For the normal functioning of each organism, it is necessary to maintain the constancy of its internal environment. This is ensured by all organs and systems: excretory, cardiovascular, respiratory and others.
In turn, for all this to work smoothly, sufficient levels of oxygen and nutrients are necessary. This is provided to us by the most important substance of our body - blood.
Blood is a tissue, and, like all tissues, it is multicomponent. It consists of cells (formed elements) and liquid (plasma). Cells perform very important functions: transporting oxygen, providing an immune response, etc. But plasma, which maintains the necessary consistency of our blood, has an equally important function.
Plasma is the basis of the coagulation and anticoagulation systems, which must be in perfect balance.
The most important cog in this mechanism is a complex plasma protein - prothrombin, which is formed in the liver under the influence of vitamin K and its amount affects blood clotting, as well as the risk of bleeding or thrombosis.
To determine it, a special study is carried out - a blood coagulogram. Indirectly, prothrombin levels can be monitored based on the following indicators:
- Prothrombin index (PTI) is the ratio of the patient’s plasma clotting time to the plasma clotting time of a healthy person of the same gender and age, expressed as a percentage. Normal values are 80-100%.
- Prothrombin time (PTT) - shows how long the plasma will clot in seconds with a special reagent added to it (thromboplastin-calcium mixture) (normally 11-16 seconds).
- International normalized ratio (INR).
- Quick prothrombin level is the ratio of plasma activity compared to the clotting time in the control sample. The normal value is 78-142%.
Of all the above values, the most objective is the international normalized ratio. It is worth noting that this is a standard for determining the state of the blood coagulation system, which does not depend on the method of determining prothrombin time and the sensitivity of reagents used in laboratories.
What is INR
INR (International Normalized Ratio) is a calculated value, an absolute number showing the ratio of a patient's prothrombin time to its standard value (that is, the prothrombin time of a healthy person), reduced to the value of the International Thromboplastin Sensitivity Index (ISI).
What is MIC?
This is the tissue factor activity in the reagent, which is indicated by the manufacturer on each package. INR shows how many times the patient’s blood clotting is changed in comparison with the norm. For example, INR 2.3 means that blood clots 2.3 times worse.
Blood INR: measurement, interpretation, norms
Many people hear the blood INR indicator. What does it mean? Why do doctors pay so much attention to him? How important is the determination of blood INR in medical practice? Read about this in our article.
What is blood INR?
The abbreviation INR blood stands for International Normalized Ratio . However, for a person not involved in medicine, this is an empty phrase. To understand the essence of blood INR and its role in the body, you need to take a short excursion into the physiology of the circulatory system.
The liquid state of blood in the human body is ensured by the coordinated work of the coagulation and anticoagulation systems. Fluidity, an important property of blood, is ensured by the anticoagulant system, and during bleeding, clotting ability becomes important. If the functioning of these systems is disrupted, a person experiences increased bleeding (for example, constant bleeding of the gums when brushing teeth, frequent nosebleeds) or a tendency to thrombosis - the formation of blood clots that can “pass” through vessels of larger diameter and “get stuck” in vessels of smaller diameter diameter It is dangerous when they enter the vessels of the heart and brain, because in these cases they lead to heart attacks and strokes and, as a result, to disability.
Normally, a healthy person is in a state of slight hypercoagulation, i.e. in a healthy body there is a slightly increased functioning of the coagulation system. However, in the absence of diseases, this feature does not lead to acute vascular accidents (heart attacks and strokes). In the presence of certain diseases (and first of all, the very common atrial fibrillation), the already existing tendency to thrombus formation sharply increases. Doctors have long noticed this feature, therefore, if a person has diseases accompanied by increased thrombus formation, they prescribe antithrombotic therapy (anticoagulants and antiplatelet agents) to prevent heart attacks and strokes. I would like to emphasize that these drugs are prescribed strictly by a doctor, since if used independently and uncontrolled, they can have serious life-threatening consequences. The severity of the effects of these drugs is closely related to the concept of blood INR.
