Laparoscopic hysterectomy, or hysterectomy, is one of the most common surgical procedures, along with cesarean section and laparoscopic gallbladder removal, in developed countries. Every year, according to statistics, more than half a million hysterectomies are performed using laparoscopy worldwide. For example, in the United States of America, since the 1980s, 10 hysterectomies are performed for every 15,000 women.
The frequency of hysterectomy by laparoscopy depends on the region and cultural development of people, as well as their social status and psycho-emotional attitude towards surgery.
According to world literature, three quarters of hysterectomies are performed abdominally, and only one fourth of all operations are performed through vaginal access. Open laparotomy more often leads to the development of complications, massive blood loss, requires much longer time for recovery after surgery, a rehabilitation period and the opportunity to start work. At the moment, there is a persistent change in treatment approaches in favor of uterine laparoscopy, which has medical, psychological, social and economic significance.
For the first time, laparoscopic removal of the uterus was performed by the American surgeon H. Rich in 1988, which influenced the development of laparoscopy in gynecology not only in the USA, but throughout the world. And already in the early 90s, a surgeon from France M. Kanis performed a hysterectomy using laparoscopy in a woman with cervical cancer. In Russia, the laparoscopy technique for removing the uterus was first performed in 1993 by V.I. Karnaukh.
According to H. Rich, laparoscopic removal of the uterus may not be used if it is possible to perform a vaginal hysterectomy.
Classification of laparoscopic hysterectomies
At the present stage of development of laparoscopy, there are several classifications for hysterectomy. The most popular among them is the classification proposed by H. Rich.
<р3>The following methods of laparoscopic removal of the uterus are distinguished:
- Diagnostic laparoscopy in combination with transvaginal removal of the uterus - this technique allows us to first evaluate the possibility of transvaginal access and its further use;
- Vaginal hysterectomy under laparoscopy control - first, laparoscopic removal of adhesions, tissues damaged by endometriosis, removal of the appendages and ligamentous apparatus of the uterus is performed, and at the second stage, ligation of the arteries and removal of the uterus are performed, like a classic vaginal hysterectomy. It is believed that true laparoscopic hysterectomy is difficult to perform, therefore, in order to avoid possible death and complications, specialists are recommended to perform this particular type of uterine laparoscopy;
- True laparoscopic hysterectomy - performed only using laparoscopic access and instruments, including ligation of the uterine artery;
- Total hysterectomy – a gynecological surgeon removes the uterus and ligates blood vessels, as well as creating a stump through a laparoscope;
- Supravaginal laparoscopic removal of the uterus (subtotal hysterectomy);
- Laparoscopic restoration of the pelvic floor and vaginal hysterectomy - if it is impossible to reconstruct the perineal muscles, eliminate genital prolapse or urinary disorders when performing a classic hysterectomy through the vaginal access, then laparoscopy is used in parallel;
- Laparoscopic removal of the uterus and lymph nodes;
- Hysterectomy according to the Semm method with removal of the mucous membrane of the cervical canal.
Execution technique
The surgery is performed under general anesthesia. Already in the operating room, antibiotics are administered to prevent surgical infection. The technique used depends on the chosen access and the extent of resection.
In general, the operation can be divided into several stages - preparation of the uterus, intersection of ligaments, vascular hemostasis, organ cutting and closure of the resulting defect.
