Calcium is a vital macronutrient that performs many functions in the human body (providing muscle contraction, blood clotting, conducting nerve impulses). Calcium is also a major component of bone tissue. Calcitriol (vitamin D) and parathyroid hormone take the most important part in the regulation of its metabolism. Hypercalcemia is a fairly common electrolyte disorder, occurring in approximately 0.17 to 3.9 cases per 100 people. Gender differences vary among people of different ages. Young men and women over 45 are more susceptible to this condition.
Causes of hypercalcemia
Hypercalcemia almost always indicates some disease or pathological process. However, sometimes it develops due to physiological reasons (in newborns on the 4th day of life, in adults after eating). The pathological causes of this condition are as follows:
- Hyperparathyroidism.
This is an endocrine disease characterized by hypersecretion of parathyroid hormone (PTH). It is the most common cause of hypercalcemia. Hyperparathyroidism is caused by adenoma, hyperplasia of the parathyroid glands, and renal failure. Sometimes hyperparathyroidism occurs as part of autoimmune polylinglandular syndrome or multiple endocrine neoplasia. - Oncological diseases.
Recognized as the second most common cause of this electrolyte disorder. In cancer, it occurs through two mechanisms. The first is bone destruction by metastases or primary focus (leukemia, lymphoma, myeloma). The second mechanism is the synthesis of PTH-like peptide by cancer cells (lung, breast, bladder cancer). - Granulomatous processes.
Chronic diseases characterized by the formation of cellular granulomas in tissues (primarily in the lungs) can also cause hypercalcemia. These include tuberculosis, sarcoidosis, histoplasmosis. Mononuclear phagocytes that are part of granulomas, due to the expression of 1-alpha hydroxylase, are able to convert vitamin D into the active form (calcitrirol, 1,25OH-D3), which enhances the absorption of calcium ions by the small intestine. - Prolonged immobilization.
As a result of prolonged inactivity, osteoclasts (cells that destroy bone tissue by dissolving mineral compounds) are activated. This leads to the release of calcium ions from the bones. This phenomenon occurs during forced immobilization after injuries, being in conditions of weightlessness (during space flights). - Taking medications.
This primarily applies to vitamin D and calcium supplements. Other medications (thiazide diuretics, theophylline, lithium) can also cause calcium imbalance by increasing osteodestruction or reabsorption processes in the tubules of the nephrons of the kidneys. - Other endocrine disorders.
In addition to the pathology of the parathyroid glands, other endocrine diseases are sometimes the cause of hypercalcemia. For example, an excess of thyroid hormones in hyperthyroidism increases the destruction of bone tissue. With adrenal insufficiency, the inhibitory effect of glucocorticoids on calcium metabolism is reduced.
Why is calcium elevated?
Why is calcium elevated? If a person is not fond of calcium-containing foods (for example, whole milk and dairy products), does not abuse calcium and vitamin D supplements, and tests still inexorably show its high concentration, the cause of hypercalcemia should be sought in a disease of the internal organs . It could be
- malignant neoplasm, accompanied by increased destruction of bone tissue;
- hyperfunction of the thyroid gland, accompanied by an increase in the level of its hormones;
- primary hyperparathyroidism - excess parathyroid hormone in the blood due to disturbances in the functioning of the parathyroid glands, leading to disturbances in calcium metabolism;
- granulomatous diseases (diseases accompanied by the formation of granulomas - small nodular accumulations of eater cells that capture and digest particles foreign or toxic to the body, including bacteria. Such diseases include sarcoidosis, tuberculosis, leprosy, berylliosis, histoplasmosis, coccidioidomycosis) , in which the inactive form of vitamin D uncontrollably turns into the active form - calcitriol, and calcium begins to be intensively absorbed in the gastrointestinal tract;
- renal, adrenal insufficiency or kidney transplant;
- idiopathic hypocalciuria - a decrease in the amount of calcium excreted in the urine.
