What are uterine fibroids?
To begin with, a woman should know the most important thing: uterine fibroids, although a tumor, are benign and not at all cancerous. It develops in the walls of the uterus itself or its cervix, and ranges in size from a couple of millimeters to several centimeters. The size of fibroids is assessed by gynecologists similar to the size of the uterus during pregnancy, i.e. four, five, twelve weeks and beyond.
The location of uterine fibroids determines its classification:
- Subserous fibroids - the nodes are located on the outside of the uterus;
- Interstitial fibroids (intramuscular) - the tumor is located directly in the muscular walls of the uterus;
- Submucosal fibroids (submucosal) - a neoplasm grows in the uterine cavity, under its mucous membrane.
It should be noted that pedunculated fibroids are not a separate type of this disease, since fibroids can have a pedicle in both the first and third cases, only differ in width.
Diagnostics
Diagnosis of cervical fibroids is carried out in stages. The first thing the doctor will do is examine the patient’s complaints, determine the time of their appearance and the possible cause, and assess the degree of progression of the disease according to the woman. The next step is an examination in a gynecological chair. During the examination, the doctor assesses the position and size of the woman’s reproductive system organs, their shape, mobility, and pain. An obligatory part is examining the cervix in a speculum and taking smears for flora. After examination and making a preliminary diagnosis, the doctor draws up a plan for an instrumental examination.
As a rule, it includes:
- Ultrasound diagnostics. With the help of ultrasound, the gynecologist is able to identify fibroids, determine their size and exact location.
- Diagnostic curettage. Diagnostic curettage is necessary to exclude pathological changes in the endometrium and timely diagnosis of malignant diseases.
- Hysterography. Hysterography is an X-ray examination with which the doctor can assess the size and shape of the uterine cavity.
- Hysteroscopy. Hysteroscopy is an endoscopic examination method, thanks to which the gynecologist can directly examine the uterine mucosa. The method is necessary for diagnosing polyps, uterine fibroids and other neoplasms. During hysteroscopy, the doctor may perform a biopsy—sampling a small piece of tissue from suspicious areas. The resulting material is sent for pathomorphological examination.
- Laparoscopy. Laparoscopy is a minimally invasive diagnostic and therapeutic procedure (more details). During laparoscopy, the surgeon inserts a laparoscope into the abdominal cavity through small incisions. The device is equipped with a lighting device and a video camera, thanks to which the doctor can see the internal organs on the monitor screen and assess their condition and perform a biopsy.
- Study of a woman's hormonal background.
Having the results of additional studies in hand, the gynecologist can develop a treatment plan for fibroids.
Causes of uterine fibroids in women
There are many reasons why a woman develops uterine fibroids. But the main one is considered to be hormonal imbalance. That is why fibroids are a diagnosis for women of childbearing age, and they may well fade away with the onset of menopause.
But not only hormonal imbalance can provoke uterine fibroids; the reasons for its appearance can be different. Here are some of them:
- genetic (hereditary) predisposition;
- metabolic disorders (obesity, diabetes, chronic diseases);
- adenomyosis;
- menstrual irregularities;
- intrauterine devices;
- prolonged stress;
- numerous terminations of pregnancy, that is, abortions;
- lack of orgasm during sexual intercourse.
Now let's talk in more detail about some of the causes of uterine fibroids.
Excess estrogen, lack of progesterone
Since uterine fibroids are a hormone-dependent tumor, they do not occur in girls who have not yet started menstruation and in women after menopause. The uterus feeds on female sex hormones (estrogen), and when their regulation is disrupted, i.e. their level increases, fibroids begin to grow. It is also known that it is not so much the high level of estrogen that provokes the growth of pathology, but rather their imbalance. But these changes can only be determined through a series of special hormone tests.
Number of pregnancies, births, abortions
To accurately determine a woman’s hormonal status, the doctor collects a detailed medical history. Many factors play a decisive role in the formation of hormonal levels, such as:
- at what age did menstruation begin?
- number of full-term pregnancies and abortions;
- was there lactation after childbirth, and how long did it last, etc.
If a woman has given birth to at least one child, the risk of fibroids is much reduced.
Women's nutrition
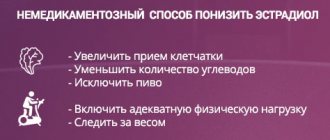
The level of estrogen in a woman’s body directly depends on how she eats. If the daily menu includes a lot of refined and fatty foods, and there is practically no fiber in it, then this can lead to an increase in estrogen. In addition, such a diet is fraught with extra pounds, which means that women who are overweight and obese have a much higher chance of getting uterine fibroids than slim women. It is also known for certain that a vegetarian diet, which mainly consists of nuts, fruits, vegetables, cereals and other low-fat foods, significantly reduces the risk of developing uterine fibroids.