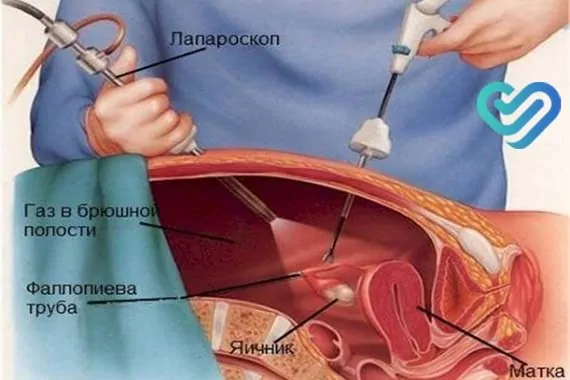
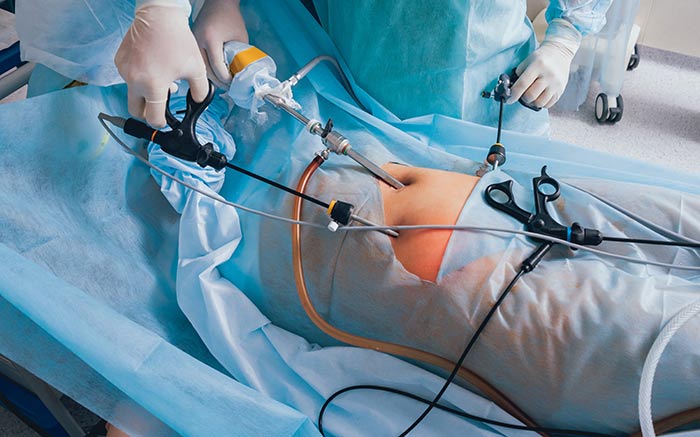
Laparoscopically assisted vaginal hysterectomy, which combines the advantages of several approaches, is of some interest. During the operation, three trocars are used, which are inserted through small incisions on the anterior abdominal wall. A uterine manipulator is inserted through the vagina, with the help of which the surgeon coordinates the position of the uterus in the pelvis, which facilitates the intervention, reduces the duration and prevents complications. Then the round ligaments are crossed on the right and left, and the bladder is separated.
With a subtotal hysterectomy, the surgeon cuts the fallopian tubes and the ovarian ligaments without affecting the cervix, while a total resection involves the removal of all parts of the organ. The next stage is hemostasis. The uterus is abundantly supplied with arteries and veins that feed it. The vessels are coagulated at the level of the internal os, where after hemostasis the body of the uterus will be cut off from its cervix. The resulting defect is closed using peritoneal sheets during subtotal hysterectomy. This process is called peritonization. Whereas with total resection, sutures are placed on the vaginal wall. The uterus is removed using a morcellator, a device for grinding tissue. The organ is removed through the abdominal cavity or through the posterior vaginal fornix. At the end of the operation, the obstetrician-gynecologist carefully checks the pelvic cavity and monitors hemostasis.
For women at risk for developing prolapse, after removal of the uterus, the posterior vaginal vault is strengthened. This manipulation is called culdoplasty.
Contraindications to surgery
- Uterine prolapse is a case in which the optimal option would be to remove the uterus not by laparoscopy, but transvaginally;
- An increase in the size of the uterus before the 16th week of pregnancy is considered a relative contraindication and depends on the experience of the surgeon who will perform the surgery;
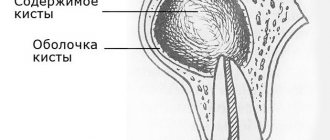
- The presence of large adnexal cysts that will not allow for intact removal due to the impossibility of moving them into a special laparoscopic bag.
During preparation for uterine laparoscopy, it is necessary to perform a number of mandatory laboratory and instrumental studies, according to the standards of preoperative preparation in gynecology. If the size of the uterus and myomatous nodes does not allow laparoscopic removal of the uterus, then gynecologists prescribe a course of hormonal therapy to reduce them. The duration of such therapy depends on the response to the drugs and on average lasts about six months. At the same time, iron deficiency in the body is corrected by prescribing replacement medications.
Before the operation, a course of antibiotic therapy is prescribed to prevent the development of infectious complications. The day before the intervention, the patient is recommended to eat only liquid food, and also cleanse the intestines using enemas or laxatives. Also, before laparoscopy of the uterus, a catheter is installed in the bladder.
At the moment, the technique of total laparoscopic hysterectomy according to Broy, from the University of Clermont-Ferrand, is considered the most progressive and effective method of uterine laparoscopy.