An increased concentration of calcium in the blood is often observed with:
— forced long-term bed rest (the absence of gravity and loads on the skeleton increases the destruction of bone tissue);
- overweight, obesity;
- abuse of alcoholic beverages (alcohol stimulates the production of parathyroid hormone, increases its concentration in the blood and, in addition, affects the functioning of liver enzymes that convert passive vitamin D into active vitamin D - calcitriol);
— radiation therapy in the shoulder and neck area;
- long-term use of lithium preparations (reduces the sensitivity of calcium receptors, fraught with the development of mild chronic hyperparathyroidism);
- long-term use of thiazide diuretics (diuretics characterized by reduced excretion of calcium, stimulating the reabsorption of calcium);
- long-term use of theophylline (a bronchodilator that increases the release of adrenaline and norepinephrine by the adrenal glands, activates adrenaline receptors, and thereby leads to the opening of calcium channels and an increase in calcium entry into cells);
- long-term use of thyroid hormones (thyroid hormones that stimulate the destruction of bone tissue).
Pathogenesis
An increase in calcium content in the blood changes the membrane potential of cells, which leads to inhibition of neuromuscular conduction in skeletal muscles, myocardium, and the gastrointestinal tract. The pathogenesis of neuropsychiatric symptoms is not completely clear. The role of slowing down the conduction of nerve impulses is assumed. Calcification of blood vessels, internal organs, dystrophy, and tissue shrinkage develops.
Due to hypercalciuria (increased filtration of calcium in the nephron tubules), the risk of nephrolithiasis increases. Calcium inhibits adenylate cyclase, which suppresses the renal effect of antidiuretic hormone. Also, due to the high extracellular concentration of this cation, the secretion of hydrochloric acid by the lining cells of the stomach increases, which leads to the development of peptic ulcers.
Excess calcium intake shortens life
Want to extend your life? Then reduce your calcium intake. This advice is given by Academician of the Odessa Regional Academy of Sciences Nikolai Grigorievich Druzyak in his outstanding book “How to Extend a Fleeting Life.”
The scientist devoted 20 years of his life to studying the phenomenon of longevity and searching for the factors that determine it. He visited areas famous for the large number of people who have crossed the century mark (Yakutia, Abkhazia, Nagorno-Karabakh, Dagestan, the Nakhichevan Republic, the Lerik region of Azerbaijan and some areas of the North Caucasus), examined local natural water, the healing properties of which are recognized throughout the world, and identified very interesting features:
- In all areas, the water had one common feature - it was SOFT , the content of calcium ions in it ranged from 8 to 20 mg/l. For example, in the water of the Zmeiny spring (Abastumani resort, Georgia), this figure was 12 mg/l. But in the water of the “Golden Key” spring, which is located near Ashgabat and is not famous for its outstanding medicinal properties, it is 40 mg/l.
- The level of calcium concentration in the blood serum of centenarians was radically different from that of ordinary people. It did not exceed 5 mg/100 g of blood .
- In the areas studied, there was no tradition of consuming dairy products . For comparison: just recently, Finland was the generally recognized leader in the production and consumption of milk per capita, and it also led in cardiovascular diseases. These days, milk consumption in this country has dropped sharply. Following this, the incidence statistics went down. And N. G. Druzyak received a letter of gratitude from the President of Finland Urho Kalevo Kekkonen for raising the problem of excess calcium consumption. Similar events occurred in the United States: a 40% reduction in milk consumption led to a decrease in cardiovascular and some other diseases. But in Japan, everything happened exactly the opposite: in the post-war period, dairy products began to make up a significant share on the Japanese table, and cardiovascular diseases came first.
Sensation!