Lack of orgasm during sexual intercourse
It's no secret that some women do not experience orgasm during sex, and this can have very unpleasant consequences for her health. The fact is that arousal causes a rush of blood to the genitals, and if satisfaction does not occur, then it does not go anywhere and stagnates in the pelvis. And this, in turn, provokes tension in the veins and vessels of the genital organs, and, as a result, hormonal imbalance and the growth of fibroids.
Symptoms of uterine fibroids
A woman may not even know that she has uterine fibroids, since in most cases this disease occurs without any symptoms. Here everything depends on the size of the nodes: if they are small, then the woman will find out her diagnosis only during a scheduled visit to the gynecologist; if they are large, then the symptoms of uterine fibroids will definitely be present.
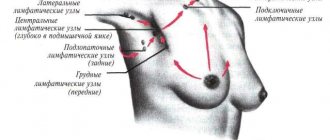
So what signs can tell a woman that she may be developing uterine fibroids? A consultation and examination by a gynecologist is required if a woman’s menstrual cycle is disrupted, her periods become irregular, heavy and painful, and bleeding or spotting may appear in the middle of the cycle. Heavy menstrual flow often causes anemia, and this leads to the fact that a woman begins to get tired quickly and is in a drowsy state all the time. Sharp pain appears in the groin and pelvic area.
If the fibroid is subserous, i.e. located outside the uterus, it can put pressure on neighboring organs - the bladder and intestines. In this case, the woman will experience frequent urination and constipation. With internal fibroids, infertility or spontaneous miscarriages can develop.
Symptoms and complications
In half of the cases, uterine fibroids are asymptomatic if small nodes are localized subperitoneally or intermuscularly. Submucosal nodes almost always give symptoms, perhaps except for the initial stage of the disease, when the tumor is still too small, which can only be detected during a physical examination. Treatment carried out at this stage will have the best effect.
The greatest danger is posed by submucous uterine fibroids. Located in the uterine cavity, large submucosal nodes put pressure on its walls and vessels, causing heavy bleeding both during menstruation and outside the cycle. A small submucosal node causes acyclic bleeding that cannot be ignored. If you begin immediate treatment of submucous fibroids at this stage, you can avoid dangerous consequences.
As the submucosal node grows, it can cause the following symptoms:
- menorrhagia (bleeding during menstruation);
- prolonged menstruation;
- discharge of blood clots;
- acyclic bleeding or spotting;
- pulling, cramping or pressing pain in the lower abdomen;
- flatulence, constipation caused by intestinal compression;
- problems with urination (delays, frequent urination) caused by the pressure of submucous fibroids on the bladder;
- discomfort during sex;
- feeling that the stomach is full.
The pain can be periodic or constant, radiating to the lower back. This depends on which direction the submucosal node grows - towards the outer uterine wall (centrifugal growth) or towards the center of the cavity (centripetal growth). The larger the volume of submucous uterine fibroids, the more serious complications can arise. In most cases, the tumor reaches several millimeters or centimeters in size. However, if the symptoms are ignored, the nodes can grow to significant sizes. The medical literature describes a case of a 63-kg leiomyoma. This can happen if you do not pay any attention to your health and do not contact a gynecologist for many years.
The thin stalk of submucous fibroids can twist, which will cause necrotic changes in the pathological focus due to impaired blood supply. This manifests itself as sharp, severe pain and requires urgent surgical treatment. If the disease develops over years and the woman does nothing, then gradually the tumor causes pathological changes in the reproductive sphere and problems with fertility. Therefore, without proper treatment, the tumor can lead to infertility. With prolonged compression of the intestines and bladder, their function is impaired.
During pregnancy, the location of fibroids near the placenta is especially dangerous. This can cause a disruption in the functioning of the placenta, in which it will not be able to fully carry out its functions, namely, deliver oxygen and nutrition to the fetus, and ensure its healthy functioning. In addition, large fibroids produce hormones that can provoke spontaneous miscarriage or premature birth by stimulating myometrial tone.
Is it possible to treat uterine fibroids without surgery?
Naturally, if a woman discovers certain symptoms, she should consult a doctor. After examination and a thorough examination, the gynecologist will decide what treatment needs to be applied - whether it will be conservative treatment or removal of fibroids. The woman’s health status, her age, and desire to have children in the future are also taken into account. In the latter case, the most gentle therapy is selected.
If we are talking about small nodes (less than twelve weeks), which do not increase and do not give serious symptoms, then the doctor can limit the woman to regular examinations every six months and ultrasound examinations, without prescribing any medications. You should also refrain from sunbathing, visiting baths and saunas, and limit physical activity.