Since antithrombotic drugs thin the blood by preventing blood clots, it is extremely important to monitor blood counts that reflect “how thin” the blood is. The main indicator is blood INR. The widely used indicators PTT (prothrombin time) and PTI (prothrombin index) are slowly receding into the background, because the method for determining these indicators involves the use of each specific laboratory with its own reagent with individual sensitivity. Therefore, results may vary greatly between laboratories. The APTT (activated partial thromboplastin time) indicator is determined during treatment with heparin (strictly in hospital conditions). The blood INR indicator was introduced into medical practice in order to somehow standardize the indicators of the blood coagulation system. It is not for nothing that the abbreviation INR blood stands for international normalized ratio.
The most common antithrombotic drug prescribed by doctors is warfarin. This is a well-studied medicine with an extensive evidence base. But it is precisely when using warfarin that it is so important to determine the blood INR. The normal range of blood INR values during warfarin treatment is 2.0-3.0. If the blood INR is less than 2.0, then the risk of ischemic stroke increases, but if the blood INR is more than 3.0, the risk of cerebral hemorrhage increases. The graph below clearly shows within which blood INR values the risks of dangerous complications are minimal (the so-called “therapeutic window”).
What should be a normal INR level?
In adults, the norm is within 0.8 – 1.3. The norm is no different for women and men. But in pregnant women there may be a slight shift in both directions, therefore during pregnancy, INR monitoring should be carried out at least once a trimester, and more often if indicated.
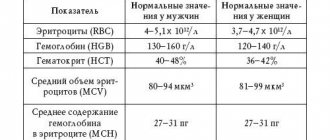
The table below shows normal INR values for various conditions.
Table No. 1: INR decoding: norm (how much it should be) for various conditions.
| Healthy people of both sexes | Pregnant women | Patients taking direct anticoagulants (heparin) | Patients taking indirect anticoagulants (warfarin) | Patients with prosthetic heart valves |
| 0.8 – 1.3 | 0.8 – 1.2 | 0.8 – 1.3 | 2.0 – 3.0 | 2.5 – 3.5 |
Complexes with this research
Preventive check-up Universal annual preventive screening RUR 11,960 Composition
Female infertility Analysis of women's reproductive health status RUR 16,210 Composition
Examination during pregnancy. 3 trimester 9 620 RUR Composition
IN OTHER COMPLEXES
- Men's check-up No. 1 RUB 18,570
- Risk of severe COVID-19 RUB 1,090
- For those at risk of COVID-19 RUB 4,510
- Pregnancy planning. Clinical indicators 6,630 R
- Expanded hospital complex 7,700 RUR
In what situations is this examination prescribed?
This examination is prescribed during treatment with indirect anticoagulants - vitamin K antagonists (neodicoumarin, warfarin, syncumar), which reduce the level of prothrombin in the blood, thus thinning it.
Regular monitoring of the indicator allows you to control the dosages of the above drugs to avoid bleeding or blood clots.
When is it necessary to take indirect anticoagulants?
In what situations is it necessary to regularly take a blood test for INR and prothrombin?
- Treatment and prevention of thrombosis of the superficial and deep veins of the lower extremities;
- Varicose veins;
- Acute coronary syndrome;
- Cerebrovascular accident in the acute stage (ACVA);
- PE (pulmonary embolism);
- Permanent form of atrial fibrillation;
- Heart disease;
- Thrombophlebitis;
- The presence of artificial valves in the heart;
- The presence of a vena cava filter (a filter in a large vein of the body that prevents thrombotic masses from entering the veins of the lower extremities and pelvic organs to the heart and lungs.
It must be remembered that when using warfarin and other anticoagulants, the INR level is increased and should be kept within 2.0 - 3.0 (the optimal value is 2.5), and with prosthetic heart valves from 2.5 to 3.5. Patients with an INR value above 6.0 require urgent treatment.
If a person is not treated with anticoagulants, then a deviation of the INR from the norm can cause serious pathological changes in the body. Let's consider in what situations the level of this indicator may change.
Where can I get the analysis done?
There are several options for donating blood to determine INR levels:
- in a private laboratory, having received a referral from a local physician or family doctor;
- directly in the therapist’s office if the necessary equipment is available;
- independently at home using a special device.
The latter option is convenient for people who need to regularly measure their INR. For example, for patients with hemophilia or patients taking Warfarin and other anticoagulants. The portable device is very easy to use. Using a special device, a puncture is made in the skin and blood is applied to the test strip. The strip is inserted into the machine, and the result appears on the display almost immediately.
