presence of uterine fibroids are varied
- Pain in the lower abdomen and lower back
. The pain can be of a different nature (depending on the location and size of the node): cramping, aching, periodic. When the pedicle of the subserous node is torsed or the node becomes necrosis, a picture of an acute abdomen develops: severe pain, nausea, vomiting, increased body temperature, leukocytosis, dysfunction of the bladder and rectum. - Various irregularities of the menstrual cycle:
more abundant, prolonged, with clots, painful menstruation, anemic syndrome. - Absence of pregnancy or miscarriage.
The longer the duration of the disease, the more often reproductive dysfunction is detected. - With large nodes, dysfunction of the pelvic organs is possible:
frequent urination (in the presence of a large fibroid node in the bladder area), constipation, venous stasis, hemorrhoids, compression of the sacral nerves, vena cava, and ureters.
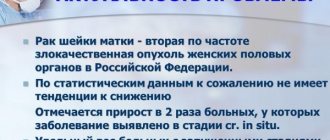
Cervical examination
Author: rasurgut from 22-11-2014, 12:27, views: 33,681
12
Cervical diseases are a fairly common gynecological pathology; on average, up to 55% of women, when visiting a gynecologist, encountered various manifestations. Basically, these are background diseases that are asymptomatic, completely reversible under the influence of appropriate therapy, or often do not require specific treatment and heal on their own. In recent years, there has been an increase in the number of cases of cervical disease in young women. The age range from 15 to 24 years is critical in relation to exposure to harmful factors. Modern diagnosis of cervical pathology is based on a wide arsenal of special studies: Examination of the cervix in the speculum with various tests when a pathological area is detected. Survey, extended and microcolposcopy - examination of the cervix with a magnification of tens and hundreds of times using a colposcope or an optical system for “intravital histological examination”. Cytological studies and biopsy. Quite rarely, if a malignant process is suspected, cervicoscopy, cervicohysterography, MRI, CT, angio- and lymphography are used. The capabilities of ultrasound diagnostics are not sufficiently used by gynecologists, despite the high information content and availability of the method in a whole group of cervical diseases. This is due to the relatively recent introduction of the transvaginal pelvic ultrasound method, where the probe is placed directly to the cervix. Ultrasound can be used as an important additional method in examining patients with cervical pathology, which allows one to assess the thickness and structure of the mucous membrane of the cervical canal, and identify formations and inclusions of the muscular layer of the cervix. In addition, echography provides additional information about the size, structure of the cervix, characteristics of the blood supply (with digital Doppler mapping and pulse Doppler), the condition of the parametrium, and sometimes the pelvic lymph nodes. Some of the most common reasons for sending patients for ultrasound of the pelvic organs to examine the cervix are: Cervical cysts and polyps of the cervical canal Hypertrophy or severe deformities of the cervix Uterine fibroids and endometriosis Female sexual dysfunctions, accompanied by pain and contact bleeding during or after sexual intercourse. Dysmenorrhea (painful menstruation) and pelvic pain of unknown etiology. Stress urinary incontinence against the background of prolapse (prolapse) of the pelvic organs. Suspicion of cervical cancer Preparation for pregnancy, childbirth Infertility examination Preparation for IVF (in vitro fertilization). The cervix
is the lower segment of the uterus.
The wall of the cervix is a direct continuation of the wall of the uterine body. The junction of the uterine body and the cervix is called the isthmus. While the uterine wall is primarily composed of smooth muscle, the cervical wall is primarily composed of connective tissue. The lower part of the cervix protrudes into the vaginal cavity and is therefore called the vaginal part of the cervix, and the upper part, lying above the vagina, is called the supravaginal part of the cervix
.
The cervical canal, located in the cervix, connects the uterine cavity and vagina. On the vaginal part of the cervix, the external os
- a branch leading from the vagina into the cervical canal and continuing into the uterine cavity, where it opens
with the internal os
.
Ultrasound picture 1. The position of the cervix in relation to the body is determined.