If the nodes grow slowly or the fibroids were already diagnosed at medium size, then the doctor prescribes treatment with hormonal drugs that inhibit the growth of estrogen and, in fact, the nodes themselves. With the proper effect, this method of treating uterine fibroids will help avoid surgery to remove it. Usually, combined oral contraceptives are prescribed for these purposes, for example, Mercilon, Novinet, or Rigevidon, Ovidon. Taking these drugs significantly reduces symptoms of uterine fibroids such as bleeding and pain. It is worth noting, however, that drugs in this group do not always help reduce the size of fibroids; they are effective only in cases where initially the nodes were no more than one and a half centimeters.
In other cases, drugs from the group of antiprogestogens - Mifeprestone - are prescribed. It is used both as a therapeutic agent for treatment and as preparation for surgery.
But the most modern, effective and gentle method of treating uterine fibroids today is considered to be FUS ablation. This is not an operation, but a non-invasive method of removing fibroid nodes, which is performed with an ultrasound beam. The doctor directs such a beam only to those places where the tumor is localized and eliminates the nodes themselves. The advantages of this method of treating uterine fibroids are quite obvious:
- with FUS ablation there is no blood loss, no anesthesia is used, and no damage is caused to the organ;
- the reproductive functions of the woman’s body are preserved, the uterus remains intact;
- high efficiency in the treatment of large nodes and multiple fibroids;
- absence of any negative side effects, i.e. no pain, fever, intoxication;
- after the use of FUS ablation, no relapses of the disease were observed;
- rehabilitation and recovery take place in the shortest possible time; the procedure can be performed on an outpatient basis.
Basic principles of non-surgical treatment of uterine fibroids
In order to cure uterine fibroids without surgery, of course, taking hormonal drugs alone is not enough. You need to undergo a full course of conservative treatment. And it includes some additional measures.
If there is a history of sexually transmitted infections, they must be treated. A woman should reconsider her diet, and in the future adhere to a certain diet, namely: as little fatty, fried and flour foods as possible, and more vegetables, fruits, wholesome and healthy foods.
- It is worth thinking about strengthening the immune system by using special means for this.
- It is necessary to normalize metabolism.
- If there are psycho-emotional disorders, you need to undergo a course of sessions with a psychologist or psychotherapist.
- If prolonged periods cause anemia, it is imperative to treat it.
When is hysterectomy surgery indicated?
Now let's look at those cases when surgery to remove the uterus is inevitable.
- The size of the nodes is more than 12 weeks, the tumor puts pressure on nearby organs: bladder, intestines.
- Rapid growth rate of nodes - the size of the uterus increases up to six months of pregnancy in just four weeks or less.
- Due to fibroids, a woman begins to experience severe uterine bleeding.
- The tissues in the myomatous nodes die and become necrotic.
- Necrosis of the node.
- Uterine fibroids and adenomyosis at the same time.
Previously, in the presence of such indications, the only option was complete removal of the uterus (hysterectomy). But the achievements of modern medicine make it possible to perform the most gentle operations, leaving women a chance for a normal life and the opportunity to have children in the future. There are several types of such operations. The most common is myomectomy. With this type of surgery, the doctor tries to directly remove only the fibroid node itself, without injuring the uterus. Myomectomy is performed in three ways, the choice of which depends on the size of the fibroid, its type and location.
Laparoscopic - several small punctures are made in the abdominal wall, through which the nodes are excised.
Hysteroscopic - done using a special instrument that is inserted into the uterus through the vagina.
These two methods of operations for removing nodes are considered the most popular and gentle today. They leave no traces, the woman’s reproductive function is preserved, and recovery after surgery does not take much time.
But when the growth of nodes cannot be stopped by any of the above methods, doctors have to resort to the most extreme and radical measure - hysterectomy, the complete removal of the uterus.
Modern medicine offers women another very delicate and gentle way to treat uterine fibroids - embolization of the uterine arteries. This method is unique in that doctors block blood flow in those vessels that feed the fibroids, the blood supply to the nodes stops and they dissolve.
Classification depending on the number of fibroids
Depending on the number of nodes, there are three types of fibroids:
- Single - 1-2 nodes, which can have different sizes.
- Multiple. More than 3 nodes are detected. Treatment usually helps reduce symptoms, but it is often not possible to remove all fibroids, and some may grow large over time.
- Mixed. There are many fibroids, but at least one of them is large and dominant. For example, multiple fibroids with a large subserous node may be diagnosed. It can be removed, but another node may grow strongly in the future. Multiple and mixed fibroids pose a particularly big problem in women of reproductive age before menopause, since sex hormones promote the growth of nodes.