The scientist noted that almost all centenarians have such traits as sociability, liveliness, curiosity, shallow experiences, the ability to easily change emotions and maintain calm and self-control in any situation. They are characterized by later puberty, normal sexuality and long-term preservation of reproductive function. While people living in areas with high calcium levels in water were noted to have excessive nervousness, irritability, early puberty, and hypersexuality. Based on his observations, N. G. Druzyak made sensational statements:
- increased calcium intake (from water, food, calcium supplements) leads to disease and premature aging and, ultimately, to a shortened life;
- healthy nerves and good character - consequences of low calcium levels in the blood;
— the physiological need for calcium is about 400 mg/day;
— a person’s main concern should not be the regular provision of calcium to the body, but the utmost limitation of its intake into the body , which is much more difficult to do, since most of us live in regions with a high calcium content in natural waters and foods.
Classification
According to the current, chronic and acute hypercalcemia (hypercalcemic crisis) are distinguished. Based on the level of cation (in mmol/l), the following degrees of severity of hypercalcemia are distinguished:
- Easy.
The content of total Ca is less than 3, ionized Ca is less than 1.5. - Moderate.
The level of total Ca is up to 3.5, ionized - up to 1.8. - Heavy.
Total Ca is above 3.5, ionized Ca is more than 1.8.
Pseudohypercalcemia is considered separately. Part of the calcium binds to plasma proteins, therefore diseases such as paraproteinemic hemoblastoses (multiple myeloma), characterized by a high protein content in the blood, are accompanied by an increase in the level of total calcium. Determination of ionized calcium helps to exclude false hypercalcemia.
Symptoms of hypercalcemia
With a mild degree of pathology, there may be no symptoms at all. In moderate to severe cases, muscle weakness appears, sometimes reaching such severity that it is difficult for the patient to get out of bed. Symptoms from the gastrointestinal tract are typical - nausea, vomiting and abdominal pain. Appetite decreases significantly and constipation occurs. Cardiac symptoms (increased blood pressure, tachycardia) are often observed.
Even with hypercalcemia of non-oncological origin due to anorexia and muscular dystrophy, the patient loses a lot of weight, acquires a cachectic appearance, which may give a false impression that he has a malignant neoplasm. The weakening of the effect of antidiuretic hormone on the kidneys causes the appearance of symptoms such as severe thirst, an increase in urine output to 5-6 liters per day.
Neuropsychological symptoms are especially clearly presented. First, emotional instability, impaired concentration, and slight drowsiness occur. In severe cases of pathology, confusion, delirium, and psychosis develop. Hallucinations are possible. With long-term high levels of calcium, it begins to be deposited in the tissues of the joints (chondrocalcinosis), which causes arthralgia.
Complications
Hypercalcemia has a wide range of adverse effects. The most common complications are osteoporosis (due to increased release of calcium ions from bones), pathological fractures, and urolithiasis. Acute pancreatitis and intestinal obstruction occur less frequently. The most life-threatening condition is considered to be hypercalcemic crisis, in which mortality reaches 60%. The cause of death is heart or kidney failure.
Another severe but rare complication is calciphylaxis (calcifying uremic arteriolopathy), characterized by ischemic necrosis of the skin and subcutaneous fat. It develops in patients with end-stage renal failure. A prolonged increase in calcium in the blood can also lead to band keratopathy, calcification of the aorta and heart valves with the formation of heart defects.
Indications for the study
Blood test for calcium
is prescribed in the following cases:
- planned preventive examination;
- kidney pathologies (in patients with such diseases, the level of macronutrients is often reduced);
- suspicion of excess Ca (in the presence of symptoms such as nausea, loss of appetite, weakness, excessive thirst);
- frequent muscle cramps;
- diseases that are associated with calcium metabolism disorders (oncology, thyroid pathologies, etc.);
- some abnormalities detected on the cardiogram;
- symptoms of macronutrient deficiency (hand tremors, muscle cramps, spastic abdominal pain);
- treatment of calcium metabolism disorders.
Diagnostics
The profile of a medical specialist supervising a patient with this pathology is determined by the cause that caused this condition. Most often, such patients are seen by endocrinologists, nephrologists, and oncologists. When interviewing the patient, it is necessary to clarify what medications he is taking. During the examination, the doctor pays attention to symptoms such as decreased muscle tone and suppressed tendon reflexes. An additional examination is prescribed, including:
- Laboratory research.