According to the recommendations of the World Health Organization, an INR blood test should be performed in all patients taking drugs that affect blood clotting. And also for those who suffer from congenital and acquired clotting diseases.
Elevated INR level
If the INR is elevated, this indicates the following problems:
- liver diseases (cirrhosis, fatty degeneration, chronic hepatitis, toxic damage);
- disruption of vitamin K synthesis in the body;
- lack of certain plasma proteins;
- DIC syndrome;
- congenital deficiency of coagulation factors;
- diseases of the stomach and intestines, in which the absorption and breakdown of fats is impaired;
- massive blood transfusion.
An INR higher than normal is a consequence of decreased blood clotting, the so-called hypocoagulation. This condition may cause bleeding or hemorrhage.
Massive external bleeding can occur with a slight violation of the integrity of the skin (abrasion, scratch), and internal bleeding most often develops against the background of an existing disease (for example, gastric - with a stomach ulcer, uterine - with uterine fibroids).
Such conditions require immediate hospitalization of the patient and correction of the impaired coagulation system.
Testimony and transcript
The most common indications for an INR test are:
- Examination before surgery. In this case, the INR norm is in the range of 0.85-1.25 units.
- Treatment of pulmonary embolism. The normal INR value in this case ranges from 2 to 3 units.
- Treatment of chronic atrial fibrillation with Warfarin. The INR ranges from 2 to 3 units.
- Heart valve defects. The normal INR for these pathologies is considered to be 2-3 units.
- Therapy of venous thrombosis. The normal INR value for venous thrombosis is 2-3 units.
- Vascular diseases. In these diseases, the INR ranges from 3 to 4.5 units.
Increased values
According to medical specialists, going beyond the above indicators is extremely undesirable, and even dangerous. An increase in INR when using Warfarin (or its analogues) indicates a decrease in coagulation, which can lead to both external and internal (uterine, abdominal, gastric) bleeding.
If the international normalized ratio increases, doctors usually resort to reducing the dosage of indirect anticoagulants. When the INR level decreases, medical specialists increase the dose of these medications due to the ineffectiveness of therapy.
An INR value exceeding 1.25 units in people who do not take anticoagulants can lead to pathologies such as:
- myocardial infarction;
- liver diseases;
- pre-infarction condition;
- polycythemia;
- malignant tumors;
- impaired absorption of lipids in the intestine;
- hemorrhagic disease in infants;
- problems with bile entering the duodenum from the liver.
If a patient’s international normalized ratio exceeds 6 units, then he needs urgent hospitalization, due to the high risk of bleeding of various locations. This condition is considered extremely dangerous if a person has concomitant illnesses such as arterial hypertension, kidney pathologies, ulcerative or inflammatory diseases of the intestines and stomach.
Decreased INR level
There is also the opposite condition - hypercoagulation, in which the blood thickens. This condition is dangerous due to blood clots that can block blood vessels leading to vital organs.
Then such severe conditions as pulmonary embolism (thromboembolism), myocardial, kidney, spleen, intestinal infarction, acute ischemic cerebrovascular accident occur.
Typically, INR levels decrease when:
- dehydration of the body (rapid loss of fluid without its replenishment) - when taking diuretics, burns, impaired permeability of the walls of blood vessels, when fluid leaks out of them into the surrounding tissues, and cellular elements remain in the channel;
- hereditary deficiency of antithrombin III;
- when taking hormonal drugs (especially oral contraceptives);
- infectious diseases accompanied by a significant increase in temperature;
- malignant neoplasms;
Also, indicators may be low due to technical errors during blood sampling or analysis.
Monitoring anticoagulant therapy using INR
Answering the question of what a blood test for INR shows, it is worth saying that this is an effective method for monitoring therapy with anticoagulants and antiplatelet agents. These two groups of drugs thin the blood. Therefore, it is necessary to constantly monitor the state of the blood coagulation system to prevent the development of severe bleeding. This is especially true for treatment with such drugs:
- "Heparin";
- "Warfarin";
- "Sinkumar";
- "Finilin."
Anticoagulants are prescribed to people with a tendency to excessive blood viscosity, with an increased risk of thrombosis (myocardial infarction and stroke, congenital and acquired heart defects, history of pulmonary embolism, varicose veins, thrombophlebitis).