It meets the following requirements:
- Ease of implementation and quick learning of the technique by specialists;
- Reliable and safe, with a low risk of injury to neighboring organs and nearby tissues;
- Low cost of the operation, which makes it cost-effective and accessible to all segments of the population.
Recently, partial laparoscopic hysterectomy has not been inferior in frequency, especially in cases of treatment of benign uterine tumors in young patients, because the trauma associated with amputation of the uterus is significantly lower than with its extirpation. There are also significantly fewer cases of ureteral injury.
The advantages of this laparoscopic operation are:
- Preservation of the morphofunctional structure of the pelvic floor and prevention of genital prolapse in the future;
- Low incidence of sexual disorders and decreased sexual libido;
- Low level of complications compared to laparoscopic hysterectomy.
The disadvantages of laparoscopic supravaginal amputation of the uterus are considered to be malignancy of the cervical stump and minor menstrual-type discharge for some time after surgical treatment.
Complications
Complications that may arise in the postoperative period include:
- postoperative bleeding;
- suppuration of the surgical wound;
- formation of adhesions in the abdominal cavity.
A special feature of this intervention is changes affecting the reproductive function of women. This could become a psychological trauma for her, but there is no point in worrying and worrying about this. You need to correctly assess the pros and cons of the operation.
So, after surgery to remove the uterus, the following consequences are possible:
- cessation of menstruation - surgical menopause or amenorrhea;
- absolute infertility - it is possible to obtain offspring only through IVF with a surrogacy program;
- reducing the risk of developing ovarian cancer;
- increased risk of pelvic organ prolapse.
The cessation of menstruation does not indicate a loss of femininity. It is important to understand that when the uterus is removed, the ovaries remain in place and continue to function as usual; only the visible sign of their work is absent - menstruation. Therefore, removal of the uterus or removal of the fallopian tubes is not equivalent to the onset of menopause. Menopause occurs in women with a removed uterus at the age at which it would have occurred if the uterus had not been removed. The inability to give birth is a serious problem, especially for those who do not yet have children. But there is a surrogacy program in which your eggs can be used for fertilization. This will be genetically your child. As a last resort, you can adopt a baby; many children from the orphanage need affection and care.
There is, of course, a risk of pelvic organ prolapse, but there are a number of exercises to strengthen the pelvic floor. Additionally, exercising can also help. You need to monitor your weight, as obesity can be a provoking factor. The big plus is that the unpleasant symptoms of the disease that bother you will disappear. In addition, studies show that when the uterus is removed, the likelihood of developing ovarian cancer decreases.
After the rehabilitation period, the woman can lead a normal life and have sexual intercourse.
Possible complications after laparoscopic hysterectomy
- Damage to the ureters and bladder
- Bleeding from uterine vessels that are not sutured
- Inflammation of the stump and surrounding tissue
- Hernias caused by the use of trocars larger than 10 mm
Since during laparoscopy of the uterus it is impossible to palpate the ureter, its initial visualization is a mandatory stage of the intervention, and its location is clarified at the beginning of the operation, since during laparoscopy the peritoneum becomes cloudy and peristalsis of the ureter decreases. If imaging is not possible, surgeons perform a laparotomy and isolate it.
What is uterine laparoscopy?
This method causes less harm to the body and has virtually no complications.
There are two types of laparoscopy:
- diagnostic – it is used to confirm or refute a diagnosis.
- surgical – used for the treatment of female genital organs.
If the disease is in its early stages, this method helps to completely remove the tumor. Even at an advanced stage, laparoscopy allows you to save the uterus and remove only the tumor present in it. This method helps maintain the menstrual cycle and also gives a woman the opportunity to become a mother.
Postoperative period
Patients after removal of the uterus using laparoscopy are prescribed narcotic painkillers on the first day. Due to the possible risk of developing thromboembolism and subsequent complications, anticoagulant therapy is carried out, and antibiotic therapy is used to prevent the development of infection. Already 12 hours after the operation, bed rest is canceled and food is allowed, while diuresis and stool are restored independently. One and a half months after laparoscopy, sexual activity is allowed.