A biochemical blood test measures the level of albumin, urea, and creatinine. Of the electrolytes, in addition to total and ionized Ca, the concentration of phosphorus and chlorides is determined. The content of vitamin D (25OH-D) is studied. PTH, PTH-like peptides. Daily urinary Ca excretion is checked. If thyrotoxicosis or hypocortisolism is suspected, a blood test for hormones (TSH, free T4, cortisol) is performed. - Functional tests.
Special provoking tests provide invaluable assistance for differential diagnosis of the causes of this disorder. These include tests with native vitamin D, thiazide diuretics, and calcitonin. A steroid suppression test with prednisolone can be used to exclude a process not associated with increased PTH secretion. - Instrumental research.
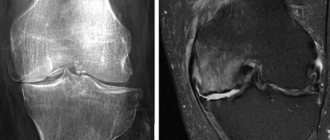
To search for adenoma or hyperplasia of the parathyroid glands, ultrasound, computed tomography, and scintigraphy are performed. Densitometry is performed to determine bone mineral density, and renal ultrasound is performed to diagnose nephrolithiasis. If there are symptoms that raise suspicion of an inflammatory process in the lungs or a malignant neoplasm, radiography, CT scan of the lungs, abdominal organs, and mammography should be prescribed to identify them.
Differential diagnosis must be made based on the predominant symptoms. Insipidal syndrome must be differentiated from diabetes mellitus and diabetes insipidus. Muscle weakness and hypotension should be distinguished from that with muscular dystrophies, myasthenia gravis, and polymyositis. Neuropsychiatric symptoms require the exclusion of psychiatric diseases.
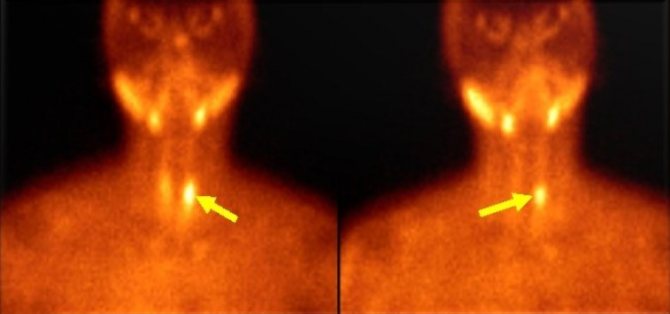
Scintigraphy. Parathyroid adenoma
general characteristics
General calcium is the most important macroelement involved in the formation of bone tissue, teeth, contraction of muscles and heart muscles, stimulates the secretion of hormones, regulates the secretory activity of the stomach, is “Factor IV” of blood coagulation, has an anti-inflammatory and desensitizing effect, is in biological antagonism with ions sodium and potassium. In the blood serum it is represented by three main fractions: bound to serum protein (about 40%), in complex with phosphate and citrate (about 15%), the remaining part is free, not bound to proteins (ionized-active, see “Ionized calcium ", Ca++). Parathyroid hormone, calcitonin and vitamin D are the main calcium-regulating hormones. Excess glucocorticosteroids suppress the activity of osteoblasts, and thyroid hormones stimulate bone resorption. Hypothyroidism interferes with the bone mobilizing effect of parathyroid hormone, leading to secondary hyperparathyroidism. Insulin stimulates osteoblastic collagen production and directly reduces renal reabsorption of calcium and sodium. Phosphorus increases the synthesis of parathyroid hormone (which reduces the level of calcium in the urine) and has a direct effect on the renal tubular transport of calcium. Changes in urinary calcium levels are usually accompanied by changes in sodium levels. These two elements jointly participate in reabsorption mechanisms in the proximal tubule. Caffeine increases urinary calcium loss. A decrease in estrogen levels in postmenopausal women is a major factor in the development of bone resorption and osteoporosis. Testosterone inhibits bone resorption. Digested carbohydrates and protein have a calciuretic effect (for every additional 50 g of dietary protein, 60 mg of calcium is lost in the urine; therefore, a protein-rich diet in adults leads to a negative calcium balance). The acid-base state (ABS) is very important. The influence of the level of serum albumin on the indicators of total calcium:• 44% of calcium is contained in the form associated with serum albumin• fluctuations in the level of serum albumin affect the determined Ca indicators; when assessing the level of total calcium, it is necessary to correct the results obtained taking into account the level of serum albumin (Ca (adjusted ) = total Ca + 0.02 x (40 – patient’s albumin level).