How to take an INR test
Patients undergoing treatment with indirect anticoagulants in a hospital setting undergo an INR test according to the following scheme:
- At the beginning, control is carried out on days 3-4;
- then 2-3 times a week until the desired results are achieved.
It should be remembered that discharge from the hospital is not a reason to discontinue anticoagulant drugs (they are taken for life), then an INR blood test must be taken every 6-8 weeks at first.
If the patient is able, he can come to the laboratory of the clinic at his place of residence or to a private institution and get tested.
Blood is taken from a vein, which is the most optimal and correct, but can be technically difficult in patients with poor veins (obese, receiving chemotherapy, with scars on the skin of the forearms and hands, etc.).
If it was not possible to obtain a sample from a vein, then blood is taken from a finger using a scarifier.
Technique and frequency of analysis
The INR level is determined in blood from a peripheral vein. The sampling is done with a disposable, sterile syringe. Before the injection, the skin is treated with an antiseptic solution. A tourniquet is applied to the forearm, and the nurse carefully draws blood into a syringe. Next, the blood is sent to the laboratory for analysis.
For patients taking anticoagulants or antiplatelet agents, the test is done once every two to three weeks. The frequency is selected individually, depending on the severity of the disease and its duration. Patients with a well-chosen treatment regimen can undergo analysis once a month.
Preparing for INR tests
Prepare for the analysis as follows:
- Before taking the test, it is necessary to discontinue medications regularly taken to treat concomitant pathologies;
- the day before the test, avoid fatty foods;
- three days before the test, give up all types of alcohol;
- It is better to donate blood in the morning on an empty stomach;
- Women are not recommended to donate blood during menstruation.
But, like all rules, there are exceptions. The above restrictions do not matter in an emergency situation when a person's life is at stake. In such situations, the INR blood test is performed urgently without preparation, and after a while the test is repeated again.
It is also possible to monitor your home at any time using a special device, knowing what the INR norm is. Measurements are taken at the same time, preferably in the morning.
It is recommended to keep a diary recording your results.
The device used to measure INR is convenient and compact; the result will be ready in a matter of minutes.
The only drawback is the rather high price. Such measures are necessary only at the beginning of a course of anticoagulant therapy in order to select the most optimal dosage of the drug. In the future, after achieving the required INR level, its monitoring must be carried out according to indications.
Table of INR norms for women by age
It should be noted that because different laboratories use different reagents, normal values may vary for each laboratory.
In this regard, when interpreting the results of the analysis, one should be guided by the standards indicated on the form with the results.
| The INR norm for women does not depend on age and is: | from 0.85 to 1.35. |
| During pregnancy, INR may decrease: | in the third trimester the norm is from 0.15 to 1.17 |
What are the indications for an emergency test?
- Acute infectious disease (respiratory, intestinal infection).
- Climate change (long-distance and long flights, transfers).
- Changing work and rest schedules, diet, physical activity, taking new medications. It should be noted that when taking new medications or consuming new foods, the INR should not be rechecked immediately, but after 2-3 days. It must be remembered that there is a list of drugs that increase or decrease the effect of warfarin.
- Frequent and prolonged bleeding (nose, gum, menstrual, blood in stool, urine, sputum).
- The appearance of compactions and swelling in the joints.
- Before planned invasive procedures (tooth extraction, gastroscopy)
In conclusion, I would like to say that following simple rules for taking anticoagulants with regular monitoring of INR will save you from unnecessary costs for expensive and inappropriate treatment and severe complications.
Treatment with warfarin
Warfarin is prescribed for treatment and prevention
- venous thrombosis and pulmonary thromboembolism.
- for deep vein thrombosis
- stroke and thromboembolism
- heart valve replacement
- after myocardial infarction
- with rheumatic heart valve disease
- with cardiac anomalies (with an open foramen ovale)
- in case of impaired contractile function of the left ventricle
- antiphospholipid syndrome
Long-term use of warfarin can be accompanied by various side effects, so it is important for the doctor to constantly keep the situation under control and monitor the patient’s normal condition in order to change or stop taking the drug in time.
Not all patients can adapt to taking warfarin. No matter what they tell you, if you feel unwell, be sure to ask your doctor to change your medication.
Warfarin is not always taken for life; in some diseases it is discontinued after 4-6 months. Sometimes warfarin is replaced with alternative drugs Pradaxa, Xarelto and others.