Also on the first day, nursing staff monitors:
- skin color and moisture
- body temperature (a slight increase to low-grade levels is allowed)
- measure pulse and blood pressure
- assess breathing
- control the amount of urine excreted
Before discharge, the gynecologist discusses with the woman information about the recovery process, prescribes the necessary medications and explains the method of caring for the postoperative wound. The doctor also specifies the time for suture removal, depending on the speed of healing and the condition of the tissue.
Features of uterine laparoscopy
This technique has gained great popularity in gynecology, and all because:
- It does not require an incision.
- Prevents the development of adhesions in tissues due to low risk of injury.
- Helps to examine the abdominal cavity in detail.
- It is possible to increase it several times.
- Short rehabilitation period.
- Leaves no marks or scars.
In what cases is laparoscopy performed?
As noted above, laparoscopy has different purposes; some require it to accurately diagnose a disease, while others need it to treat it. It may also be prescribed after surgery to monitor the healing process. But the most common purposes of laparoscopy are:
- fibroids and fibroids;
- abnormal development of the uterus, its prolapse;
- oncological diseases;
- violation of the patency of the fallopian tubes;
- cysts, endometriosis;
- ectopic pregnancy;
- lack of effect from taking hormones;
- infertility treatment;
- trachelectomy and hysterectomy.
When is laparoscopy performed?
Preparation for the operation begins with finding out the patient’s menstrual cycle. This question is very important, because the effect of the procedure depends on it. If you do it during menstruation, you can get an infection, because the female body is most susceptible to various types of infections at this time.
According to gynecologists, laparoscopy is best done immediately after menstruation, or in the middle of the cycle. If this method is required to treat infertility, then it is better to do it after ovulation, so you can see what happens to the egg.
Which method of hysterectomy is better?
It is impossible to say unequivocally which method of extirpation is worse and which is better. Each of them has its own advantages and disadvantages. For example, laparoscopic and vaginal hysterectomy are easier to tolerate by patients, since they do not involve layer-by-layer dissection of the abdominal wall. However, in oncological practice, open intervention is often required, since a thorough examination of the pelvic organs, and in some cases the abdominal cavity, is necessary to search for cancer metastases and radical removal of all interested tissues.
The extent of the operation is determined by the diagnosis and stage of the disease. The most extensive interventions are performed for ovarian cancer, since it is prone to early contact metastasis through the peritoneum. Therefore, during the operation, not only extensive extirpation of the uterus and appendages is performed, but also excision of the greater omentum and peritoneum.
Uterus and appendages in a woman’s body: anatomy and functions
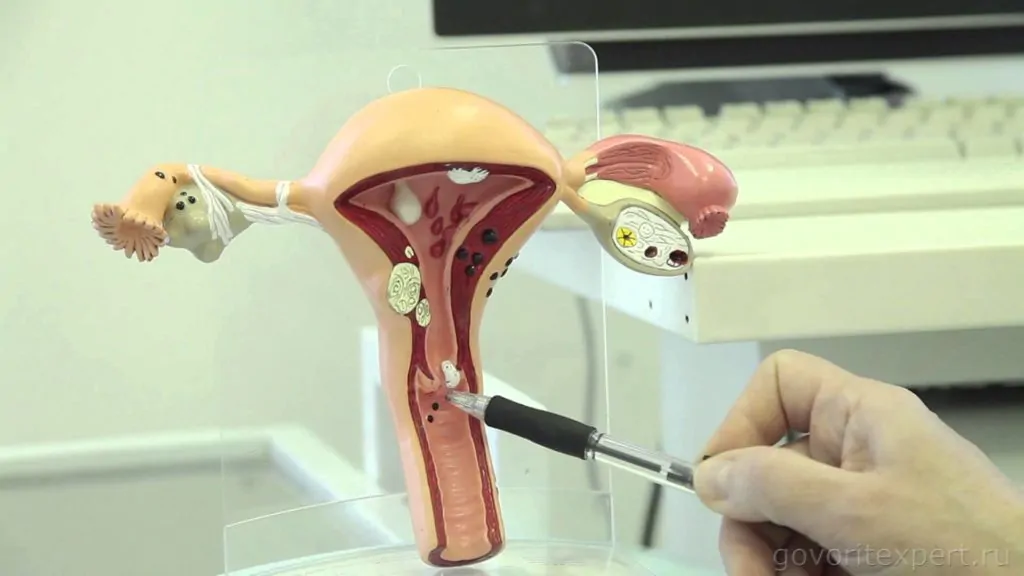