Treatment of hypercalcemia
Conservative therapy
Patients with any degree of severity should be hospitalized in a hospital (endocrinology, nephrology department) for treatment. Patients with severe neurological symptoms and hypercalcemic crisis should be transferred to the intensive care unit. It is necessary to discontinue all medications that can cause an increase in calcium levels. Treatment of hypercalcemia has the following directions:
- Increased excretion of calcium in urine.
First, it is necessary to ensure adequate rehydration with physiological NaCl solution (0.9%). This will improve renal perfusion and increase the filtration of calcium ions by the renal glomeruli. Additionally, forced diuresis is performed using loop diuretics (furosemide). It is necessary to constantly monitor blood electrolyte levels. - Decreased absorption of Ca in the intestine.
Sodium or potassium phosphate salts are well suited for this purpose. Phosphates are strictly contraindicated for the treatment of secondary hyperparathyroidism caused by renal failure. Also, glucocorticosteroids (prednisolone, hydrocortisone) and synthetic antimalarial drugs (hydroxychloroquine, chloroquine) are used to suppress Ca absorption in the gastrointestinal tract. - Suppression of bone resorption.
An important stage in the treatment of hypercalcemia caused by hyperparathyroidism or cancer. The most effective drugs for preventing the progression of osteoporosis are bisphosphonates (pamidronic acid, zoledronic acid), which inhibit the activity of osteoclasts. The peptide hormone calcitonin and the cytotoxic antibiotic mithramycin have a similar mechanism of action, but a faster effect. - Suppression of the production of PTH and PTH-like protein.
For the pathogenetic treatment of primary and secondary hyperparathyroidism, calcimimetics (cinacalcet) are used, which increase the sensitivity of PTG cell receptors, thereby reducing PTH production. Gallium nitrate is used to treat hypercalcemia caused by a malignant tumor, which inhibits the secretion of PTH-like protein by tumor cells. - Intensive therapy.
For the treatment of severe life-threatening conditions (hypercalcemic crisis, calciphylaxis), as well as when other conservative methods of therapy are ineffective, hemodialysis using a low-calcium dialysate solution is an emergency measure to reduce Ca in the serum.
Surgery
Surgical removal of the parathyroid glands is the main treatment for primary hyperparathyroidism. The main indication for surgical intervention is a Ca level above 2.75 mmol/l. To prevent postoperative hypocalcemia (“hungry bone syndrome”), the patient is prescribed vitamin D and calcium supplements. Malignant tumors also need to be removed. To treat oncohematological pathologies, bone marrow transplantation is performed.
Experimental treatment
New drugs are currently being developed to treat this condition. The drug osteoprotegerin, which is a cytokine from the family of tumor necrosis factors, is at the stage of clinical trials. It inhibits the differentiation of osteoclasts and stimulates their apoptosis. In in vitro experiments, the calcitriol analogue EB 1089 suppressed the expression of the PTH peptide gene.