The cervix is located at a wide angle to the body of the uterus, the narrowing of this space and the sharpening of the angle refers to the so-called inflections of the uterus
2. Shape
The cervix has a cylindrical shape, in cross section in the form of an oval
3. Contours
The contours of the cervix should be smooth and clear.
Here the thickness of the anterior and posterior walls is assessed; normally it is the same 4. Dimensions
The dimensions of the cervix vary widely.
Not only individual anatomical and physiological characteristics are important, but also previous pregnancies that resulted in childbirth through the natural birth canal. The maximum size of the cervix/hypertrophy of the cervix/ is 37*30*34 mm and the minimum size/shortening of the cervix/ is 29*26*29 mm, the most important indicator for a successful pregnancy. The physiological ratio of the length of the uterine body to the length of the cervix is assessed (3:1 in reproductive age) 5. Echogenicity
The myometrium of the cervix has a slightly greater echogenicity in relation to the body, due to a more pronounced fibrous component in the muscle tissue
6. Structure
The myometrium of the cervix should have a homogeneous structure.
Single round anechoic inclusions up to 5 mm and hyperechoic inclusions in women who have given birth are interpreted as a variant of the norm. Hypoechoic round formations visualized in the wall of the cervix are most often represented by endocervical cysts. 7. The cervical canal of the cervix is assessed separately according to several parameters.
The cervical canal is represented by a hyperechoic (bright) linear structure.
Its contours are clear and even. The width of the cervical canal, the thickness of the mucosa (endocervix), the assessment of folding, the presence of polypoid formations, the deposition of calcifications, and the identification of other pathological areas are carried out. Much attention, especially in pregnant women, is paid to examining the internal os of the canal. The external os and superficial structures of the vaginal part of the cervix are in most cases poorly visualized, so their assessment must be treated with extreme caution. The echographic picture of the cervix does not undergo significant changes during the menstrual cycle. Significant differences during the secretory period (menstruation) are the high echogenicity (brightness) of the endocervix in combination with the heterogeneous internal echostructure of the canal contents, due to the presence of a rejected component (bleeding). Classification of cervical diseases.
/important in ultrasound diagnostics/ Cervicitis Cervicitis is a total inflammation of the cervix, including the mucous membrane of the vaginal part of the cervix (exocervicitis) and the mucous membrane of the cervical canal (endocervicitis).
In the postmenopausal period, atrophic cervicitis develops due to thinning of the cervical mucosa. Superficial cervicitis and erosions are not examined by ultrasound; the echo signs of endocervicitis are quite conditional and are associated mainly with changes in the ultrasound picture of the cervical canal, which cannot be explained by other reasons. For example, disruption of the contours and expansion of the cervical canal, thickening of the endocevix, multiple cysts or microcalcifications in a nulliparous woman will be classified as this pathology. Cervical cyst Cervical cyst is a common pathology, mainly due to inflammatory changes or hormonal imbalance. There are single and multiple cervical cysts. Gynecologists call such cysts “Nabothian cysts” or “Ovulae Nabothii”. Nabothian cysts arise as the end result of “self-healing” of cervical ectopia/i.e. This is a type of cervical erosion/. There is a blockage of the excretory ducts of the glands of the cervix and a thick grayish secretion in the form of mucus accumulates under the thin transparent capsule. Round anechoic inclusions detected on ultrasound in the cervix are considered to be nabothian gland cysts; the detection of fine suspension in similar inclusions with thickening of the wall in which they are located usually indicates endometriosis of the cervix. Polyp of the cervical canal and endometrium on a stalk Polyps of the mucous membrane of the cervical canal are connective tissue outgrowths covered with epithelium. On ultrasound they are usually visible as hyper- and isoechoic oval-shaped formations that dilate (widen) the cervical canal. As a rule, they have a stalk, when lengthened, polyps that arise in the middle and upper part of the mucous membrane of the cervical canal can appear from the cervical canal. Differential diagnosis is necessary with large endometrial polyps or with polyps emanating from the lower third of the uterine cavity. Modern ultrasound equipment with high resolution makes it possible to diagnose small polyps that do not extend beyond the external pharynx. They look like inclusions of increased or moderate echogenicity in the cervical canal. After the diagnosis of a polyp of the mucous membrane of the cervical canal is established, regardless of the patient’s age, polypectomy with careful removal of the polyp stalk or its coagulation under endoscopic control is indicated. Often, at the same time as a polyp of the cervical canal, a polyp or endometrial hyperplasia is detected. Polyps are a benign disease
.