The uterus refers to the internal genital organs of a woman. It is a hollow organ formed by muscle tissue and has a pear-shaped shape, compressed in the anteroposterior direction. Over the course of a woman’s life, the size and weight of the organ changes: in women who have not given birth, the uterus weighs up to 50 grams, in women who have given birth – about 80-90 grams. The length of the virgin uterus is approximately 7-8 centimeters, the thickness of its walls is 1-2 centimeters.
The anatomical location of the organ is between the rectum and the bladder in the pelvic area.
Content:
- Uterus and appendages in a woman’s body: anatomy and functions
- The essence of the procedure for laparoscopy of the uterus and appendages
- Indications and contraindications for laparoscopy of organs
- Preparation for the procedure
- How the operation is performed: types of laparoscopy of the uterus and appendages
- Rehabilitation: what happens after laparoscopy
- Possible complications and consequences of the operation
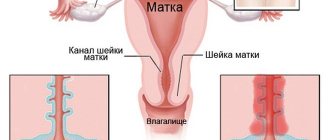
The structure of the uterus is represented by the bottom, walls and a tapering cervix, and it is interesting that the bottom is located in the upper part of the organ, and the cervix at the bottom adjoins the upper part of the vagina.
The main functions of the organ are participation in the process of the menstrual cycle and conception of the fetus. It is in the uterine cavity that the fertilized embryo is fixed, where it develops and grows for 9 months, and the uterus itself stretches significantly.
The ovarian appendages in a woman are rudimentary elements. The appendages are called periovarians. It is the epididymis that is anatomically represented by the supraovaries. It is located between the layers of the mesentery of the fallopian tube laterally behind the ovary.
The epididymis consists of longitudinal ducts and convoluted tubules that flow into them. These tubules are transverse ducts with a small lumen, the blind ends of which are directed towards the hilum of the ovary.

The uterine appendages include the ovaries themselves and the fallopian tubes. The fallopian tubes (fallopian tubes) are paired, oblong-shaped organs. They are located on both sides of the uterus, and connect its cavity with the abdominal cavity.
The ovaries are oval or almond-shaped - paired organs, pinkish-gray in color, about 4 centimeters long, 2 centimeters wide, and approximately 1 centimeter thick. The anterior part of the ovaries is attached to the broad uterine ligament, and their posterior part is free.
The surface of the ovaries is represented by germinal epithelium, under which there is:
- inner medulla;
- outer cortical.
The cortical component of the ovary contains follicles - female eggs that participate in the process of conception.
Extended hysterectomy
This operation involves removing tissue in the following volume:
- Uterus.
- Cervix.
- Fallopian tubes.
- Ovaries.
- The lateral parametrium is removed to the ureters.
- The ureters themselves do not tunnel.
- The anterior parametrium and posterior parametrium are not deleted.
- Blood vessels are excised as close as possible to the uterus.
- Vaginal resection is not performed or is performed to a minimal extent.
- If necessary, pelvic lymph nodes are removed.
This intervention is also called type 1 hysterectomy and is provided for the surgical treatment of stage 1b and 2a cervical cancer. For other types of cancer, the scope of the operation may be wider.