How to reduce calcium in the blood? Treatment of hypercalcemia
How to reduce calcium in the blood? It’s a pity that we can’t get rid of calcium deposits in blood vessels as quickly as we can get rid of scale in a kettle. With the human body, everything is much more serious. Treatment of hypercalcemia depends on its cause and form (degree). General recommendations include:
- exclusion of drugs that simultaneously contain calcium and vitamin D (that is, they should be used when it is necessary to heal a fracture, or with an advanced degree of osteoporosis, after weighing the risks);
- limiting the consumption of foods high in calcium (milk, dairy products, eggs, hard cheese, cabbage, parsley);
- drinking soft drinking water (water filters can be used) with low calcium content, boiled or distilled water (no more than 2 months);
- use of “Fitin” (medicine, a mixture of calcium and magnesium salts, obtained from fat-free hemp and other cakes), oxalic acid (an organic compound found in sorrel, tinder fungi), ballast substances (components of plant foods that cannot be digested in the human body - dietary fiber), which reduces the absorption of calcium in the intestine;
- drinking plenty of fluids in combination with taking diuretics (Furosemide, Torsemide, Hypotheazid, in the absence of renal or heart failure) to increase calcium excretion in the urine;
- the use of procedures with infusions and decoctions of medicinal herbs.
With a slight increase in calcium in the blood, such measures are usually sufficient.
In severe cases of hypercalcemia, the following is used:
- intravenous administration of fluid (saline);
— dialysis (therapeutic hardware procedure for purifying blood from metabolic products);
- removal of tissue from one or more parathyroid glands (a person has 2-8 in total);
- prescribe corticosteroids, bisphosphonates, calcitonin to preserve calcium in the bones and inhibit the processes of bone tissue destruction.
In most cases, hypercalcemia is the result of serious disturbances in the functioning of the body. Therefore, in addition to normalizing the level of calcium in the blood, it is important to find the root cause of this condition and eliminate it.
Prognosis and prevention
Hypercalcemia is a severe and in some cases (especially in acute cases) a life-threatening pathological condition. In hypercalcemic crisis, the mortality rate is very high (60%). The frequency of deaths in chronic cases averages 20-25%. However, the prognosis is largely determined by the cause of the increase in Ca levels.
Prevention of this pathology consists in timely diagnosis and proper treatment of the diseases against which it develops. Before starting to take vitamin D or other medications that may increase Ca levels in the blood, a blood test should be performed to assess Ca levels.
Is there enough calcium in the body?
Is there enough calcium in the body? In most regions of our country, the water is quite hard, that is, the calcium content in it exceeds 20 mg/l. Proof? What about scale on the surfaces of taps and ceramic tiles? What about unpleasant deposits on dishes? What about stains on linen after ironing? And what about the breakdowns of washing machines and dishwashers, which the same advertising offers us to prevent with the help of special strong chemicals? The culprit of all these troubles is calcium carbonate salt (CaCO3), which, when heated, turns into a practically insoluble mineral compound.
Every sip of water we drink contains calcium salts in varying quantities. They quickly and easily enter the bloodstream, being absorbed through the walls of the stomach. How much water do doctors recommend drinking per day? That's right, 2 - 2.5 liters.
This amount already enriches our body with 140 - 180 mg of calcium (with an average calcium content of 70 mg/l; the maximum permissible concentration of calcium, according to the standards for the physiological usefulness of drinking water according to SanPiN 2.1.4.1116-02. “Drinking water. Hygienic requirements to the quality of water packaged in containers. Quality control "is in the range of 25 - 130 mg/dm3, which corresponds to 25 - 130 mg/l). But we also get macronutrients from food.
One liter of low-fat milk contains 1200 mg of calcium (and all of it is completely absorbed!). And according to statistics, in Moscow one person drinks on average 820 ml of this drink per day. 100 g of Dutch cheese already contains 1000 mg of calcium, and 100 g of sesame seeds (remember that sprinkle on buns?) - as much as 1474 mg! As a result, the total consumption of the mineral only with food and water can amount to double the daily requirement, and yet many, trusting advertising calls, additionally take calcium-containing preparations. Is not it too much? And note: scientists have not yet recorded a SINGLE CASE of calcium deficiency in the body of people eating exclusively plant foods.
The absorption of calcium in the body is a very complex and responsible process. After all, it is important not just to absorb calcium, but to absorb the amount of it that the body needs to ensure its normal functioning - no more, no less.