However, sometimes cancer (especially adenocarcinoma) can have the appearance of a polyp. Uterine fibroids, located in the cervix or a “nascent” myomatous node Cervical fibroids are very rare and make up only 8% of all locations of uterine fibroids. In some cases, it is possible to detect a “nascent” submucous myomatous node. They can also be subserous, intramural and submucosal. Ultrasound signs of cervical myomatous nodes are generally identical to changes in the body of the uterus. The presence of cervical fibroids in the vast majority of cases is an indication for surgical treatment. Ectopic pregnancy Very rarely, implantation of a fertilized egg can be observed in the cervical canal (cervical pregnancy). In these cases, the fertilized egg is visualized in the cervix in the form of a round hypoechoic formation. In fact, it is uterine, / because The cervix is part of the uterus, but is considered dangerous to an ectopic pregnancy and requires immediate medical intervention. Endometriosis of the cervix or surrounding tissue Genital endometriosis is a common disease in women of reproductive age. The causes of endometrioid lesions of the cervix are diathermocoagulation of ectopia (cauterization of erosion), damage during surgical abortion, childbirth. On the relatively deep wound surface, pieces of endometrial tissue, released during the next menstruation, attach and “take root.” The ultrasound picture is represented mainly by cervical cysts - round hypoechoic formations, often with heterogeneous, hyperechoic content. A distinctive feature of endometrioid cysts of the cervix is the thickening of the wall in which the cyst is located. Cervical endometriosis usually manifests itself in the form of bleeding on the eve of menstruation. Endometriosis of the pericervical tissue is visualized in the form of hyperechoic (increased brightness) areas in the adipose tissue, with clear, uneven contours, manifested by periodic pain in the posterior vaginal vault, which is not amenable to conventional, in this case, anti-inflammatory therapy. Narrowing of the cervical canal, atresia of the cervical canal and vagina. With atresia of the cervical canal and vagina, ultrasound allows the installation of a hematometer in cases of a functioning uterus. Atresia of the hymen is characterized by the development of hematocolpos, the size of which depends on the height of vaginal obliteration and the amount of accumulated blood. Ultrasound reveals a large amount of heterogeneous, hypoechoic fluid in the uterine or vaginal cavity, respectively. Cicatricial changes in the cervix (post-traumatic changes and strictures, including after abortion and childbirth) Deformation of the cervix occurs as a result of traumatic childbirth or surgical interventions on the cervix. During labor, the cervix shortens, flattens, and then dilates to a diameter of 10 cm, allowing the fetal head to pass through the mother's birth canal. Sometimes, during the passage of the head, the cervix ruptures. In such cases, the cervix after childbirth is formed defective - the cervical canal often remains gaping, and the cervix itself can take on the most bizarre shapes. Cervical cancer
This is a dangerous malignant disease. Cervical cancer ranks third among cancer pathologies in women, second only to breast and uterine cancer, and has a tendency to grow rapidly and metastasize. According to the degree of invasion (germination of layers located under the epithelium), cancer is divided into carcinoma in situ, minimally invasive, and invasive cancer. Invasive cancer has 4 stages, depending on invasion into neighboring organs, involvement of regional lymph nodes and the presence of distant metastases (bones, liver, brain). Ultrasound diagnosis of cervical cancer in the early stages of development is not possible, and is usually used to clarify the stage of the malignant disease, the degree of invasion of the oncological process and search for metastases. Examination of women in order to prepare for pregnancy and childbirth, management of infertility and IVF will be discussed in separate sections.
Tags: pelvic ultrasound of the cervical organs pain in the lower abdomen cyst cancer uterine fibroids ectopic pregnancy endometriosis
- 80
Category: Pelvic ultrasound / Cervical ultrasound